Abstract
Purpose
Prosthetic-based breast reconstruction is performed with increasing frequency in the United States. Major mastectomy skin flap necrosis is a significant complication with outcomes ranging from poor aesthetic appearance to reconstructive failure. The present study aimed to explore the interactions between intraoperative fill and other risk factors on the incidence of flap necrosis in patients undergoing mastectomy with immediate expander/implant-based reconstruction.
Methods
A retrospective review of 966 consecutive patients (1,409 breasts) who underwent skin or nipple sparing mastectomy with immediate tissue expander reconstruction at a single institution was conducted. Age, body mass index, hypertension, smoking status, premastectomy and postmastectomy radiation, acellular dermal matrix use, and application of the tumescent mastectomy technique were analyzed as potential predictors of flap necrosis both independently and as synergistic variables with high intraoperative fill. The following three measures of interaction were calculated: relative excess risk due to interaction, attributable proportion of risk due to interaction, and synergy index (SI).
Results
Intraoperative tissue expander fill volume was high (≥66.7% of the maximum volume) in 40.9% (576 of 1,409 breasts) of cases. The unadjusted flap necrosis rate was greater in the high intraoperative fill cohort than in the low fill cohort (10.4% vs. 7.1%, p=0.027). Multivariate logistic regression did not identify high intraoperative fill volume as an independent risk factor for flap necrosis (odds ratio 1.442, 95% confidence interval 0.973-2.137, p=0.068). However, four risk factors were identified that interacted significantly with intraoperative fill volume, namely tumescence, age, hypertension, and obesity. The SI, or the departure from additive risks, was largest for tumescence (SI, 25.3), followed by hypertension (SI, 2.39), obesity (SI, 2.28), and age older than 50 years (SI, 1.17).
Immediate prosthetic-based breast reconstruction continues to gain popularity among mastectomy patients [1]. According to the American Society of Plastic Surgeons, more than 78% of the 91,655 breast reconstructions performed in the United States during 2012 involved a tissue expander and/or an implant [2]. Studies investigating the influence of potential risk factors have guided evidence-based decision making, serving to minimize adverse events and to improve patient outcomes within this growing population [3-12]. Risk factors such as smoking, radiation, and obesity have been shown to increase a patient's risk of flap necrosis [3,10-14]. Through similar putative mechanisms, each of these risk factors significantly impairs postoperative blood flow to the native skin, resulting in various degrees of tissue injury. These patient-related risk factors are often beyond the surgeon's control; however, a potential surgical variable is intraoperative expander fill volume. Judicious intraoperative tissue expansion is critical for preserving three-dimensional breast architecture and eliminating dead space. Meanwhile, overfilling of expanders may contribute to the development of perioperative complications, specifically mastectomy flap necrosis, by compressing the microvascular circulation underlying the skin flap [15].
A previous study of intraoperative fill did not find large tissue expander volumes to be independently associated with poor patient outcomes [8]; however, the possibility of a significant interaction between high intraoperative fills and other known risk factors has, to our knowledge, yet to be explored. While an otherwise healthy patient may tolerate high intraoperative fills and recover without postoperative morbidity, a patient with coexisting preoperative or intraoperative risk factors may experience clinically relevant tissue ischemia and flap necrosis. Understanding potentially synergistic interactions between intraoperative fill volume and other risk factors on the development of flap necrosis will allow surgeons to more objectively evaluate a patient's risk. In this single-institution study of more than 1,400 breasts, we aimed to explore the interactions between intraoperative fill volume and other risk factors on flap necrosis rates in patients undergoing mastectomy with immediate expander/implant based reconstruction.
This study was performed under the approval of the Northwestern University Institutional Review Board (approval No. STU00056967). A retrospective review of medical records was performed for 966 consecutive patients (1,409 breasts) who underwent skin- or nipple-sparing mastectomy with immediate tissue expander reconstruction by four surgical oncologists and two reconstructive surgeons (J.K. and N.A.F.) at a single institution between 2004 and 2012.
Demographic information, clinical characteristics, operative factors, follow-up period, and postoperative outcomes were recorded. Patient demographics and clinical characteristics included age, body mass index (BMI), hypertension, smoking status, premastectomy radiation, and postmastectomy radiation. Patients with a recorded history of smoking within 1 month of the operation were deemed smokers. Operative factors included acellular dermal matrix (ADM) use, intraoperative tissue expander fill, and use of the tumescent technique. High intraoperative tissue expander fill was defined as a fill volume greater than 66.7% of the maximum volume. The primary outcome of interest was the occurrence of postoperative mastectomy flap necrosis and included only those cases requiring surgical excision with or without closure. Incidences of flap necrosis are reported per breast.
The mastectomy was performed by an oncologic surgeon, usually through an incision encompassing the nipple-areola complex with a lateral extension for skin-sparing mastectomy or through a lateral inframammary fold incision for nipple-sparing mastectomy. Incisions were jointly planned by the oncologic and reconstructive surgeons. At the discretion of the oncologic surgeon, if the tumescent technique was used, the breast and axillary subcutaneous and deep tissues were infiltrated with tumescent solution consisting of lactated Ringer's containing 1% lidocaine and dilute (1:1,000) epinephrine [16]. Mastectomy then proceeded by sharp dissection. Nontumescent mastectomies were performed in the standard fashion using primarily Bovie electrocautery.
After mastectomy, the pectoralis major was elevated using Bovie electrocautery, taking care to preserve the lateral serratus anterior fascia. The inferior attachments of the pectoralis were completely divided. The medial attachments were partially divided to allow the tissue expander to sit as medially as possible without thinning of the medial tissues. A tissue expander of appropriate base width was chosen and placed into the subpectoral pocket. The lateral border of the pectoralis major was sutured to the serratus anterior fascia to achieve total submuscular coverage of the expander. In cases in which total muscular coverage was not optimal because of violation of the rectus abdominis fascia, serratus anterior fascia, or a tight subpectoral space, ADM was used to assist in coverage of the tissue expander. If ADM was used, it was positioned and secured to the inframammary fold, inferolateral border of the pectoralis, and serratus fascia, if present, at this time. The expander was filled to the point at which the skin laxity was taken up, but the skin was not stretched. Two closed suction drains were placed between the pectoralis and the mastectomy flap, one in the axilla and the other in the inferior pole, and the skin was closed.
Postoperatively, the closed suction drains remained in place until output was less than 30 mL over 24 hours. Oral antibiotic prophylaxis was prescribed until the removal of drains. Serial expansion was started when the incisions had completely healed and was performed at intervals; fill volumes were determined on a per-patient basis. Expansion was delayed if the patient was to undergo adjuvant radiation therapy.
Categorical variables were compared for <66.7% fill versus ≥66.7% fill using Pearson chi-square test, and quantitative variables were compared using Student t-tests. Multivariate logistic regression analysis, adjusting for age, hypertension, BMI, smoking, premastectomy and postmastectomy radiation, tumescence, and ADM use, was used to identify independent risk factors for mastectomy flap necrosis and to examine the effect of a high intraoperative fill.
Chi-square analyses were used to identify unadjusted predictors for flap necrosis within each intraoperative fill group. Logistic regression models were used to adjust for potential confounders and quantitatively assess for synergistic interactions between a high intraoperative fill and those risk factors identified in the unadjusted analysis. As previously described, four exposure categories were created from each pair of dichotomous risk factors, including the three possible combinations of exposure and a fourth reference category [17]. Adjusted odds ratios (ORs) were calculated for each potential risk factor in the absence of the other and for the combination of risk factors relative to those patients who were unexposed to both. Three measures of interaction were calculated, namely the relative excess risk due to interaction (RERI), the attributable proportion (AP) of risk due to interaction, and the synergy index (SI) [17]. The RERI captures the additional, additive risk from the interaction between the two variables (ORBoth-ORHigh Fill-ORSecondary+1). AP standardizes this value as a proportion of the combined effect (RERI/ORBoth). SI is the ratio of the risk of the combined effect (ORBoth-1) to the sum of the individual effects [(ORHigh Fill-1)+(ORsecondary-1)]. All the analyses were performed with SPSS version 21.0 (IBM Corp., Armonk, USA) and p<0.05 considered as significant.
Mastectomy with immediate prosthetic-based reconstruction was performed in 1,409 breasts (966 patients), of which 576 (40.9%) received a high intraoperative tissue expander fill volume (≥66.7% of the maximum volume). The mean±SD follow-up period for all the patients was 21.0±15 months (minimum, 5 months) after expander-implant exchange. Table 1 summarizes the preoperative and intraoperative variables according to fill volume. The patients who received a high intraoperative fill volume tended to have a higher BMI (26.5 kg/m2 vs. 25.0 kg/m2, p<0.001) and to be older (49.0 years vs. 47.8 years, p=0.043) than their low intraoperative fill counterparts. In addition, the high-volume group had a lower rate of active smokers (6.8% vs. 10.3%, p=0.021) and a higher rate of ADM use (49.3% vs. 37.6%, p<0.001). The unadjusted flap necrosis rate was greater in the high intraoperative fill cohort than in the low fill cohort (10.4% vs. 7.1%, p=0.027).
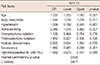
Multivariate logistic regression did not identify high intraoperative fill volume as an independent risk factor (OR, 1.442; 95% confidence interval, 0.973-2.137; p=0.068). Active smoking, age, and BMI were significantly associated with the incidence of flap necrosis (Table 2).
Table 3 compares the unadjusted flap necrosis rate according to intraoperative fill volume stratified by individual risk factors. Among the patients with a low intraoperative fill volume, the rate of flap necrosis differed significantly between smokers and nonsmokers (15.1% vs. 6.2%, p=0.002) and between patients older than 50 years and those 50 years or younger (10.1% vs. 5.3%, p=0.010). Within the high intraoperative fill cohort, flap necrosis rates differed significantly according to the following risk factors: tumescence, age, hypertension, and obesity.
After adjusting for potential confounders, tumescent mastectomy technique, age older than 50 years, hypertension, and obesity showed a statistically significant synergistic interaction with a high intraoperative fill volume with regard to the development of major mastectomy flap necrosis, whereas the individual effects were not significantly associated with an increased risk (Table 4). Table 5 summarizes the synergistic effect of each risk factor on the rate of flap necrosis. The RERI quantifies the extent to which the risk when both factors are present (the joint effect) is greater than the sum of their individual risks; the AP standardizes the RERI as a proportion of the risk of the joint effect. A RERI and AP of 0 suggest no interactions; RERI/AP >0, a positive interaction; and an RERI/AP <0, a negative interaction. The greatest interaction was noted for tumescence and a high fill (RERI=0.925), where nearly half of the risk of the joint effect was attributed to a synergistic interaction (AP, 0.471). The RERI was 0.194 for age older than 50 years (AP, 0.083), 0.631 for hypertension (AP, 0.302), and 0.585 for obesity (AP, 0.286). The SI measures the departure from additive risks; an SI of 2.39 for hypertension suggests that the risk from the synergistic interaction between hypertension and a high fill is 2.4-fold greater than the additive risks of each individual variable. The SI was greatest for tumescence (SI, 25.3), followed by hypertension (SI, 2.39), obesity (SI, 2.28), and age older than 50 (SI, 1.17).
Mastectomy skin flaps are particularly vulnerable to poor circulation and hypoxia, exposing patients to a high risk of postoperative complications, specifically wound breakdown and flap necrosis [14,18-20]. Following immediate prosthetic-based reconstruction, the inflated expander may increase stress on the already tenuous microvascular circulation [8,15]. The rate of flap necrosis in the literature varies greatly from 8.7% to as high as 22%, largely because of differences in definition and surgical technique [8,12,20-22]. Our relatively low observed flap necrosis rate of 8.45% is consistent with our strict definition, which was meant to include only those cases that required surgical excision. Severe mastectomy flap necrosis requiring surgical excision often results in less favorable aesthetic outcomes and in some cases, reconstructive failure. Although high intraoperative fill volume was not an independent risk factor for flap necrosis in either our study or in a previous study by Crosby et al. [8], high expander fill volume may interact synergistically with other risk factors. McCarthy et al. [12] found that individual risk factors do not interact to create a multiplicative effect on the risk of an overall complication; however, they did not examine interactions within individual complications, including flap necrosis. Our study of more than 1,400 mastectomies with immediate tissue expander placement is the first to quantitatively explore the potential synergistic effect of intraoperative fill volume with other risk factors on flap necrosis. Further clarification of the role of intraoperative fill volume will aid in surgical decision making and improve patient outcomes.
Each of the four synergistic relationships we identified can be explained by the effect of risk factors on the blood supply to the native skin flap. By all measures, the most significant interaction was observed between tumescence and high intraoperative fill volume. The impact of tumescence on postoperative complication rates remains controversial. The vasoconstrictive effect of epinephrine from the tumescent solution is believed to affect skin flap viability [6,23]. Some studies have suggested that even transient intraoperative decreases in dermal blood flow can predict postoperative ischemia-induced tissue necrosis [19]. Recently published studies have demonstrated increased rates of major flap necrosis following tumescent mastectomy [6,23]. In our own institution, Seth et al. [6] reported that more than 75% of tumescent-related complications were associated with another independent risk factor, again suggesting compounding effects. In the current series, although tumescence was not an independent risk factor for flap necrosis, when combined with a high intraoperative fill, it conferred a nearly 2-fold increase in risk. Other studies, however, have reported a positive experience with tumescent mastectomy and suggest a role for unmeasured confounders, including the surgeon's technique and experience [24]. In our series, mastectomies were performed by one of four high-volume oncologic breast surgeons with extensive experience with the technique. Combined with the compression of the microvasculature due to high expander fill volumes, the vasoconstrictive effect of tumescence seems to cross a threshold of tissue ischemia, tipping the scales of flap viability toward necrosis.
Increased age, obesity, and hypertension were also found to synergistically increase flap necrosis rates when combined with a high intraoperative fill volume, after adjusting for potential confounders in the logistic regression models. Associated with each of these three risk factors is a host of local and systemic effects that alter blood flow and decrease both the speed and quality of wound healing [25-27]. Small vessel disease associated with these risk factors may decrease mastectomy flap perfusion. These effects may not be large enough to independently manifest themselves as full thickness flap necrosis but are clinically relevant in the setting of high intraoperative fill volumes.
One cited advantage of ADM use in breast reconstruction is higher initial fill volume, which may translate into fewer expansions of shorter duration [28]. Indeed, the rate of ADM use was higher in the group with >66.7% fill volume in this study. ADM use was not associated with mastectomy flap necrosis.
Our study had several limitations, most of which were associated with the retrospective nature of our review. We were limited to only those variables that were widely available within the medical records, and we were therefore unable to comment on other objective measures of the breast including skin flap length and flap thickness. Specifically, the relationship between high intraoperative fill volumes and high body mass index may be confounded by flap length. Patients with a high BMI often have large breast skin envelopes and thus long skin flaps. Furthermore, they are likely to require large fill volumes for full breast projection. It is possible that intraoperative fill volume is a surrogate for mastectomy flap length. Future studies controlling for flap length and the amount of distal skin flap resected are necessary to better clarify the pathophysiological basis of our findings. Flap thickness is influenced by patient characteristics and the experience of the oncologic surgeon, and is an important variable in flap survival [29]. While the ideal study would include such measurements, in our study, we believe that few outliers that would have confounded our results were likely to exist. Finally, the present study describes the results of a single, high-volume surgical center; thus, the rates of flap necrosis and risks ascribed to each risk factor may not be completely generalizable. A high-powered, multicenter, prospective analysis would effectively mitigate many of the inherent biases of this study and better clarify the nature of these synergistic interactions on the development of flap necrosis.
In the postmastectomy, hypovascular milieu, multiple risk factors decreasing flap perfusion interact to cross a threshold and synergistically increase the risk of flap necrosis. As immediate prosthetic-based breast reconstruction continues to be performed with increasing frequency, our findings provide a solid foundation for future analyses to improve patient care and decrease complication rates.
Figures and Tables
Table 3
Unadjusted flap necrosis rate stratified by risk factors for each intraoperative fill cohort

References
1. Albornoz CR, Bach PB, Mehrara BJ, Disa JJ, Pusic AL, McCarthy CM, et al. A paradigm shift in U.S. breast reconstruction: increasing implant rates. Plast Reconstr Surg. 2013; 131:15–23.
2. 2011 Plastic surgery procedural statistics. American Society of Plastic Surgeons;Accessed August 13th, 2013. http://www.plasticsurgery.org/news-and-resources/2011-statistics-.html.
3. Pinsolle V, Grinfeder C, Mathoulin-Pelissier S, Faucher A. Complications analysis of 266 immediate breast reconstructions. J Plast Reconstr Aesthet Surg. 2006; 59:1017–1024.

4. Davies K, Allan L, Roblin P, Ross D, Farhadi J. Factors affecting post-operative complications following skin sparing mastectomy with immediate breast reconstruction. Breast. 2011; 20:21–25.

5. Davila AA, Mioton LM, Chow G, Wang E, Merkow RP, Bilimoria KY, et al. Immediate two-stage tissue expander breast reconstruction compared with one-stage permanent implant breast reconstruction: a multi-institutional comparison of short-term complications. J Plast Surg Hand Surg. 2013; 47:344–349.

6. Seth AK, Hirsch EM, Fine NA, Dumanian GA, Mustoe TA, Galiano RD, et al. Additive risk of tumescent technique in patients undergoing mastectomy with immediate reconstruction. Ann Surg Oncol. 2011; 18:3041–3046.

7. Seth AK, Hirsch EM, Fine NA, Kim JY. Utility of acellular dermis-assisted breast reconstruction in the setting of radiation: a comparative analysis. Plast Reconstr Surg. 2012; 130:750–758.

8. Crosby MA, Dong W, Feng L, Kronowitz SJ. Effect of intraoperative saline fill volume on perioperative outcomes in tissue expander breast reconstruction. Plast Reconstr Surg. 2011; 127:1065–1072.

9. Cordeiro PG, McCarthy CM. A single surgeon's 12-year experience with tissue expander/implant breast reconstruction: part I. a prospective analysis of early complications. Plast Reconstr Surg. 2006; 118:825–831.

10. Goodwin SJ, McCarthy CM, Pusic AL, Bui D, Howard M, Disa JJ, et al. Complications in smokers after postmastectomy tissue expander/implant breast reconstruction. Ann Plast Surg. 2005; 55:16–19.

11. Alderman AK, Wilkins EG, Kim HM, Lowery JC. Complications in postmastectomy breast reconstruction: two-year results of the Michigan Breast Reconstruction Outcome Study. Plast Reconstr Surg. 2002; 109:2265–2274.

12. McCarthy CM, Mehrara BJ, Riedel E, Davidge K, Hinson A, Disa JJ, et al. Predicting complications following expander/implant breast reconstruction: an outcomes analysis based on preoperative clinical risk. Plast Reconstr Surg. 2008; 121:1886–1892.

13. Bailey MH, Smith JW, Casas L, Johnson P, Serra E, de la Fuente R, et al. Immediate breast reconstruction: reducing the risks. Plast Reconstr Surg. 1989; 83:845–851.
14. Sørensen LT, Hørby J, Friis E, Pilsgaard B, Jørgensen T. Smoking as a risk factor for wound healing and infection in breast cancer surgery. Eur J Surg Oncol. 2002; 28:815–820.

15. Mortenson MM, Schneider PD, Khatri VP, Stevenson TR, Whetzel TP, Sommerhaug EJ, et al. Immediate breast reconstruction after mastectomy increases wound complications: however, initiation of adjuvant chemotherapy is not delayed. Arch Surg. 2004; 139:988–991.

16. Staradub VL, Morrow M. Modified radical mastectomy with knife technique. Arch Surg. 2002; 137:105–110.

17. Andersson T, Alfredsson L, Källberg H, Zdravkovic S, Ahlbom A. Calculating measures of biological interaction. Eur J Epidemiol. 2005; 20:575–579.

18. Niinikoski J, Jussila P, Vihersaari T. Radical mastectomy wound as a model for studies of human wound metabolism. Am J Surg. 1973; 126:53–58.

19. Olivier WA, Hazen A, Levine JP, Soltanian H, Chung S, Gurtner GC. Reliable assessment of skin flap viability using orthogonal polarization imaging. Plast Reconstr Surg. 2003; 112:547–555.

20. Losken A, Styblo TM, Schaefer TG, Carlson GW. The use of fluorescein dye as a predictor of mastectomy skin flap viability following autologous tissue reconstruction. Ann Plast Surg. 2008; 61:24–29.

21. Meretoja TJ, Rasia S, von Smitten KA, Asko-Seljavaara SL, Kuokkanen HO, Jahkola TA. Late results of skin-sparing mastectomy followed by immediate breast reconstruction. Br J Surg. 2007; 94:1220–1225.

22. Slavin SA, Schnitt SJ, Duda RB, Houlihan MJ, Koufman CN, Morris DJ, et al. Skin-sparing mastectomy and immediate reconstruction: oncologic risks and aesthetic results in patients with early-stage breast cancer. Plast Reconstr Surg. 1998; 102:49–62.

23. Chun YS, Verma K, Rosen H, Lipsitz SR, Breuing K, Guo L, et al. Use of tumescent mastectomy technique as a risk factor for native breast skin flap necrosis following immediate breast reconstruction. Am J Surg. 2011; 201:160–165.

24. Munhoz AM, Gemperli R, Filassi JR. Comment on: use of tumescent mastectomy technique as a risk factor for native breast skin flap necrosis after immediate breast reconstruction. Am J Surg. 2012; 204:549–550.

25. Holt DR, Kirk SJ, Regan MC, Hurson M, Lindblad WJ, Barbul A. Effect of age on wound healing in healthy human beings. Surgery. 1992; 112:293–297.
26. Gerstein AD, Phillips TJ, Rogers GS, Gilchrest BA. Wound healing and aging. Dermatol Clin. 1993; 11:749–757.

27. Van de Kerkhof PC, Van Bergen B, Spruijt K, Kuiper JP. Age-related changes in wound healing. Clin Exp Dermatol. 1994; 19:369–374.

28. Spear SL, Sher SR, Al-Attar A. Focus on technique: supporting the soft-tissue envelope in breast reconstruction. Plast Reconstr Surg. 2012; 130(5):Suppl 2. 89S–94S.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download