Abstract
Purpose
Breast-conserving surgery (BCS) with radiotherapy has become a standard treatment for early stage breast cancer, since the installation of NSABP B-06. One of the serious problems in BCS is that of local recurrence. There are many risk factors for local recurrence, such as large tumor size, multiple tumors, axillary lymph node involvement, young age, high nuclear grade, and so on. The aim of this study is to identify patients with a higher risk of local recurrence of breast cancer.
Methods
Between January 2002 and December 2006, 447 patients with breast cancer, and who had undergone BCS with immediate breast reconstruction, were enrolled in the study. The follow-up period was 5 years from the time of operation and we analyzed local recurrence, disease-free survival (DFS), and overall survival (OS). The analysis included various clinicopathological factors such as age, chemotherapy, radiotherapy, hormone therapy, pathologic characteristics, and margin status. Statistical analysis was performed with log-rank test and Kaplan-Meier method. The p-value <0.05 was considered statistically significant.
Results
The mean follow-up period was 88 months and local recurrence of breast cancer occurred only in 16 cases (3.6%). The actual 5-year DFS, and OS rates were 90.6% and 93.3%, respectively. For the local recurrence of breast cancer, positive margin status, multiple margin positivity, conversed margin cases, T/N stages showed statistical significance in univariate analysis. However, only multiple margin positivity was identified as an independent risk factor for local recurrence in multivariate analysis.
Breast-conserving surgery with radiotherapy has become a standard treatment for early breast cancer since the treatment was determined to have an equivalent survival rate to mastectomy [1-4]. One of the serious problems in breast-conserving surgery is local recurrence and hence, the most important factor for successful breast-conserving surgery is the complete resection of the tumor.
The local recurrence rate (LRR) of breast cancer has been reported as 3% to 20% [5-9]. Although several studies have reported that local recurrence does not greatly influence overall survival (OS), it still poses concerns since re-excision of the tumor is necessary and the incidence of contralateral breast cancer becomes much higher in cases with local recurrence [10].
The risk factors for local recurrence of breast cancer which have been reported include large tumor size [8,11], multifocality [9,12-16], axillary lymph node involvement [11], young age [9,17,18], high nuclear grade [12,19], extent of the intraductal component and positive surgical margin status. Among these, the most important factor involved in local recurrence is positive surgical margin status [7,9]. In order to perform a complete excision with clear resection margin, it is important to secure 1 to 2 cm of distance from tumor and perform an intraoperative evaluation of the margin status. When a positive surgical margin is reported on intraoperative frozen biopsy, or when a pathologic report for margin status shows a result to be reversed from negative to positive, re-excision should be performed to prevent local recurrence. These are very stressful situations for both patients and surgical oncologists. Thus, evaluation of the tumor size, number, location, and morphologic features should be done via imaging modalities prior to surgical planning.
The aim of this study was to identify the most important high risk factors for local recurrence of breast cancer. The authors investigated additional risk factors besides those which have been previously suggested and focused on multiple surgical margin positivity.
Between January 2002 and December 2006, the data of 447 patients with breast cancer who underwent breast-conserving surgery were collected for this study. Data were recorded prospectively and were analyzed retrospectively. Exclusion criteria included stage IV breast cancer, synchronous or metachronous malignancy in other organs.
All breast cancer was diagnosed by needle or excision biopsy, and the size, number, and location of the tumor were identified through mammography, ultrasonography, and breast magnetic resonance imaging (MRI) prior to surgery. According to the tumor stage and characteristics, neoadjuvant chemotherapy, adjuvant chemotherapy, radiotherapy, or hormone therapy was applied in each case.
Informed consent was obtained from all patients and the protocol used in this study was approved by the Institutional Review Board Committee of the Pusan National University Hospital (H-1211-005-012).
A follow-up period of 5 years was set up from the time of operation. Local recurrence, disease-free survival (DFS), and OS were investigated during this period. Disease follow-up was performed every 6 months based on blood tests with a tumor marker, chest plain X-ray, mammography, breast and abdomen ultrasonography, bone scan, brain computed tomography (CT), and positron emission tomography/computed tomography (PET/CT).
The patients were divided into two age groups, based on 50 years as the supposed age of menopause. Patients were classified into groups that received neoadjuvant chemotherapy, adjuvant chemotherapy, radiotherapy or hormone therapy. Information from surgical margin status included simple positive results, multiple positive results and conversion cases which were negative in the frozen to positive in the final pathologic report. Surgical margin positivity was defined when the atypical cell, carcinoma in situ or invasive cancer cells existed within 5 mm of the cut surface. Multiple margin positivity was defined when margin positive results was found more than twice in the same site or in more than 2 different sites simultaneously (Figure 1). Basically, negative surgical margin is defined as the margin having at least 5 mm of free distance in the frozen section or in the final pathologic report. Conversion cases which underwent re-operation were included in positive margin cases.
The morphologic features of the tumor margin were classified as round, irregular, spiculated, or amorphous, according to the images on breast MRI. Tumor type, stage, nuclear grade, histologic grade, presence of estrogen receptor or progesterone receptor, HER2/neu gene expression and triple negative were also verified from pathologic reports.
The surgical margin is deemed to be 2 cm from the tumor by preoperative ultrasonography. When the tumor is not palpable, we performed ultrasound-guided H-wire localization not to miss the tumor during operation. Either sentinel node biopsy or axillary lymph node dissection was performed according to the axillary lymph node status. To evaluate the surgical margin status, tissues were obtained using the circumferential method from 12 directions of the surgical cavity. Determination of the surgical margin was performed by three different pathologists in random order. Re-excision and secondary margin evaluation were performed when margin positive was diagnosed in the intraoperative frozen section. After the negative results of surgical margin were confirmed, breast reconstruction methods such as local flap, thoraco-epigastric flap, lateral thoracic fasciocutaneous flap, and latissimus dorsi myocutaneous flap were applied according to the volume and location of removed breast tissue.
Statistical analyses were performed with SPSS version 16.0 (SPSS Inc., Chicago, USA). Categorical variables were compared using chi-square test and actual 5-year DFS, and OS was evaluated with the Kaplan-Meier method. Comparison of local recurrence-free survival between 2 groups was examined using the log-rank test in univariate analysis. A Cox proportional hazard model was used to analyze various prognostic factors in multivariate analysis. The p-value <0.05 was considered statistically significant.
The mean age of the patients was 46.6 years (range, 24-75 years) and the mean follow-up period was 88 months. In our study, local recurrence of breast cancer occurred only in 16 cases (3.6%) and actual 5-year DFS, and OS rates were 90.6% and 93.3%, respectively (Figure 2).
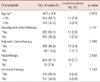
Three hundred four patients (68.0%) were below the age of 50 years, and those under 50 years of age presented with a higher LRR than those over 50 years of age. There was, however, no statistical significance in the LRRs between the two age groups. Neoadjuvant chemotherapy and adjuvant chemotherapy were applied to 282 patients (63.1%) and 406 patients (90.8%), respectively. Moreover, irradiation was applied to nearly all patients (434, 97.1%) after breast-conserving surgery. The local recurrence of breast cancer was identified only in the group who received radiotherapy, and eight cases of local recurrence occurred equally in both groups treated with hormone therapy. These treatment modalities, however, were not statistically significant (Table 1).
The mean tumor size was 2.0 cm and morphological features of the tumor margin were not associated with the local recurrence of breast cancer. However, overall, T and N stages of significantly contributed to the LRR of breast cancer (p<0.001, p=0.001, and p=0.008, respectively). The tumor types were classified as ductal, lobular, mucinous lesion, and others. There were 52 cases (11.6%) of carcinoma in situ and 366 (81.8%) cases of invasive carcinoma lesions. We found no influence of tumor type on the risk of local recurrence.
No differences were found in nuclear grade, histologic grade, lymphovascular invasion, and perineural invasion among the groups. Information of hormone receptors was available in 444 cases (99.3%), but again, no significant differences were found with regard to recurrence. In our study, HER2/neu gene positive rate, and triple negative rate were 25.3% and 14.8%, respectively and this was similar to other previous studies. However, unlike previous reports, HER2/neu positivity or triple negativity did not show a statistically significant association with LRR.
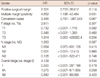
Among 90 cases (20.1%) of positive surgical margin, multiple margin positivity was identified in 37 cases (8.3%). In 10 cases, the final pathologic report was conversed to frozen biopsy results from less to more aggressive lesion. Re-excision was performed in 4 cases and the other 6 cases received only irradiation. There were 10 (11.1%) and 9 (24.3%) cases of local recurrence in margin positive cases and multiple margin positive cases, respectively. Pathologically, LRR after the breast-conserving surgery was attributable to a positive surgical margin, multiple margin positivity and conversion results (p<0.001, p<0.001, and p=0.008, respectively). However, the types of positive margin and multiple margin positivity were not associated with local recurrence (p=0.699, p=0.424) (Table 2).
Among various clinicopathological factors, the margin positive cases and multiple margin positive cases showed statistical significance only with T stage (p=0.019, p=0.011), and the pathologic characteristics of positive margin cases are shown in Table 3.
The adjusted multivariate analysis for risk factor of local recurrence included a positive surgical margin, multiple margin positivity, conversion cases, T stage, N stage and overall stage which showed significance in univariate analysis. However, only multiple margin positivity was an independent risk factor for local recurrence of breast cancer (p=0.031) (Table 4).
In univariate analysis of OS, statistical significance was shown in N stage (p=0.007), overall stage (p<0.001), lymphovascular invasion (p=0.001), and presence of progesterone receptor (p=0.021). However, only N stage and overall stage were associated with OS independently, and the local recurrence was not associated with OS in our study.
LRRs after breast-conserving surgery for breast cancer ranged from 2% to 20% and for early breast cancer were 12% and 20% at 5 and 10 years, respectively [5-9,20,21]. Although previous randomized trials have reported that groups with a high incidence of local recurrence demonstrate the same OS those with a low incidence of local recurrence [1,2], patients with local recurrence of breast cancer experience not only anxiety in relation to the recurrence, but stressful situations such as re-operation, and chemotherapy, etc. Hence, identification of patients with high risk factor of local recurrence is very important.
The risk factors of local recurrence in breast cancer have been reported as young age, large tumor, positive surgical margin, extensive intraductal component, multifocality, axillary lymph node involvement, extranodal extension, and high nuclear grade. Among these factors, positive surgical margin is the most important factor because it is the only factor which can be controlled by surgeons [6].
Generally, breast cancer in young age groups shows more aggressive tumor progression. However, there are some conflicting reports about the incidence of local recurrence between age groups [12,13,17]. In the present study, no difference in local recurrence was found between patients younger than 50 and those older than 50. However, it is difficult to draw conclusions since treatment strategies were not strictly controlled.
Chemotherapy and radiotherapy have been reported to be associated with local control and OS. However, in our study, there was no significant association of the incidence of local recurrence with chemotherapy and radiotherapy. Nevertheless, the result is not reliable because most patients in this study received these treatments.
Several studies reported the margin positive rate in primary excision from 4% to 14% [5,7,9]. When positive surgical margin is diagnosed, surgeons should perform re-excision immediately until the negative result is confirmed. Authors assessed the tumor size and location with preoperative imaging modalities and evaluated the frozen sections for surgical margins. In our study, primary margin positive rate and multiple margin positive rate were 20.1% and 8.3%, respectively. They showed statistical significance with local recurrence of breast cancer in univariate analysis. However, the multiple margin positivity was associated only with pathological T stage, and not with the clinical T stage. The multiple margin positivity was the only independent risk factor of local recurrence in adjusted multivariate analysis. This means that the rate of multiple margin positivity would be more detected in cases of larger pathologic tumors, and that the risk of local recurrence would be higher with inadequate resection, even if surgeons confirmed the negative surgical margin during operation and performed the standard treatments. In these cases, surgeons should consider a much larger scale of surgery or mastectomy to prevent the local recurrence of breast cancer to remove the still remained tumor cells. Of course, for successful results, surgeons and patients should discuss their options before surgery, and the surgeon should ideally be proficient in various oncoplastic techniques.
According to previous reports, multiple margin positivity has been considered as an extensive ductal carcinoma in situ. However, positive results in our study included cases of atypical cells, carcinoma in situ, and invasive carcinoma. Ductal carcinoma in situ showed no significance in our study, in terms of its relationship with either the type of cancer or the stage of cancer.
The surgical margin status has been accepted to be the most important risk factor, because it is the only risk factor which is controllable by surgeons. For the accurate diagnosis of surgical margin, there are several requirements. First, a guideline for the margin status should be established. There is no clear consensus as to the definition of a positive surgical margin. To establish a treatment guideline, an in-depth discussion between surgeons and pathologists, in order to achieve a definition of a positive result is needed. Based on previous reports, it might be reasonable for positive surgical margins to include atypical cells, in situ or invasive cancer cells within 5 mm from cut surface [22-24]. Second, adequate specimens should be obtained. There are some limitations to performing frozen biopsies when margin specimens contain an artifact of electrocautery or fat tissue. Margin tissue should be taken with surgical scissors from the breast parenchyma. Third, the surgical margin evaluation should be performed by surgeons. Only surgeons can recognize correct directions and decide for re-excision. Many authors are using "total-circumference intraoperative frozen method" and taking the tissues from the remnant breast cavity for margin evaluation, due to its varying directions and farther tissues from the tumor [25].
In pathologic assessments, conversion cases which were diagnosed as negative in the frozen, but as positive in the final pathologic report existed. When the surgical procedure is incomplete, re-excision is recommend for more than a focal degree of margin positivity and only irradiation treatment is enough for a focal degree of margin positivity [6]. There were 6 cases with irradiation treatment only in this study, and one case of local recurrence was confirmed during the follow-up. However, conversion case was not considered as an independent risk factor for local recurrence.
Large tumor size, positive lymph nodes, estrogen-negative status, high histologic grade, and lymphovascular invasion are also risk factors for the local recurrence of breast cancer [7,26,27]. Although, overall stage and T/N stages in this study showed statistical significance in univariate analysis, they were not independent factor, and other pathologic characteristics, including hormone status, were not associated with the local recurrence of breast cancer, even in univariate analysis.
The most important point of this study is that multiple margin positivity would be an independent risk factor for the local recurrence of breast cancer, and the identification of tumor size and location, multifocality, and morphologic features of the tumor should be assessed before surgery in order to prevent multiple margin positive cases. However, only a few reports have described multiple margin positivity and they did not suggest guidelines for margin evaluation or treatment strategies.
There are, of course, some limitations in our study. The follow-up period was only 5 years and this was a single institution investigation with a small population. According to the rules of thumb, such as 10 or more events per predictor variable, 16 cases of local recurrence in our study is not a sufficient number for a reliable prediction [28]. Hereafter, if a large population with long term follow-up in multicentric investigation is performed, a much more concrete conclusion will be drawn.
Based on our results, multiple margin positivity of breast cancer is an independent risk factor for the local recurrence of breast cancer. In conclusion, authors recommend a much larger scale of oncoplastic surgery, equivalent to mastectomy, for successful breast-conserving surgery when multiple margin positivity is confirmed.
Figures and Tables
 | Figure 1Definitions of surgical margin status. (A) Negative surgical margin means that the tumor is removed with more than 5 mm of free distances from resection margin. (B) Positive surgical margin (black arrow) is defined as when tumor cells are found on the resection margin. (C) Multiple positive surgical margin (black arrows) is defined as when tumor cells are found on more than two points of the resection margins. |
References
1. Fisher B, Anderson S, Bryant J, Margolese RG, Deutsch M, Fisher ER, et al. Twenty-year follow-up of a randomized trial comparing total mastectomy, lumpectomy, and lumpectomy plus irradiation for the treatment of invasive breast cancer. N Engl J Med. 2002. 347:1233–1241.

2. Veronesi U, Cascinelli N, Mariani L, Greco M, Saccozzi R, Luini A, et al. Twenty-year follow-up of a randomized study comparing breast-conserving surgery with radical mastectomy for early breast cancer. N Engl J Med. 2002. 347:1227–1232.

3. Jacobson JA, Danforth DN, Cowan KH, d'Angelo T, Steinberg SM, Pierce L, et al. Ten-year results of a comparison of conservation with mastectomy in the treatment of stage I and II breast cancer. N Engl J Med. 1995. 332:907–911.

4. van Dongen JA, Voogd AC, Fentiman IS, Legrand C, Sylvester RJ, Tong D, et al. Long-term results of a randomized trial comparing breast-conserving therapy with mastectomy: European Organization for Research and Treatment of Cancer 10801 trial. J Natl Cancer Inst. 2000. 92:1143–1150.

5. Mirza NQ, Vlastos G, Meric F, Buchholz TA, Esnaola N, Singletary SE, et al. Predictors of locoregional recurrence among patients with early-stage breast cancer treated with breast-conserving therapy. Ann Surg Oncol. 2002. 9:256–265.

6. van den Broek N, van der Sangen MJ, van de Poll-Franse LV, van Beek MW, Nieuwenhuijzen GA, Voogd AC. Margin status and the risk of local recurrence after breast-conserving treatment of lobular breast cancer. Breast Cancer Res Treat. 2007. 105:63–68.

7. Ikeda T, Akiyama F, Hiraoka M, Inaji H, Ohuchi N, Takatsuka Y, et al. Surgical margin status as a cause of local failure after breast conserving therapy. Breast Cancer. 1999. 6:93–97.

8. Luini A, Rososchansky J, Gatti G, Zurrida S, Caldarella P, Viale G, et al. The surgical margin status after breast-conserving surgery: discussion of an open issue. Breast Cancer Res Treat. 2009. 113:397–402.

9. Fredriksson I, Liljegren G, Palm-Sjövall M, Arnesson LG, Emdin SO, Fornander T, et al. Risk factors for local recurrence after breast-conserving surgery. Br J Surg. 2003. 90:1093–1102.

10. Kurtz JM, Amalric R, Brandone H, Ayme Y, Spitalier JM. Contralateral breast cancer and other second malignancies in patients treated by breast-conserving therapy with radiation. Int J Radiat Oncol Biol Phys. 1988. 15:277–284.

11. Katz A, Strom EA, Buchholz TA, Thames HD, Smith CD, Jhingran A, et al. Locoregional recurrence patterns after mastectomy and doxorubicin-based chemotherapy: implications for postoperative irradiation. J Clin Oncol. 2000. 18:2817–2827.

12. Kurtz JM, Jacquemier J, Amalric R, Brandone H, Ayme Y, Hans D, et al. Why are local recurrences after breast-conserving therapy more frequent in younger patients? J Clin Oncol. 1990. 8:591–598.

13. Müller A, von Fournier D, Kaufmann M, Otto HF, Abel U. Whole breast irradiation and boost irradiation in breast-conserving therapy based on morphologic findings. Breast Dis. 1989. 2:121–130.
14. Cowen D, Jacquemier J, Houvenaeghel G, Viens P, Puig B, Bardou VJ, et al. Local and distant recurrence after conservative management of "very low-risk" breast cancer are dependent events: a 10-year follow-up. Int J Radiat Oncol Biol Phys. 1998. 41:801–807.

15. Leopold KA, Recht A, Schnitt SJ, Connolly JL, Rose MA, Silver B, et al. Results of conservative surgery and radiation therapy for multiple synchronous cancers of one breast. Int J Radiat Oncol Biol Phys. 1989. 16:11–16.

16. Kurtz JM, Jacquemier J, Amalric R, Brandone H, Ayme Y, Hans D, et al. Breast-conserving therapy for macroscopically multiple cancers. Ann Surg. 1990. 212:38–44.

17. Calle R, Vilcoq JR, Zafrani B, Vielh P, Fourquet A. Local control and survival of breast cancer treated by limited surgery followed by irradiation. Int J Radiat Oncol Biol Phys. 1986. 12:873–878.

18. Stotter AT, McNeese MD, Ames FC, Oswald MJ, Ellerbroek NA. Predicting the rate and extent of locoregional failure after breast conservation therapy for early breast cancer. Cancer. 1989. 64:2217–2225.

19. Clark RM, McCulloch PB, Levine MN, Lipa M, Wilkinson RH, Mahoney LJ, et al. Randomized clinical trial to assess the effectiveness of breast irradiation following lumpectomy and axillary dissection for node-negative breast cancer. J Natl Cancer Inst. 1992. 84:683–689.

20. Straus K, Lichter A, Lippman M, Danforth D, Swain S, Cowan K, et al. Results of the National Cancer Institute early breast cancer trial. J Natl Cancer Inst Monogr. 1992. (11):27–32.
21. Veronesi U, Banfi A, Salvadori B, Luini A, Saccozzi R, Zucali R, et al. Breast conservation is the treatment of choice in small breast cancer: long-term results of a randomized trial. Eur J Cancer. 1990. 26:668–670.

22. Vicini FA, Kestin LL, Goldstein NS, Baglan KL, Pettinga JE, Martinez AA. Relationship between excision volume, margin status, and tumor size with the development of local recurrence in patients with ductal carcinoma-in-situ treated with breast-conserving therapy. J Surg Oncol. 2001. 76:245–254.

23. Taghian A, Mohiuddin M, Jagsi R, Goldberg S, Ceilley E, Powell S. Current perceptions regarding surgical margin status after breast-conserving therapy: results of a survey. Ann Surg. 2005. 241:629–639.

24. Houssami N, Macaskill P, Marinovich ML, Dixon JM, Irwig L, Brennan ME, et al. Meta-analysis of the impact of surgical margins on local recurrence in women with early-stage invasive breast cancer treated with breast-conserving therapy. Eur J Cancer. 2010. 46:3219–3232.

25. Fukamachi K, Ishida T, Usami S, Takeda M, Watanabe M, Sasano H, et al. Total-circumference intraoperative frozen section analysis reduces margin-positive rate in breast-conservation surgery. Jpn J Clin Oncol. 2010. 40:513–520.

26. Carter CL, Allen C, Henson DE. Relation of tumor size, lymph node status, and survival in 24,740 breast cancer cases. Cancer. 1989. 63:181–187.





 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download