Abstract
Purpose
According to the National Surgical Adjuvant Breast and Bowel Project P1 (NSABP-P1) study, tamoxifen can prevent 49% of invasive breast cancers in patients who have a 5-year risk of 1.67% or more. Because tamoxifen is associated with both adverse effects (endometrial cancer, stroke, pulmonary embolism) and protective effect (fracture prevention), it is necessary to weigh the risks and benefits of using tamoxifen for prevention in Korean women. This study weighed those risks and benefits.
Methods
Data were reviewed on the incidences of breast cancer, hip fracture, endometrial cancer and stroke in the absence of tamoxifen treatment in Korean women. We also reviewed NSABP-P1 data on the effects of tamoxifen on these outcomes. A risk-benefit index was calculated according to age and specific risk of breast cancer. Sensitivity analyses were performed with assumptions regarding the effects of tamoxifen.
Results
Compared to U.S. women, the numbers of hip fractures and endometrial cancers were lower, but the number of strokes was much higher. The net benefit of tamoxifen was reduced with increasing age because of a high risk of stroke in older women. Older Korean women had more risk than benefit from tamoxifen chemoprevention. Only women younger than age 40 had a positive risk-benefit index with an average 5-year risk of breast cancer in Korea. Sensitivity analysis showed that this result was robust.
According to the National Surgical Adjuvant Breast and Bowel Project P1 (NSABP-P1) study [1], tamoxifen can prevent 49% of invasive breast cancer in patients who have a 5-year risk of 1.67% or more. Based on this study, the U.S. Food and Drug Administration (FDA) approved tamoxifen as a preventive agent for breast cancer. However, many doctors and patients are reluctant to take tamoxifen for prevention because of its life threatening side effects. Tamoxifen increases the risk of endometrial cancer by 2.53 times, the risk of ischemic stroke by 1.59 times and the risk of pulmonary embolism by 3.01 times [1]. Tamoxifen also has the beneficial effects of preventing osteoporosis, and decreasing the risk of hip fracture by 0.55 times [1].
Gail et al. [2] proposed a risk-benefit index to weigh the risks and benefits of tamoxifen chemoprevention. They showed that tamoxifen was most beneficial for younger women with an elevated risk of breast cancer. They also showed that tamoxifen was not suitable for low-risk older patients.
Korean women have different breast cancer probabilities compared to Western counties [3]. It is not certain that tamoxifen is beneficial to Korean women as a chemopreventive agent. Therefore, we estimated the risks and benefits of tamoxifen using a Korean database in order to evaluate the feasibility of using tamoxifen for chemoprevention in Korean women.
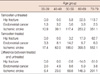
To calculate a risk-benefit index of preventive tamoxifen, we used different data sources. For the preventive effects of tamoxifen, we could not know the exact chemopreventive effects of tamoxifen for Korean women because there were no prospective randomized controlled studies about tamoxifen chemoprevention in Korea. Therefore, we assumed that the effect of tamoxifen on Korean women was the same as on U.S. women. We used the relative risks of breast cancer, hip fracture, endometrial cancer and ischemic stroke from the NSABP-P1 study [1]. We summarized assumed relative risks with 95% confidence intervals in Table 1.
The incidence rates of hip fracture for Korean women were obtained from the study [4] that used the Korean National Health Insurance database. We re-calculated the incidence rate of female hip fractures according to 10-year age intervals [4]. There was no data under the age of 50, but a hip fracture at a young age is a rare event. So we assumed that the incidence is zero for those under age 50.
The incidence rates of stroke were obtained from another study [5] that also used the Korean National Health Insurance database. That study showed the 10-year probability of stroke per hundred individuals calculated for five-year age intervals. We re-calculated the incidence rate of female stroke according to the 10 year age intervals. Among those with cerebrovascular stroke, tamoxifen increases the incidence of ischemic stroke, but not hemorrhagic stroke. In the same study [5], the proportion of patients with an ischemic stroke was 58.9% of all females who had strokes. So we multiplied 0.589 by the incidence of strokes.
For the incidence rates of endometrial cancer, we used age-specific endometrial cancer incidence rates from the Korea Central Cancer Registry data [6].
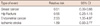
The overall mortality rates and cause-specific mortality rates for patients with endometrial cancer and ischemic stroke were obtained from statistics on cause-specific death from the Korea National Statistical Office [7]. We searched the web-based Korea National Statistical Office's database by the International Classification of Disease (ICD)-10 diagnostic codes I63 for ischemic stroke and C54, C55 for endometrial cancer. The mortality rates for hip fracture were obtained from the hip fracture study [4]. The incidence rates and the mortality rates of hip fracture, endometrial cancer and ischemic stroke are summarized in Table 2.
To calculate the expected number of invasive breast cancer prevented over a 5-year period, we multiplied the estimated 5-year risk of invasive breast cancer by the relative risk reduced by tamoxifen. For example, if the 5-year risk of invasive breast cancer is 1%, it means that 100 breast cancers will occur among 10,000 people over a 5-year period. If they take a tamoxifen for prevention, 49 breast cancers will be prevented because the assumed relative risk of breast cancer is 0.51. The 5-year risk of invasive breast cancer was calculated by the Korean breast cancer risk assessment tool [3], a web-based breast cancer risk assessment tool for Korean women. In the tool, the risk factors for breast cancer (age, family history, body mass index, age of first delivery, breast feeding history and breast biopsy history) are entered, and breast cancer risk in the following 5 years and 10 years, and up to ages 64 and 74 years are calculated.
To calculate the expected number of hip fractures, endometrial cancers and ischemic strokes, we used Equation 1 which is the same method as that of Gail et al. [2]. In equation 1, the hazard rate means the incidence rate multiplied by the relative risk in Table 1. In tamoxifen untreated people, the relative risk is one, so the hazard rate is the same as the incidence rate. Mortality rates from other causes were calculated by subtraction of cause-specific mortality rates from overall mortality rates. In Table 3, we summarized the calculated number of hip fractures, endometrial cancers and ischemic strokes in the tamoxifen untreated and treated groups. The differences between tamoxifen treated and untreated cases also summarized. We compared these results with the results of Gail et al. [2] for U.S. women.
(Equation 1)
Expected number of non-breast event over 5 years
= hazard rate / (hazard rate + mortality rate from other causes) × [1 - exp{-5 × (hazard rate + mortality rate from other causes)}]
To estimate the risks and benefits of tamoxifen chemoprevention, we followed the methods of Gail et al. [2]. Life-threatening events related to tamoxifen are invasive breast cancer, hip fracture, endometrial cancer and stroke. The benefits of tamoxifen are prevention of both invasive breast cancer and hip fracture. The risks of tamoxifen are endometrial cancer and stroke (Figure 1). To summarize the risks and benefits of tamoxifen in a single number, we defined the risk-benefit index as follows:
(Equation 2)
Risk-benefit index
= expected number of invasive breast cancer prevented + expected number of hip fracture prevented - expected number of endometrial cancer - expected number of stroke
As the study of Gail et al. [2] suggested, we assumed that the magnitude of each event of breast cancer, hip fracture, endometrial cancer and stroke was the same. For example, one case of endometrial cancer that occurs is equivalent to one case of breast cancer prevented. If the risk-benefit index is negative, it shows that tamoxifen has more risk than benefit. For women with a previous history of hysterectomy, there is no risk of endometrial cancer. So we calculated this separately for women with a hysterectomy without adding the risk of endometrial cancer. We calculated the risk-benefit index for average 5-year risk of breast cancer according to the study of Kim et al. [3].
We assumed that the effect of tamoxifen on Koreans was the same as on the U.S. women and used the relative risks of breast cancer, hip fracture, endometrial cancer and ischemic stroke from NSABP-P1. But it was not certain that the effect of tamoxifen on Korean women was the same as for U.S. women. So we conducted sensitivity analyses in which we varied our assumptions regarding the relative risks of breast cancer, hip fracture, endometrial cancer and ischemic stroke. We calculated the 5-year risk of breast cancer for specific age groups when the risk-benefit index was zero, which meant that the risk and the benefit for tamoxifen was the same. In one-way sensitivity analysis, each parameter of relative risk of breast cancer, hip fracture, endometrial cancer and ischemic stroke was varied separately from the lower limit to the upper limit of the 95% confidence interval. Then, we conducted sensitivity analysis including all relative risks in the same way.
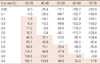
The expected numbers of hip fractures, endometrial cancers and ischemic strokes were calculated using Equation 1. The expected numbers of hip fractures and ischemic strokes increased with age (Table 3). The expected number of endometrial cancers is highest in the sixth decade of life.
From the results of the study of Gail et al. [2], the expected numbers of hip fractures per 10,000 in tamoxifen untreated U.S. white women were 50 for women in their 50s, 116 for women in their 60s and 339 those in their 70s. For endometrial cancers, the expected numbers of the same U.S. white women were 10 for those in their 40s, 40 for those in their 50s, 70 for their 60s and 75 for their 70s. For ischemic strokes, the expected numbers of the same U.S. white women were 22 for ages 40-49, 54 for 50-59, 156 for 60-69, and 342 for age 70 and over. Expected numbers of hip fractures and endometrial cancers were lower in Korean women than in U.S. white women, but the expected number of ischemic strokes was much higher in Korean women.
The expected number of hip fractures was decreased by tamoxifen, but the expected numbers of endometrial cancers and ischemic strokes were increased by tamoxifen (Table 3). The number of ischemic strokes dramatically increased with age. This increase was exaggerated with tamoxifen treatment (Table 3). The magnitude of endometrial cancer was smaller than that of hip fractures or ischemic strokes induced by tamoxifen.
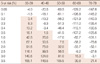
The risk-benefit index was calculated using Equation 2. In Tables 4 and 5, the shaded area shows a positive risk-benefit index that has more benefits than risks. For the specific 5-year risk of breast cancer, the net benefit of tamoxifen was reduced according to increases with age because of the high risk of stroke in older women. So older Korean women had more risk than benefit from tamoxifen chemoprevention.
Comparing non-hysterectomy (Table 4) and hysterectomy (Table 5) women, there was little difference in the risk-benefit index because the incidence of endometrial cancer was low. The effect of endometrial cancer is smaller than effects of hip fracture or ischemic stroke induced by tamoxifen.
According to the study of Kim et al. [3], the average 5-year risk of breast cancer in Korea was 0.18% for age 35, 0.38% for age 45, and 0.28% for age 55. At that average risk of breast cancer, the risk-benefit index was 0.4, -9.3, and -61.0 for ages 35, 45, and 55, respectively. Therefore, only women younger than age 40 had a positive risk-benefit index for average 5-year risk of breast cancer.
We calculated the 5-year risk of breast cancer at each specific age group when the risk-benefit index was zero, which meant that the risk and benefit from tamoxifen was the same. The numbers were 0.17% for women in their 30s, 0.57% in their 40s, 1.52% in their 50s, 2.81% in their 60s, and 3.14% for women in their 70s. Sensitivity analysis regarding the 95% confidence interval of breast cancer relative risk as parameters, the point was converged as the age decreased. Sensitivity analyses regarding relative risk of hip fracture, endometrial cancer and ischemic stroke showed similar results. Sensitivity analysis that included all relative risks in the same way, also showed similar results (Figure 2). It showed that the result of this study regarding women younger than age 40 is robust.
Since 1999, tamoxifen has been recommended in the U.S. to prevent breast cancer. Of 10 million U.S. women, it was estimated that 2.4 million would benefit from taking tamoxifen for chemoprevention [8]. However, only 0.2% of U.S. women took tamoxifen for chemoprevention in 2000, and only 0.08% of U.S. women took tamoxifen for chemoprevention in 2005 [9]. The decline was due to life-threatening effects of tamoxifen: endometrial cancer, stroke and pulmonary embolism. Therefore, Gail et al. [2] proposed a risk-benefit index of tamoxifen chemoprevention. According to that study, women younger than 50 years old had more benefits than risks. If women had a hysterectomy, there was no risk of endometrial cancer. Therefore, women younger than 60 years old had more benefits than risks.
In Korea, tamoxifen is popular as a therapeutic agent but not as a preventive agent. The incidence of breast cancer in Korean women is much lower than in U.S. women. Therefore, the benefit of tamoxifen for prevention would also be low. This study showed that only Korean women younger than age 40 had a positive risk-benefit index for average 5-year risk of breast cancer.
In this study, we used the relative risks of NSABP-P1 for breast cancer, hip fracture, endometrial cancer and stroke, assuming that the effect of tamoxifen prevention for Korean women was the same as for U.S. women. This point is the most important drawback in this study. In the NSABP-P1 study, Asian Americans were rarely enrolled and there was no evidence of tamoxifen chemoprevention in Korea until now. So we agree on the necessity of doing a tamoxifen chemopreventive trial for Korean women. This study will be useful to suggest enrollment criteria for a future tamoxifen prevention trial.
Although there is no evidence of tamoxifen preventing breast cancer in Korean women, some high-risk patients are taking tamoxifen for preventive purpose. So a presumptive guideline of preventive tamoxifen is thought to be needed. This study will be useful to guide the use of preventive tamoxifen.
The relative risk of Korean women can be calculated by large sized case-control study. It is possible that using tamoxifen for prevention in Korean women will have different effects than this study. If the relative risks of Korean women are different from those of U.S. women, the results of this study will be wrong. Therefore, we did sensitivity analyses to overcome the uncertainty due to the assumed relative risks. We used the upper and lower limit of the 95% confidence interval of relative risk as input variables. It showed wide ranges of variation among older women, but the range converged for younger women. For women under age 40, there was little change with variation in relative risks. So, we thought that the conclusion of this study regarding women under the age of 40 is reliable.
We did not count pulmonary embolism as a life-threatening effect. Until now, there has been no data on pulmonary embolism incidence in Korea. There is some hospital based data, none from the general population. The incidence of pulmonary embolism in Korea is much lower than in the U.S. population [10]. Therefore, we assumed that pulmonary embolism had little effect on the risk of tamoxifen.
Gail et al. [2] divided the effects of tamoxifen into three categories: life-threatening events, severe events and other events. Invasive breast cancer, hip fracture, endometrial cancer, stroke and pulmonary embolism were included in life-threatening events. They assumed that life-threatening events had the same magnitude of effect on the risk-benefit index. Strictly speaking, each event has different mortality and cost. Furthermore the magnitude of each event is subjective and each woman has different concerns regarding the same event. As they mentioned [2], no standard index would be particularly appropriate. However, they found the benefit of tamoxifen was insensitive to the particular weights used. In particular, breast cancer and endometrial cancer had similar survival rates. So we thought that it was appropriate to use a risk-benefit index of the same magnitude.
Korean women had much higher risk of ischemic stroke than women in the U.S. The risk of stoke increased with age. Therefore, older Korean women had more risk than benefit from tamoxifen chemoprevention. Although this study had some drawbacks, we found that Korean women under age 40 had more benefit than risk from tamoxifen chemoprevention. Tamoxifen chemoprevention should be limited to Korean women younger than age 40.
Figures and Tables
Figure 1
Weighing the life-threatening risks and benefits of tamoxifen chemoprevention for Korean women.

Figure 2
Sensitivity analysis regarding the 95% confidence interval of relative risk as parameters in the women with and without hysterectomy.

Table 3
Calculated numbers of non-breast cancer events expected in 5 years among 10,000 tamoxifen untreated and treated Korean women
References
1. Fisher B, Costantino JP, Wickerham DL, Redmond CK, Kavanah M, Cronin WM, et al. Tamoxifen for prevention of breast cancer: report of the National Surgical Adjuvant Breast and Bowel Project P-1 Study. J Natl Cancer Inst. 1998. 90:1371–1388.

2. Gail MH, Costantino JP, Bryant J, Croyle R, Freedman L, Helzlsouer K, et al. Weighing the risks and benefits of tamoxifen treatment for preventing breast cancer. J Natl Cancer Inst. 1999. 91:1829–1846.

3. Kim SH, Chae YS, Son WJ, Shin DJ, Kim YM, Chang MC. Estimation of individualized probabilities of developing breast cancer for Korean women. J Korean Surg Soc. 2008. 74:405–411.
4. Kang HY, Yang KH, Kim YN, Moon SH, Choi WJ, Kang DR, et al. Incidence and mortality of hip fracture among the elderly population in South Korea: a population-based study using the national health insurance claims data. BMC Public Health. 2010. 10:230.

5. Jee SH, Park JW, Lee SY, Nam BH, Ryu HG, Kim SY, et al. Stroke risk prediction model: a risk profile from the Korean study. Atherosclerosis. 2008. 197:318–325.

6. Ministry for Health, Welfare and Family Affairs, Korea Central Cancer Registry. Cancer Incidence in Korea 1999-2002. 2008. Goyang: Korea Central Cancer Registry;76–77.
7. Statistics of deaths by cause. Korean Statistical Information Service. Accessed August 1st, 2011. http://www.kosis.kr/.
8. Freedman AN, Graubard BI, Rao SR, McCaskill-Stevens W, Ballard-Barbash R, Gail MH. Estimates of the number of US women who could benefit from tamoxifen for breast cancer chemoprevention. J Natl Cancer Inst. 2003. 95:526–532.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download