Abstract
Purpose
The aim of this study was to evaluate and compare the rate of sister chromatid exchange (SCE), the occurrence of micronuclei, and the lymphocyte proliferation rate index (PRI) in patients with breast cancer, their first-degree relatives, and healthy volunteers.
Methods
We analyzed the frequency of SCE and micronuclei, and the PRI in the peripheral blood lymphocytes of 30 women with breast cancer, 22 of their female family members, and 20 age-matched healthy female volunteers.
Results
SCE occurred significantly more often in the lymphocytes of breast cancer patients (10.84±0.4 per metaphase), compared with their first-degree relatives (7.45±0.54) and controls (5.94±0.2) (p<0.001 for both). The mean SCE frequency was not statistically different between first-degree relatives and controls (p=0.071). Similarly, micronuclei occurred at a significantly higher rate in breast cancer patients (9.6±0.72), and in their first-degree relatives (7±0.64), compared to controls (3.85±0.4) (p<0.001 and p=0.001, respectively). There was also a significant difference between the occurrence of micronuclei in patients compared to their family members (p=0.021). The PRI was significantly lower in patients (1.61±0.1), compared with both their first-degree relatives (1.75±0.1), and controls (1.74±0.1) (p=0.001 and p=0.002, respectively).
The frequency of sister chromatid exchanges (SCEs), the occurrence of micronuclei, and the proliferation rate index (PRI) in peripheral blood lymphocytes are cytogenetic markers of chromosome instability that have been implicated in the development of many tumors [1-4]. The relevance of frequent cytogenetic alterations as a cancer risk biomarker is further supported by epidemiological studies [5-7]. SCEs, which are symmetric exchanges between portions of apparently homologous sister chromatids, involve DNA breakage and its subsequent religation. Micronuclei are produced by chromosome fragment exclusion or whole chromosome lagging at mitosis. Their presence indirectly reflects chromosome breakage or impairment of the mitotic apparatus. SCE and micronuclei have been shown to be elevated in a number of different types of cancer [3,8-12]. Using an SCE assay, we were able to obtain the PRI, an indicator of cell proliferation that reflects cytotoxic events or mutagenesis that can cause cancer.
Breast cancer is primarily a multifactorial disease resulting from a combination of environmental and heritable factors. A number of large epidemiological studies have shown that the relative risk of breast cancer is greater for first-degree relatives and is associated with the number of affected individuals in the family.
The aim of the current study was to evaluate the incidence of micronuclei and SCE, as well as the PRI in the peripheral blood lymphocytes of breast cancer patients before chemotherapy or radiotherapy treatment, their first-degree relatives, and healthy women. We also wished to establish whether there was an association between DNA damage and the level of specific tumor markers.
We performed SCE analysis for 30 female patients with breast cancer (56.4±2.3 years), 22 first-degree relatives (43±2.9 years), and 20 healthy female volunteers (52±2.1 years). None of the patients had been treated with cytotoxic drugs or radiotherapy. Fourteen of the breast cancer patients had a family history of this disease. Amongst the first-degree relative group, the enrolled individuals were a mother in 3 cases, a sister in 9 cases, and a daughter in 10 cases, none of whom had cancer themselves. None of the individuals in the control group had a personal or family history of cancer. Patient characteristics (family history of cancer, age, and smoking habit) and tumor characteristics (cancer size and grade, presence of metastatic axillary lymph nodes) were evaluated (Table 1).
This study was approved by the ethical committee of the Süleyman Demirel University Medical Faculty (resolution No. 873 dated April 3, 2010).
Peripheral blood was collected from all patients prior to surgery, chemotherapy, or radiotherapy, as well as from their first-degree relatives, and age- and sex-matched healthy donors of a similar socioeconomic status from the same region of Turkey. None reported consuming alcohol, the use of a genotoxic medicine, a known genetic disorder, or any kind of cancer.
Blood culture, harvesting, and slide preparation were performed according to the established protocol [13], with some modifications. Heparinized whole blood was cultured in 4.7 mL of RPMI-1640 medium (BIO1-106-1B; Biological Industries Israel Beit Haemek Ltd., Kibbutz Beit Haemek, Israel) containing 20% fetal calf serum (BIO4-001-1B; Biological Industries Israel Beit Haemek Ltd.), 2% phytohemagglutinin (BIO12-006-1H; Biological Industries Israel Beit Haemek Ltd.), L-glutamine (BIO3-020-1B; Biological Industries Israel Beit Haemek Ltd.), and penicillin/streptomycin (BIO3-031-1B; Biological Industries Israel Beit Haemek Ltd.). Then, 5-bromodeoxyuridine (Sigma B5002; Sigma-Aldrich Co., LLC, St. Louis, USA) was added after 48 hours to give a final concentration of 10 µg/mL. Cultures were set up in darkly stained flasks that were additionally wrapped with aluminum foil to protect them from light. The total culture time was 72 hours including the final 2 hours of colcemid treatment (10 µg/mL, 12-003-1C; Biological Industries Israel Beit Haemek Ltd.). The cells were then exposed to a hypotonic solution of potassium chloride at 37℃ for 10 minutes, fixed in a mixture of methanol and glacial acetic acid (3:1), and thoroughly washed in fresh fixative 3 times. SCE staining was performed as previously described [14]. Slides were stained with Giemsa in phosphate buffer (pH 7.0).
For micronucleus analysis, whole-blood cultures were set up as per the SCE protocol, but without 5-bromodeoxyuridine. To obtain binucleated cells, cytochalasin B (6 µg/mL) was added to each culture 68 hours after their initiation. All the other steps were the same as those used for the SCE procedure. Under 100× magnification, a minimum of 1,000 binucleated cells with well-preserved cytoplasm were scored from each patient and the micronucleus frequency was calculated by dividing the total number of micronuclei present in binucleated cells by the total number of binucleated cells.
For analysis of the lymphocyte PRI, in fluorescence plus Giemsa-stained preparations, cells dividing for the first (M1), second (M2), or third time (M3) in culture containing 5-bromodeoxyuridine were identified by the differential staining pattern of the sister chromatids. In brief, M1 cells contained chromosomes in which both sister chromatids were uniformly stained dark. The M2 cells contained only harlequin chromosomes, with one chromatid darkly stained and its sister chromatid lightly stained, and M3 cells contained chromosomes with both sister chromatids showing a uniformly light stain. Lymphocyte proliferation kinetics were studied using 100 differentially stained metaphases per blood sample. The PRI was calculated using the formula: PRI=(M1+2M2+3M3)/100, as described by Lamberti et al. [15].
Statistical analysis was performed using the Graphpad Instant Tm program (GraphPad Instant 3; GraphPad Software Inc., San Diego, USA). Mann-Whitney U, Kruskal-Wallis, chi-square, and Spearman nonparametric correlation tests were used for the interpretation of the results where appropriate. The level of statistical significance was 0.05.
The age, smoking habits, menopause status, and pregnancy at term of the patients, first-degree relatives, and controls are listed in Table 1. None of the patients in either group smoked, and only 5 of the first-degree relatives smoked (22.7%) (p=0.002). There was no statistically significant difference between the mean number of SCEs and occurrence of micronuclei between smokers and nonsmokers. The mean ages of the patients, first-degree relatives, and controls were 56.4±2.3, 43±2.9, and 52±2.1 years, respectively (p=0.011). There was no significant association between the mean age of the patients, first-degree relatives, and controls and DNA damage evaluated on the basis of SCE, micronuclei, and PRI (Table 2).
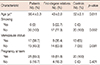
The occurrence of SCE and micronuclei, and the PRI in lymphocytes from 30 treatment-naïve breast cancer patients, 22 of their first-degree relatives, and 20 control subjects are summarized in Table 3. The mean SCE frequency was significantly higher in patients compared to both first-degree relatives and controls (p<0.0001 for both), but was not statistically different between first-degree relatives and controls (p=0.071). The mean micronuclei frequency was significantly higher in patients and first-degree relatives compared to controls (p<0.001 and p=0.001, respectively). There was also a significant difference in the mean number of micronuclei between patients and their first-degree relatives (p=0.021). The mean PRI was significantly lower in patients compared to both first-degree relatives and controls (p=0.001 and p=0.002, respectively), but did not differ significantly between first-degree relatives and control subjects.
The clinical and pathological characteristics of patients were also taken into account in the analysis of SCE, micronuclei, and PRI values. Fifteen patients had lymph node metastasis, and the mean number of excised lymph nodes and positive lymph nodes was 28.73 (range, 18-46) and 5.67 (range, 1-19), respectively. The mean number of SCE and micronuclei, and PRI with respect to tumor T stage, tumor grade, and the presence of lymph node metastasis are shown in Table 4. Only the mean PRI in the group of patients with lymph node metastasis (1.56±0.1) was significantly lower than patients without lymph node metastasis (1.67±0.11).
In the present study, the levels of spontaneous DNA damage in lymphocytes of treatment-naïve breast cancer patients, their first-degree relatives, and healthy control subjects were examined. All of these individuals underwent the same examination at the same hospital. SCE, micronuclei, and the PRI were used as indicators of DNA damage.
Increasing age and smoking may both cause increased instability in the transcription and structure of the genome [16,17]. SCE frequency, micronuclei occurrence, and the PRI are cytological markers of chromosome loss and cellular proliferation. None of the cancer patients or control subjects were smokers, and only 5 (22.7%) of the first-degree relatives had a smoking habit (p=0.002). In the first-degree relative group, there was no statistically significant difference in the mean number of SCE and micronuclei between smokers and nonsmokers (p>0.05). There was however a statistically significant difference in the mean ages of the patients, first-degree relatives, and control subjects (p=0.011), with a younger average age in the first-degree relatives group. There were no significant associations between patient age and the number of SCEs and micronuclei, and PRI values between any of the groups (Table 2).
Genomic instability, caused by the mutation of target genes, increases the chance of developing cancer. The extent of SCE is a widely used indicator for chromosomal stability in lymphocytes from patients affected with both malignant and nonmalignant disorders [2,9,18]. Elevated SCE in the lymphocytes of patients with various cancers has been found in several studies. For instance, the peripheral lymphocytes from patients with carcinoma of the cervix uteri were found to have a mean of 7.8 SCEs per metaphase, which was slightly higher than that of the control group [19]. An increased level of SCEs has also been observed in the lymphocytes from patients with ovarian cancer, where there was a mean value of 18 SCEs per cell, which was significantly higher than the lymphocytes from healthy volunteers (6.9 per cell) [20]. Likewise, lymphocytes from patients with hereditary breast cancer had on average 11 SCEs per cell, which was significantly higher than those of the control group (7.7 SCEs per cell) [21]. In the present study, lymphocyte SCE frequency was used as a marker of genomic instability. It was elevated (10.8±0.4) in women with breast cancer compared to those of the control group (5.9±0.2, p<0.001). This elevation in the SCE frequency among breast cancer patients may be due to the involvement of genetic factors in the causation of the disease, and hence the SCE assay may be considered as a potential indicator for the development of breast cancer in at-risk individuals.
In this study, we measured the SCE levels in both patients and their first-degree relatives. An increased SCE frequency in patients and their first-degree relatives has also been demonstrated in some previous studies. Cefle et al. [22] showed that SCE frequency was significantly higher in young women with breast cancer (n=20, all <40 years old) and in their first-degree relatives (n=20), compared with controls (n=20), all of whom were from western Turkey. They concluded that patients with early-onset breast cancer exhibit increased genomic instability, as do their first-degree relatives. In another study, Roy et al. [21] evaluated the occurrence of SCEs in peripheral blood lymphocytes of hereditary breast cancer patients (n=11) and healthy blood relatives (n=36). They observed a significantly higher group mean value for SCEs/cell in breast cancer patients (11.01 SCEs/cell) and their first-degree relatives (9.69 SCEs/cell) compared to the control group (7.67 SCEs/cell). In our study, the level of SCE was significantly raised only in the patient group. Although the difference in the mean SCE levels between the patient and first-degree relative group did not reach statistical significance, the borderline significance (p=0.071) in this case may indicate a high level of chromosomal instability in breast cancer families. Marked interindividual differences in SCE values were observed in the first-degree relatives. While some individuals had very low mean SCE levels (3.2) in this group, others had very high levels (11.8) (Table 3). Several lines of evidence suggest that differences in DNA repair capacity among individuals reflect genetic differences, and that first-degree relatives with a high mean SCE value may have an increased risk of developing breast cancer. However, a long-term follow-up of patients and their first-degree relatives with higher SCE frequencies is necessary to establish the clinical applicability of this cytogenetic marker.
The micronucleus assay in human lymphocytes is one of the most common methods used for measuring DNA damage in human populations because it is relatively easier to score micronuclei than chromosomal aberrations [15]. It is now well established that micronuclei are formed by the condensation of acentric chromosomal fragments or by whole chromosomes lagging behind cell division. As micronuclei are detected during interphase, they are the only biomarkers that allow the evaluation of both clastogenic and aneuploidogenic effects in a wide range of cells [23]. Higher micronuclei frequencies were previously observed in breast cancer patients relative to controls [24,25]. Santos et al. [25] showed that micronuclei frequencies were significantly higher in breast cancer patients (23.2±1.4) compared to healthy control subjects (10.4±0.7, p<0.0102). In our study, we measured the micronuclei levels in both patients and their first-degree relatives (Table 3). Increased numbers of micronuclei were present in both the patients (9.6±0.7) and their first-degree relatives (7±0.6) compared to the control subjects (3.9±0.4) (p<0.001 and p=0.001, respectively). The elevated number of micronuclei in the breast cancer patients may be due to the involvement of genetic factors in the causation of the disease, and similarly, a high number of micronuclei among their blood relatives may indicate inheritance of the phenomenon.
Using the SCE assay, we were able to obtain the PRI, an indicator of cell proliferation that reflects cytotoxic events. The delay in cell turnover times resulting from exposure to cytotoxic agents or mutagens that can cause cancer may also decrease the PRI. These mutagens may also reduce the proliferative capacity of lymphocytes. Santos et al. [25] found that the PRI in patients was not significantly different from that of healthy control subjects. In contrast, Kopjar et al. [26] found that breast cancer patients had a significantly lower PRI compared with healthy women. Similarly, we showed that the PRI in the patient group was significantly lower than that of the healthy control group (Table 3). Mechanisms that could explain the reduced PRI in cancer patients include metabolic stress due to tumor growth, clastogenic products released by the tumor cells, or mutagens generated by the cancer.
We also evaluated the possible influence of some clinical-pathological features of breast cancer on the numbers of SCEs and micronuclei, and the PRI, the patient group (Table 4). Tumor stage, tumor grade, and presence of lymph node metastasis were not related to the occurrence of micronuclei or SCEs. However, the mean PRI was lower in patients with lymph node metastasis than in those without lymph node metastasis (p=0.009). The presence of lymph node metastasis may represent a cytotoxic event for peripheral blood lymphocytes of cancer patients.
In conclusion, we have found that peripheral blood lymphocytes of treatment-naïve breast cancer patients exhibit higher numbers of SCEs and micronuclei, and a lower PRI than healthy control subjects. In addition, the first-degree relatives of breast cancer patients also have more micronuclei, a slightly higher frequency of SCE, and similar levels of PRI compared to the control group.
Figures and Tables
Table 2
Correlations between the ages of the patients, first-degree relatives, and controls and the DNA damage evaluated with SCE, MN, and PRI levels of them
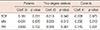
Table 3
SCE, MN, and PRI in untreated breast cancer patients, their first-degree relatives, and controls

Table 4
Breast tumor characteristics and the DNA damage evaluated with SCE, MN, and PRI

SCE=sister chromatid exchange; MN=micronucleus; PRI=proliferation rate index.
*Values of SCE, MN, and PRI are presented as mean±SD; †Nuclear grade are evaluated with Bloom-Richardson grading; ‡Presence of lymph node metastasis compared to absence of lymph node metastasis in breast cancer patients, p=0.009.
References
1. Sandberg AA. Chromosome abnormalities in human cancer and leukemia. Mutat Res. 1991; 247:231–240.

2. Dhillon VS, Dhillon IK. Chromosome aberrations and sister chromatid exchange studies in patients with prostate cancer: possible evidence of chromosome instability. Cancer Genet Cytogenet. 1998; 100:143–147.

3. Mohana Devi S, Balachandar V, Arun M, Suresh Kumar S, Balamurali Krishnan B, Sasikala K. Analysis of genetic damage and gene polymorphism in hepatocellular carcinoma (HCC) patients in a South Indian population. Dig Dis Sci. 2013; 58:759–767.

4. Albertini RJ, Anderson D, Douglas GR, Hagmar L, Hemminki K, Merlo F, et al. IPCS guidelines for the monitoring of genotoxic effects of carcinogens in humans: International Programme on Chemical Safety. Mutat Res. 2000; 463:111–172.

5. Hagmar L, Bonassi S, Strömberg U, Brøgger A, Knudsen LE, Norppa H, et al. Chromosomal aberrations in lymphocytes predict human cancer: a report from the European Study Group on Cytogenetic Biomarkers and Health (ESCH). Cancer Res. 1998; 58:4117–4121.
6. Bonassi S, Hagmar L, Strömberg U, Montagud AH, Tinnerberg H, Forni A, et al. Chromosomal aberrations in lymphocytes predict human cancer independently of exposure to carcinogens: European Study Group on Cytogenetic Biomarkers and Health. Cancer Res. 2000; 60:1619–1625.
7. Fucić A, Znaor A, Strnad M, van der Hel O, Aleksandrov A, Miskov S, et al. Chromosome damage and cancer risk in the workplace: the example of cytogenetic surveillance in Croatia. Toxicol Lett. 2007; 172:4–11.

8. Dhar PK, Devi S, Rao TR, Kumari U, Joseph A, Kumar MR, et al. Significance of lymphocytic sister chromatid exchange frequencies in ovarian cancer patients. Cancer Genet Cytogenet. 1996; 89:105–108.

9. Dhillon VS, Kler RS, Dhillon IK. Choromosome instabililty and sister chromatid exchange (SCE) studies in patients with carcinoma of cervix uteri. Cancer Genet Cytogenet. 1996; 86:54–57.

10. Dhillon VS, Bhasker R, Kler RS, Husain SA. Sister chromatid exchange (SCE) studies in breast cancer patients: a follow-up study. Cancer Genet Cytogenet. 1995; 80:115–117.

11. Narin A, Tuncay O. Relationships between malignant melanoma and chromosome damage in human peripheral blood lymphocytes. Asian Pac J Cancer Prev. 2012; 13:5229–5232.

12. Gutiérrez-Enríquez S, Ramón Y, Alonso C, Corral A, Carrasco P, Cornet M, et al. Ionizing radiation or mitomycin-induced micronuclei in lymphocytes of BRCA1 or BRCA2 mutation carriers. Breast Cancer Res Treat. 2011; 127:611–622.

13. Barch MJ, Lawce HJ, Arsham MS. Peripheral blood culture. In : Barch MJ, editor. The ACT Cytogenetics Laboratory Manual. 2nd ed. New York: Raven Press;1991. p. 24–30.
14. Perry P, Wolff S. New Giemsa method for the differential staining of sister chromatids. Nature. 1974; 251:156–158.

15. Lamberti L, Bigatti Ponzetto P, Ardito G. Cell kinetics and sister-chromatid-exchange frequency in human lymphocytes. Mutat Res. 1983; 120:193–199.

16. Orta T, Günebakan S. The effect of aging on micronuclei frequency and proliferation in human peripheral blood lymphocytes. Indian J Hum Genet. 2012; 18:95–100.

17. Hoffmann H, Speit G. Assessment of DNA damage in peripheral blood of heavy smokers with the comet assay and the micronucleus test. Mutat Res. 2005; 581:105–114.

18. Nordenson I, Beckman L, Lidén S, Stjernberg N. Chromosomal aberrations and cancer risk. Hum Hered. 1984; 34:76–81.

19. Cortés-Gutiérrez EI, Cerda-Flores RM, Leal-Garza CH. Sister chromatid exchanges in peripheral lymphocytes from women with carcinoma of the uterine cervix. Cancer Genet Cytogenet. 2000; 122:121–123.

20. Baltaci V, Kayikçioğlu F, Alpas I, Zeyneloğlu H, Haberal A. Sister chromatid exchange rate and alkaline comet assay scores in patients with ovarian cancer. Gynecol Oncol. 2002; 84:62–66.

21. Roy SK, Trivedi AH, Bakshi SR, Patel RK, Shukla PH, Patel SJ, et al. Spontaneous chromosomal instability in breast cancer families. Cancer Genet Cytogenet. 2000; 118:52–56.

22. Cefle K, Ucur A, Guney N, Ozturk S, Palanduz S, Tas F, et al. Increased sister chromatid exchange frequency in young women with breast cancer and in their first-degree relatives. Cancer Genet Cytogenet. 2006; 171:65–67.

23. Pastor S, Creus A, Parrón T, Cebulska-Wasilewska A, Siffel C, Piperakis S, et al. Biomonitoring of four European populations occupationally exposed to pesticides: use of micronuclei as biomarkers. Mutagenesis. 2003; 18:249–258.

24. Aristei C, Stracci F, Guerrieri P, Anselmo P, Armellini R, Rulli A, et al. Frequency of sister chromatid exchanges and micronuclei monitored over time in patients with early-stage breast cancer: results of an observational study. Cancer Genet Cytogenet. 2009; 192:24–29.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download