Abstract
Purpose
A more noninvasive evaluation of axillary lymph node in breast cancer is one of the principal challenges of breast cancer treatment. To detect axillary lymph node metastasis (ALNM) in T1 breast cancer, we have compared the axillary ultrasonography (AUS), contrast-enhanced magnetic resonance imaging (cMRI), and 18F-fluorodeoxyglucose positron emission tomography/computed tomography (PET/CT) to determine the most adequate test or a combination of tests.
Methods
Retrospectively, 349 T1 breast cancer patients who were preoperatively examined using AUS, cMRI, and PET/CT between 2008 and 2011 and whom underwent pathological evaluations of axillary lymph nodes were reviewed and analyzed.
Results
In total, 26.4% (92/349) of patients exhibited ALNM. The sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV), and accuracy of AUS for determining ALNM were 44.6%, 88.7%, 58.6%, 81.7%, and 77.1%, respectively. cMRI was similar to AUS. The sensitivity, specificity, PPV, NPV, and accuracy of PET/CT were 44.5%, 94.2%, 73.2%, 82.6%, and 81.1%, respectively. The combination including cMRI and PET/CT was the most accurate with sensitivity, specificity, PPV, NPV, and accuracy values of 39.1%, 98.8%, 92.3%, 81.9%, and 83.1%, respectively. The mean number (3.5±4.2) of ALNMs in the patients who were positive based on cMRI and PET/CT and also pathologically proven to exhibit ALNM was significantly larger than the number (2.16±2.26) in other patients who exhibited ALNM (p=0.035).
Conclusion
There are no definitive modalities for detecting ALNM in T1 breast cancers to replace sentinel lymph node biopsy (SLNB). If ALNM is suspected based on cMRI and PET/CT, the axillary dissection without SLNB might be a better option because it is related to high possibilities of ALNM and large axillary metastatic volumes.
Axillary lymph node metastasis (ALNM) is a key factor for the prognosis of breast cancer and has a major impact on decisions regarding treatment modalities; thus, diagnostically accurate methods for determining ALNM are very important [1,2]. Currently, the standard axillary staging procedure in patients with early breast cancer is sentinel lymph node biopsy (SLNB), which has a lower morbidity rate and similar accuracy as compared with traditional axillary dissection (AD) [3-5]. However, SLNB requires a specialist in nuclear medicine and preoperative lymphoscintigraphy as well as a broad and elaborate pathological examination. Additionally, it is a time consuming and complicated process; thus, SLNB may not be a particularly useful procedure [6,7]. For these reasons, a more noninvasive evaluation of axillary lymph node (ALN) in breast cancer is one of the principal challenges of breast cancer treatment.
Axillary ultrasonography (AUS) is widely used for the detection of ALNM because it is relatively accurate and noninvasive [8,9]. AUS is simple, easy, and less expensive than other methods; therefore, it is an elemental test in breast cancer evaluation. Additionally, AUS can be adjusted for use with fine needle aspiration cytology (FNAC) or core needle biopsy (CNB). Thus, if ALNM is suspected on AUS, the use of FNAC or CNB with AUS can accurately determine ALNM. Subsequently, the patients with ALNM can undergo AD without SLNB and patients who are ALNM negative based on the FNAC or CNB can undergo SLNB. This triage reduces unnecessary SLNB [10,11].
Because early screening is widespread, patients who are newly diagnosed with breast cancer are more often at low stages and have tumors that are small in size; indeed, patients with tumors ≤2 cm in size (T1) account for up to 80% of newly diagnosed patients [12,13]. The rate of ALNM in T1 breast cancer (approximately 21%-40%) is lower than that in patients with larger tumors, and the number and volume of tumors are decreased [1,12,13]. Additionally, most of these tumors are clinically impalpable [1,12,13]. Accordingly, AUS is not accurate enough to determine whether SLNB is necessary in patients with T1 breast cancer [14,15].
In addition to AUS, preoperative contrast-enhanced breast and axilla magnetic resonance imaging (cMRI) and 18F-fluorodeoxyglucose (FDG) positron emission tomography/computed tomography (PET/CT) are noninvasive methods that are usually conducted for the evaluation of patients with breast cancer. cMRI is helpful for the evaluation of the multiplicity and extent of tumors in the breast, and PET/CT is used for the diagnosis of locoregional and distant metastases [16,17]. Both are relatively accurate methods for the evaluation of ALNM as well [16,18-20].
Until now, there has been no comparative study of these 3 modalities (AUS, cMRI, and PET/CT) with respect to their accuracy for the detection of ALNM in T1 breast cancer. The purpose of this study is to determine the accuracy of ALNM detections in T1 breast cancer by examining AUS, cMRI, and PET/CT, either singularly or in combination, to determine which method (or combination of methods) is the best triage test to evaluate whether SLNB should be performed.
We retrospectively researched 1,017 patients with breast cancer who were being consecutively operated at Kyungpook National University Hospital (from January 2008 to December 2011). The exclusion criteria of patients were a tumor size of >2 cm according to a pathological report or a vague tumor size for patients whom had received neoadjuvant chemotherapy or had been diagnosed using vacuum-assisted core biopsy. After these patients were excluded, 470 counts of T1 breast cancer patients remained.
Of these patients, 349 were preoperatively examined using AUS, cMRI, and PET/CT and underwent pathological evaluation of ALNs via SLNB or AD. Subsequently, we researched the clinical, imaging, and pathological characteristics of these 349 patients. We adopted the pathological classification proposed by the American Joint Committee on Cancer (7th edition, 2010). This study was approved by the Institutional Review Board of Kyungpook National University Hospital (IRB No. KNUH 2012-09-012).
An expert radiologist performed bilateral ultrasonography of the breast and axilla with a high frequency linear array transducer (L8-15 MHz) on an Acuson Sequoia® (Siemens Medical Solutions, Mountain View, USA). Lymph nodes were categorized as suspicious if they exhibited one or more of the following characteristics: cortical thickening or eccentric cortical lobulation with obliteration of echogenic hilum, irregular shape, loss of fatty hilum, or round shape [9,11].
We performed cMRI using a GE Signa Excite TwinSpeed® 1.5T (General Electric Medical Systems, Milwaukee, USA) with a 4 channel breast coil that covered the axilla and breast. The examination was performed with the patient in the prone position. First, an axial precontrast T1-weighted spin-echo image (TR/TE=416/10 ms; 3.4 mm slice thickness; 0.1 mm slice gap) and a sagittal T2-weighed fast spin-echo image (TR/TE=3,000/94 ms; 2.6 mm slice thickness) were acquired.
A diffusion-weighted axial image was obtained by single-shot echo planar imaging (b value=750; 1,000 sec/mm2; TR/TE=6,000/86 ms; 3.4 mm slice thickness; 0.1 mm slice gap) before obtaining dynamic contrast-enhanced images using 3D fat-suppressed spoiled gradient recalled echo sequences (TR/TE=6.2/2.9 ms; flip angle 10; FOV 25-28 cm; 2.6 mm slice thickness; pre-enhanced; and 2, 4, 6, 8, and 10-minute images after gadolinium DTPA [Magnevist®; Bayer Healthcare Pharmaceuticals, Berlin, Germany] 0.1 mmol/kg infusion). Additionally, a subtraction image was obtained using precontrast and contrast images.
All patients fasted for at least 6 hours, and blood glucose levels were checked before the administration of 18F-FDG. Patients with elevated blood glucose levels had their examinations rescheduled, and their blood glucose concentration was managed such that it was <150 mg/dL in all subjects. Approximately 8.1 MBq of 18F-FDG per kg of body weight was injected intravenously, and the patients were advised to rest for 1 hour before acquisition of the PET/CT image. PET/CT scans were performed using a Reveal RT-HiREZ 6 slice CT apparatus® (CTIMI, Knoxville, USA) and a 16-slice CT Discovery STE apparatus® (General Electric Healthcare, Milwaukee, USA). Prior to the PET scan, a low-dose CT scan was obtained without contrast enhancement from the skull vertex continuing to the knee with the patient in the supine position with quiet respiration for attenuation correction. PET scans with a maximum spatial resolution of 6.5 mm (Reveal PET/CT) and 5.5 mm (Discovery PET/CT) were also performed from the skull vertex continuing to the knees with 3 minutes per bed position. PET images obtained by the Reveal PET/CT and Discovery PET/CT scanners were reconstructed with a 128×128 matrix, an ordered subset expectation maximum iterative reconstruction algorithm (4 iterations, 8 subsets), a Gaussian filter of 5.0 mm, and a slice thickness of either 3.0 mm (Reveal PET/CT) or 3.27 mm (Discovery PET/CT).
Each SLNB sample was bisected and evaluated with intraoprative frozen section and hematoxylin and eosin staining. The remaining portions of the SLNB samples were subsequently submitted for permanent sectioning and immunohistochemical assay.
SLNBs were performed in 96.8% (338/349) of the patients, and ADs were performed directly in 3.2% (11/349) of patients who were highly suspected to be ALNM positive. Completion ADs were performed in 22.3% (78/349) of the patients because 67 patients had ALNM, and operations were performed on 11 patients during the validation period of SLNB.
We calculated the sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV), and accuracy (ACC) for AUS, cMRI, PET/CT and combinations of the 3 modalities. We compared the similarity between tests using McNemar test. An independent samples t-test was used for comparing the mean number of ALNMs in the patients. SPSS version 18.0K for Windows® (SPSS Inc., Chicago, USA) was used for statistical analysis with p<0.05 considered as significant.
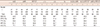
The clinicopathological characteristics of 349 patients are displayed in Tables 1 and 2. The mean age of the patients was 51.3 years (range, 25-79 years). There was a palpable breast tumor in 73.1% (255/349) of patients and a palpable axillary mass in only 2.3% (8/349) of patients. The mean size of the tumor was 1.32 cm (range, 0.1-2.0 cm). The number of T1c (tumor size, ≤2 and >1 cm) patients was 269 (77.1%).
26.4% (92/349) of patients had ALNM. Of these patients, 71.7% (66/92) were at N1, 16.3% (15/92) were at N2, 8.7% (8/92) were at N1mi, and 3.3% (3/92) were at N3. With regard to T-stage, of these patients, 90.2% (83/92) were at T1c, 7.6% (7/92) were at T1b, and 2.2% (2/92) were at T1a (Figure 1).
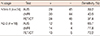
As noted in Table 3, 41.4% (29/70) of patients who were suspected of having ALNM based on preoperative AUS did not actually show ALNM based on pathological examination. 18.3% (51/279) of patients who did not exhibit evidence of ALNM based on preoperative AUS were shown to have ALNM based on pathological examination (sensitivity 44.6%, specificity 88.7%, PPV 58.6%, NPV 81.7%, accuracy 77.1%). Based on cMRI, the false-positive rate was 39.8% (29/73), and the false-negative rate was 17.4% (48/276) (sensitivity 47.8%, specificity 88.7%, PPV 60.2%, NPV 82.6%, accuracy 77.9%). Based on PET/CT, the false-positive and false-negative rates were 26.8% (15/56) and 17.4% (51/293), respectively (sensitivity 44.5%, specificity 94.2%, PPV 73.2%, NPV 82.6%, accuracy 81.1%).
With regards to the similarity between tests, there was no significant difference between AUS and cMRI (p=0.728); however, there was a small difference between PET/CT and AUS (p=0.061) and a significant difference between PET/CT and cMRI (p=0.025).
There were no combinations with high sensitivity and high specificity. The combination of cMRI and PET/CT was most accurate (sensitivity 39.1%, specificity 98.8%, PPV 92.3%, NPV 81.9%, accuracy 83.1%). The mean number of ALNMs in the patients who were positive based on cMRI and PET/CT and also pathologically proven to exhibit ALNM was 3.5±4.2 (range, 1-25), which was significantly larger than the number in other patients who exhibited ALNM (2.16±2.26; range, 1-13) (p=0.035). Additionally, 53% (19/36) of the patients in this group had over 3 ALNMs.
Finally, the sensitivity of the tests was decreased at lower N stages. The sensitivity values of AUS, cMRI, and PET/CT were 45.6%, 45.6%, and 41.6%, respectively, in 74 patients with less than 3 ALNMs (N1mi-1) and 66.7%, 77.8%, and 72.2%, respectively, in 18 patients with more than 4 ALNMs (N2-3) (Table 4).
The sensitivity and specificity of AUS for the detection of ALNM were 61% and 82%, respectively, based on a meta-analysis of 31 studies [14]. van Rijk et al. [10] reported that the sensitivity, specificity, PPV, and NPV were 35%, 82%, 53%, 68%, and 64%, respectively, using 726 breast cancer patients who had no palpable ALN, and the rate of ALNM in this group was 21%. The sensitivity and PPV of AUS for the prediction of ALNM tend to be lower when tumors are smaller or there is a low rate of ALNM [14,23]. In this study, the breast cancer patients had ≤2-cm tumors (T1) with a mean size of 1.32 cm, which is the smallest reported size among studies that reported mean tumor sizes. Additionally, only 2.3% of patients had palpable ALNs; thus, the sensitivity (45.7%) and PPV (59.7%) of AUS for the detection of ALNM were low in this study. Our study also showed a lower sensitivity of AUS in patients at lower N stages.
In this study, because of the low sensitivity and PPV of AUS, many patients with ALMN must undergo SLNB prior to undergoing AD instead of undergoing AD immediately. We determined that cMRI and PET/CT, which are noninvasive and popular preoperative examinations for breast cancer patients, may be helpful for improving the sensitivity and PPV of AUS for detecting ALNM.
cMRI is generally used to evaluate the regional extent of breast cancer before breast-conserving surgery, it examines changes in tumor extent prechemotherapy and postchemotherapy, screens high-risk patients and those with large breasts, evaluates isolated ALNMs of unknown origin, and evaluates ALNM of breast cancer, the latter of which is a less subjective evaluation than that obtained with AUS [16,24]. The sensitivity and specificity of cMRI for predictions of ALMN were 36% to 100% and 54% to 100%, respectively. These ranges were fairly wide because they were dependent on the definition of ALNM, the types of contrast used, the sizes of the breast cancer and the numbers of metastatic ALNs (similar to AUS) [18,19,22,23,25]. Most of the studies showing high sensitivities were undertaken with less than 100 patients, and comparisons were not being made with AUS. Additionally, some studies used unusual enhancement materials [25,26]. Thus, not enough studies have been performed to truly evaluate the realistic accuracy of cMRI for detection of ALNM [25]. Recently, 2 studies examining over 100 breast cancer patients reported that the sensitivity of cMRI for the detection of ALNM was below 40%, which was lower than AUS, although the accuracy of the cMRI was similar to that of AUS [22,23]. Our study showed that cMRI had a higher sensitivity and PPV (sensitivity 47.8%, specificity 88.7%, PPV 60.2%, NPV 82.6%, accuracy 77.9%) than AUS (sensitivity 44.6%, specificity 88.7%, PPV 58.6%, NPV 81.7%, accuracy 77.1%); however, these differences were very small.
PET/CT is useful for evaluating distant metastasis, extranodal extension, and ALNM in breast cancer patients [17]. The sensitivity (20%-77%) and specificity (65%-100%) of PET/CT for detecting ALNM cover a wide range [19,20,27-30]. In the study that examined 136 T1 breast cancer patients, the sensitivity and specificity of PET/CT for predicting ALNM were 34% and 97%, respectively [27]. Chae et al. [28] reported that because the sensitivity (48.5%), specificity (84%), and accuracy (73.2%) of PET/CT were lower than the same parameters for AUS (sensitivity 51.5%, specificity 89.3%, accuracy 77.8%), PET/CT was not an adequate means of detecting ALNM in breast cancer. However, Ueda et al. [29] indicated that the accuracies of AUS (sensitivity 57.6%, specificity 95.2%, PPV 85%, NPV 82%, accuracy 83.1%) and PET/CT (sensitivity 54.2%, specificity 85%, PPV 97%, NPV 82%, accuracy 84.7%) were similar. Additionally, when 2 examinations indicated the possibility of ALNM, PPV was 100%, and when 2 examinations were negative for ALNM, NPV was 85%. Thus, PET/CT could provide additional information regarding ALNM when AUS is also used. Kim et al. [30] also reported that there was no difference between PET/CT and AUS, and combined examinations improved PPV and NPV. In this study, the sensitivity and PPV of PET/CT for detecting ALNM (sensitivity 44.5%, specificity 94.2%, PPV 73.7%, NPV 82.3%, accuracy 80.9%) were lower than the values reported in other studies because of a smaller tumor size and lower incidence of ALNM, as lower values were similarly also observed when using AUS and cMRI.
In this study, we were able to compare 3 tests for ALNM directly for over 300 patients with T1 breast cancer for the first time. For the 3 tests that were examined, sensitivity ranged from 44.5% to 47.8%, and while the sensitivity of cMRI was the highest, the differences were very small. Of the 3 tests, PET/CT showed the highest specificity, PPV, and accuracy (94.2%, 73.2%, and 81.1%, respectively). Based on the above results, PET/CT was the most accurate test for detection of ALNM; however, it was not a definitive test because it had the lowest sensitivity and its PPV was below 80%.
The next step was to search the combination of 3 tests to determine which had a higher NPV or PPV than the single test. When all 3 examinations were negative, NPV (84%) was the highest value. However, the differences in NPV between each single examination were not large (1%-2%), and the false-negative rate was 16% (41/249), and these false-negative patients represented 45.1% (41/92) of the patients with ALNM. Therefore, even if all examinations were negative, SLNB would be necessary to confirm ALNM.
When all 3 examinations were positive, the PPV (94%) was the highest value and the differences in PPV between each single examination were 20.9% to 35.5%. When cMRI and PET/CT were positive, the PPV (92%) was similarly high. AUS with cMRI or PET/CT showed lower PPVs (AUS & cMRI 69%, AUS & PET/CT 84.6%). Therefore, the highest PPV for all positive values on the 3 tests mainly derives from the positives of cMRI and PET/CT.
All positives on cMRI and PET/CT showed a lower PPV, a higher sensitivity than all positives on 3 tests, and the difference (4.3%) in sensitivity was larger than the gap (2.1%) in PPV. Thus, the accuracy of the combination for cMRI and PET/CT was the highest in single tests or the combination of tests. If AD without SLNB was done when ALNM was suspected based on cMRI and PET/CT, 11% (36/349) of all T1 patients or 39% (36/92) of the patients with ALNM might avoid unnecessary SLNB. On the other hand, AD would be overtreatment in 0.9% (3/349) of all T patients or 1.2% (3/257) of the patients without ALNM. However, SLNB basically has risk of false negatives and our study also showed that the combination of cMRI and PET/CT was related with larger axillary metastatic volumes. Therefore, if ALNM is suspected based on cMRI and PET/CT, AD without SLNB might be a better option.
There are several limitations to our study. First, this is a retrospective study, and the interpreters of the cMRI and PET/CT had knowledge of the AUS results for the most part. Thus, this knowledge may have affected the results of cMRI and PET/CT. However, cMRI and PET/CT have their own diagnostic criteria for ALNM not related with ultrasonographic findings, so AUS may not have definitive effects on the results of cMRI and PET/CT. Additionally, the determination of pathological ALNM mostly depended on SLNBs (74.5%); however, SLNB has a high level of accuracy similar to that of AD [3,4]. Thus, the difference between these 2 methods may be small. cMRI and PET/CT are very expensive to implement, so the cost effectiveness of the 2 examinations is questionable. However, as mentioned earlier, cMRI and PET/CT were conducted not only for detections of ALNM but also for various other reasons.
For detection of ALNM in T1 breast cancer patients, there are no definitive modalities to replace the SLNB. Although PET/CT is more accurate than AUS and cMRI, it is insufficient for decision-makings. If ALNM is suspected based on cMRI and PET/CT, the AD without SLNB might be a better option because it is related to high possibilities of ALNM and large axillary metastatic volumes.
Figures and Tables
 | Figure 1Frequency of axillary lymph node metastasis (ALNM) based on T-stage. The table provides the precise patient numbers and percentages, which are represented graphically in the figure. |
Table 3
Detection of axillary lymph node metastasis by image studies
AUS=axillary ultrasonography; cMRI=contrast-enhanced magnetic resonance imaging; PET/CT=18F-fluorodeoxyglucose positron emission tomography/computed tomography; ≥1+=axillary lymph node metastasis was suspected based on the results of more than one test; ≥2+=axillary lymph node metastasis was suspected based on the results of more than two tests; 3+=axillary lymph node metastasis was suspected based on the results of all 3 tests; PALNM=pathologic axillary lymph node metastasis; SEN=sensitivity; SPEC=specificity; PPV=positive predictive value; NPV=negative predictive value; ACC=accuracy.
Notes
References
1. Carter CL, Allen C, Henson DE. Relation of tumor size, lymph node status, and survival in 24,740 breast cancer cases. Cancer. 1989; 63:181–187.

2. Wilking N, Rutqvist LE, Carstensen J, Mattsson A, Skoog L. Stockholm Breast Cancer Study Group. Prognostic significance of axillary nodal status in primary breast cancer in relation to the number of resected nodes. Acta Oncol. 1992; 31:29–35.

3. Giuliano AE, Jones RC, Brennan M, Statman R. Sentinel lymphadenectomy in breast cancer. J Clin Oncol. 1997; 15:2345–2350.

4. Krag DN, Anderson SJ, Julian TB, Brown AM, Harlow SP, Ashikaga T, et al. Technical outcomes of sentinel-lymph-node resection and conventional axillary-lymph-node dissection in patients with clinically node-negative breast cancer: results from the NSABP B-32 randomised phase III trial. Lancet Oncol. 2007; 8:881–888.

5. Crane-Okada R, Wascher RA, Elashoff D, Giuliano AE. Long-term morbidity of sentinel node biopsy versus complete axillary dissection for unilateral breast cancer. Ann Surg Oncol. 2008; 15:1996–2005.

6. Purushotham AD, Upponi S, Klevesath MB, Bobrow L, Millar K, Myles JP, et al. Morbidity after sentinel lymph node biopsy in primary breast cancer: results from a randomized controlled trial. J Clin Oncol. 2005; 23:4312–4321.

7. Goyal A, Newcombe RG, Chhabra A, Mansel RE. Morbidity in breast cancer patients with sentinel node metastases undergoing delayed axillary lymph node dissection (ALND) compared with immediate ALND. Ann Surg Oncol. 2008; 15:262–267.

8. Rajesh YS, Ellenbogen S, Banerjee B. Preoperative axillary ultrasound scan: its accuracy in assessing the axillary nodal status in carcinoma breast. Breast. 2002; 11:49–52.

9. Alvarez S, Añorbe E, Alcorta P, López F, Alonso I, Cortés J. Role of sonography in the diagnosis of axillary lymph node metastases in breast cancer: a systematic review. AJR Am J Roentgenol. 2006; 186:1342–1348.

10. van Rijk MC, Teertstra HJ, Peterse JL, Nieweg OE, Olmos RA, Hoefnagel CA, et al. Ultrasonography and fine-needle aspiration cytology in the preoperative evaluation of melanoma patients eligible for sentinel node biopsy. Ann Surg Oncol. 2006; 13:1511–1516.

11. Jung J, Park H, Park J, Kim H. Accuracy of preoperative ultrasound and ultrasound-guided fine needle aspiration cytology for axillary staging in breast cancer. ANZ J Surg. 2010; 80:271–275.

12. Bevilacqua JL, Kattan MW, Fey JV, Cody HS 3rd, Borgen PI, Van Zee KJ. Doctor, what are my chances of having a positive sentinel node? A validated nomogram for risk estimation. J Clin Oncol. 2007; 25:3670–3679.

13. Viale G, Zurrida S, Maiorano E, Mazzarol G, Pruneri G, Paganelli G, et al. Predicting the status of axillary sentinel lymph nodes in 4351 patients with invasive breast carcinoma treated in a single institution. Cancer. 2005; 103:492–500.

14. Houssami N, Ciatto S, Turner RM, Cody HS 3rd, Macaskill P. Preoperative ultrasound-guided needle biopsy of axillary nodes in invasive breast cancer: meta-analysis of its accuracy and utility in staging the axilla. Ann Surg. 2011; 254:243–251.

15. Solon JG, Power C, Al-Azawi D, Duke D, Hill AD. Ultrasound-guided core biopsy: an effective method of detecting axillary nodal metastases. J Am Coll Surg. 2012; 214:12–17.

16. Mameri CS, Kemp C, Goldman SM, Sobral LA, Ajzen S. Impact of breast MRI on surgical treatment, axillary approach, and systemic therapy for breast cancer. Breast J. 2008; 14:236–244.

17. Danforth DN Jr, Aloj L, Carrasquillo JA, Bacharach SL, Chow C, Zujewski J, et al. The role of 18F-FDG-PET in the local/regional evaluation of women with breast cancer. Breast Cancer Res Treat. 2002; 75:135–146.

18. Kvistad KA, Rydland J, Smethurst HB, Lundgren S, Fjøsne HE, Haraldseth O. Axillary lymph node metastases in breast cancer: preoperative detection with dynamic contrast-enhanced MRI. Eur Radiol. 2000; 10:1464–1471.

19. Peare R, Staff RT, Heys SD. The use of FDG-PET in assessing axillary lymph node status in breast cancer: a systematic review and meta-analysis of the literature. Breast Cancer Res Treat. 2010; 123:281–290.

20. Gil-Rendo A, Zornoza G, García-Velloso MJ, Regueira FM, Beorlegui C, Cervera M. Fluorodeoxyglucose positron emission tomography with sentinel lymph node biopsy for evaluation of axillary involvement in breast cancer. Br J Surg. 2006; 93:707–712.

21. Luciani A, Dao TH, Lapeyre M, Schwarzinger M, Debaecque C, Lantieri L, et al. Simultaneous bilateral breast and high-resolution axillary MRI of patients with breast cancer: preliminary results. AJR Am J Roentgenol. 2004; 182:1059–1067.

22. Valente SA, Levine GM, Silverstein MJ, Rayhanabad JA, Weng-Grumley JG, Ji L, et al. Accuracy of predicting axillary lymph node positivity by physical examination, mammography, ultrasonography, and magnetic resonance imaging. Ann Surg Oncol. 2012; 19:1825–1830.

23. García Fernández A, Fraile M, Giménez N, Reñe A, Torras M, Canales L, et al. Use of axillary ultrasound, ultrasound-fine needle aspiration biopsy and magnetic resonance imaging in the preoperative triage of breast cancer patients considered for sentinel node biopsy. Ultrasound Med Biol. 2011; 37:16–22.

24. Ko EY, Han BK, Shin JH, Kang SS. Breast MRI for evaluating patients with metastatic axillary lymph node and initially negative mammography and sonography. Korean J Radiol. 2007; 8:382–389.

25. Harnan SE, Cooper KL, Meng Y, Ward SE, Fitzgerald P, Papaioannou D, et al. Magnetic resonance for assessment of axillary lymph node status in early breast cancer: a systematic review and meta-analysis. Eur J Surg Oncol. 2011; 37:928–936.

26. Memarsadeghi M, Riedl CC, Kaneider A, Galid A, Rudas M, Matzek W, et al. Axillary lymph node metastases in patients with breast carcinomas: assessment with nonenhanced versus uspio-enhanced MR imaging. Radiology. 2006; 241:367–377.

27. Veronesi U, De Cicco C, Galimberti VE, Fernandez JR, Rotmensz N, Viale G, et al. A comparative study on the value of FDG-PET and sentinel node biopsy to identify occult axillary metastases. Ann Oncol. 2007; 18:473–478.

28. Chae BJ, Bae JS, Kang BJ, Kim SH, Jung SS, Song BJ. Positron emission tomography-computed tomography in the detection of axillary lymph node metastasis in patients with early stage breast cancer. Jpn J Clin Oncol. 2009; 39:284–289.





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download