Abstract
Purpose
Luminal-type breast cancer has a good prognosis compared to other types, such as human epidermal growth factor receptor 2 and triple negative types. Luminal-type breast cancer is classified into luminal A and B, according to the proliferation index. We investigated the clinicopathological factors that affect the prognosis of the luminal-type subgroups.
Methods
We reviewed the medical records and the pathologic reports of 159 luminal-type breast cancer patients who were treated between February 2005 and November 2007. We divided luminal-type breast cancer into luminal A and B, according to Ki-67 (cutoff value, 14%) and analyzed the clinicopathologic factors, such as age at diagnosis, intensity score of estrogen receptor and progesterone receptor, histologic grade, and Bcl-2. Moreover, we compared the disease-free survival (DFS) of each group.
Results
In the univariate analysis, age (p=0.004), tumor size (p=0.010), lymph node metastasis (p=0.001), and Bcl-2 (p=0.002) were statistically significant factors in luminal-type breast cancer. In the multivariate analysis, lymph node (p=0.049) and Bcl-2 (p=0.034) were significant relevant factors in luminal-type breast cancer. In the subgroup analysis, the increased Bcl-2 (cutoff value, 33%) was related with a longer DFS in the luminal B group (p=0.004).
Traditionally, breast cancer was classified by morphology, and hormonal receptors were thought to be an important prognostic factor. However, among breast cancer patients with homogenous morphology and hormonal receptor, it was known that clinical prognosis can be heterogeneous [1]. The prognosis of breast cancer has been known to be associated with tumor size, nodal status, hormonal receptor status, histologic grade, nuclear grade, human epidermal growth factor receptor 2 (HER2) expression, Ki-67 expression, etc. [2]. However, the numerous studies for gene molecular profiles of breast cancer replaced the traditional prognostic factors these days.
The molecular difference was researched by the gene microarray of breast cancer, and different gene expression profiles were found, which were classified into basal-like type, HER2 type, normal breast-like type and luminal-type. Luminal-type breast cancer was characterized by profiles of estrogen receptor (ER) positive or progesterone receptor (PR) positive; it showed better prognosis than other subtypes, such as basal-like type and HER2 type. Recently, luminal-type breast cancer was classified into types A and B by Ki-67 or HER2 expression [3]. Also, in recent studies, luminal-type A breast cancer has shown better prognosis than luminal-type B [4]. In this study, we analyzed luminal-type breast cancer in order to find out the clinicopathological factors affecting prognosis in luminal-type breast cancer.
We reviewed the clinical data of breast cancer patients who underwent surgery from February 2005 to November 2007. A total of 159 patients with profiles of ER positive or PR positive were classified as having luminal-type breast cancer. They were divided into two subtypes A and B by using a cutoff of 14% for Ki-67. The cutoff value of Ki-67 was determined such that it was an optimal value relevant to disease-free survival (DFS) of luminal-type breast cancer in other previous studies [5-7]. We analyzed the clinicopathological factors affecting the prognosis of both groups. Approval of the present study was obtained from the Institutional Review Board (SP IRB 12-076).
The clinicopathological factors contained age at diagnosis, tumor size, lymph node metastasis, histologic grade, ER, PR, Bcl-2, adjuvant chemotherapy, radiotherapy, and endocrine therapy. Age at diagnosis was set at 35 years and tumor size was set at 2 cm. Lymph node metastasis was classified by being either positive or negative. Histologic grade was classified into stages I, II, and III by the Modified Bloom and Richardson's histologic grade. ER and PR were classified by the intensity (0, 1+, 2+, 3+) and proportion (%), and Bcl-2 was classified by the cutoff value of 33% expression. Prognosis of patients was determined by the DFS. According to these standards, we analyzed the differences of DFS and the associated clinicopathological factors between subtypes A and B.
Liquid mouse monoclonal antibody ER NCL-1-ER-6F11 (Leica Microsystems Inc., Newcastle Upon Tyne, UK) and PR NCL-L-PGR-312 (Leica Microsystems Inc.) diluted 1:80 with normal goat serum (NGS diluted 1 in 5 TBS) were used as the primary antibody for the ER and PR assay. The secondary antibody was goat anti-mouse peroxidase conjugated immunoglobulines, we used the 3, 3'-diaminobenzidine tetrahydrochloride (DAB) as the chromogen. ER and PR were scored as 0, 1+, 2+, and 3+ according to the intensity with the description of the percentage in regards to the proportion of stained nuclei in 10 high power fields. The ER and PR positivities were defined as any positive scores or percentages over zero.
IHC for Bcl-2 and Ki-67 was performed by the avidin-biotin peroxidase complex method with aminoethylcarbazole as a chromogen using the Vectastain ABC Elite kit (Vector Laboratories, Burlingame, USA). The sections were counterstained with Mayer's hematoxylin. For the Bcl-2 measurement, the sections were incubated in monoclonal mouse anti-human Bcl-2 oncoprotein (1:100; Dako, Glostrup, Denmark), and brown nuclear immunostaining was examined. For the Ki-67 measurement, the sections were incubated with monoclonal mouse anti-human Ki-67 antigen (1:100; Dako), and brown nuclear immunostaining was examined. Ki-67 of >14% and Bcl-2 of >33% were considered as positive expressions.
IHC of HER2/neu protein were performed on 4 µm thick paraffin embedded tissue sections placed on poly-L-Lysine coated slides. After deparaffinization and blocking of the endogenous peroxidase, HER2/neu immunostaining was performed using rabbit anti-human c-erbB-2 oncoprotein as the primary antibody (Dako, Copenhagen, Denmark) at 1:100 dilution. Binding of the primary antibody was checked by Dako Quick-Staining, Labelled Streptavidin-Biotin System (LSAB; Dako, Carpentaria, USA), followed by the addition of diaminobenzidine (DAB) as a chromogen. Each slide was scored in a blinded fashion by two pathologists according to the manufacturer's recommended criteria. The immunostaining was read in a semiquantitative manner and was graded as follows: 0, 1+, 2+, and 3+. Intensity scores of 0 or 1+ were designated as negative expression and 3+ were designated as positive expression for HER2/neu. Scores of 2+ were taken as equivocal cases, which were further recommended for the fluorescence in situ hybridization (FISH) analysis.
Two-color FISH was conducted on 3.5 µm consecutive sections of the TMA paraffin blocks using 20 µL of LSI HER2/CEP17 probes (Vysis Inc., Downers Grove, USA). At least a 2-fold increase of the HER2 signals over the CEP 17 signals using the LSI HER2 probe in the tumor cell was considered as the criterion for gene amplification.
Pearson's chi-square test was used for the univariate analysis in order to analyze the clinicopathological factors affecting the prognosis between subtypes A and B. Logistic regression was used for the multivariate analysis. The difference of DFS between subtypes A and B was analyzed by the Kaplan-Meier method. In each luminal A and B breast cancer groups, the univariate analysis of clinicopathological factors affecting the prognosis was conducted by the Log-rank test; moreover, the multivariate analysis was administered by the Cox multivariate regression model. The SAS software (SAS 9.0; SAS Institute Inc., Cary, USA) was used for the statistical analysis. Results that had p-value <0.05 were statistically significant.
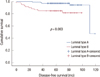
In a total of 159 patients, 99 patients were diagnosed with luminal-type A breast cancer and 60 patients were diagnosed with luminal-type B breast cancer. Breast-conserving surgery (BCS) was performed on 90 patients (56.7%) and mastectomy was performed on 69 patients (43.3%) (Table 1). Further, the median follow-up period was 65.9 months (range, 7-95 months). Adjuvant management contained chemotherapy, radiotherapy, endocrine therapy. Chemotherapy was performed on 121 patients (76.1%) and not on 38 patients (33.9%). Radiotherapy was conducted on 80 patients (50.3%) and not on 79 patients (49.7%). Endocrine therapy was performed on 143 patients (89.9%) and not on 16 patients (10.1%). Luminal-type A breast cancer group had longer DFS than luminal-type B breast cancer group with statistical significance (p=0.003) (Figure 1). The receiver operating characteristic curve of Ki-67 suggested the cutoff value was at 10%, 14%, and 20%. Also, the optimal cutoff value was 14% because the widest area under the curve was seen at 14% (Figure 2).
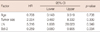
When we compared the luminal-type A group and the luminal-type B group, the proportion of the Bcl-2 high expression (>33%) (p=0.013) rate and the small size tumor (≤2 cm) (p=0.001) increased significantly in the luminal-type A group. The proportion of lymph node (LN) metastasis positive (p=0.033) and histologic high grade (p<0.001) rate increased significantly in the luminal-type B group (Table 1). In the luminal-type breast cancer group, patients in the age group of over 35 years showed longer DFS than the younger age group (p=0.004) and the small tumor size group (≤2 cm) also showed longer DFS than the group with a tumor size over 2 cm (p=0.010). The lymph node metastasis negative group showed longer DFS than the node positive group. Moreover, the high Bcl-2 expression group (>33%) showed longer DFS than the low expression group (p=0.002) (Table 2). In the multivariate analysis, nodal status and Bcl-2 expression were statistically significant relevant factors in the luminal-type breast cancer group (Table 3).
In the subgroup analysis with luminal A group, age at diagnosis (p=0.001), tumor size (p=0.045) and LN metastasis (p=0.004) were statistically significant factors to affect DFS in the univariate analysis, but not in the multivariate analysis (p=0.240) (Table 4). The younger age group (age ≤35 years) showed longer DFS (p=0.001). The smaller tumor size group (≤2 cm) (p=0.045) and the LN metastasis negative group (p=0.004) also showed longer DFS (Table 4).
In the luminal B group, Bcl-2 expression (p=0.004) was the only statistically significant factor affecting DFS in the univariate analysis (Table 5). Additionally, in the multivariate analysis to the luminal B group, Bcl-2 expression was a statistically significant independent factor (p=0.012). Further, Bcl-2 expression over 33% (p=0.004) showed longer DFS curve (Figure 1). In the luminal A group, Bcl-2 expression (p=0.867) was not a statistically significant factor (Table 4) and thus, had no statistically difference in DFS (p=0.89) (Figure 3).
Breast cancer is a heterogeneous disease and shows various clinical courses within the same molecular subtype. Perou et al. [8] classified breast cancer into several subgroups, such as normal-like breast type, luminal-type, HER2 type and basal-like type, according to gene profile. In addition, Brenton et al. [4] also reported that the prognosis of breast cancer differs according to its genotype. Luminal-type breast cancer showed better prognosis than other subtypes, and additionally, when we divide luminal-type breast cancer to types A and B by Ki-67 expression (cutoff value, 14%), luminal-type A (Ki-67 ≤14%) breast cancer showed a lower relapse risk and a longer survival period than luminal-type B (Ki-67 >14%) breast cancer. Additionally, luminal-type B breast cancer showed poor prognosis than luminal-type A breast cancer, but showed better response to systemic chemotherapy. Also, ER-positive tumors responded better to endocrine therapy. Furthermore, up to 80% of patients with ER and PR-positive tumors, whose profile of luminal type breast cancer responding to endocrine therapy, compared to less than 10% of patients with ER and PR-negative tumors [9-11]. In our study, luminal-type A breast cancer showed longer DFS than luminal-type B breast cancer and was statistically significant; it also increased the proportion of the low histologic grade.
Bcl-2 protein is known to be an anti-apoptotic factor in the cell cycle and it also related to poor prognosis in many other malignancies. Target therapy to Bcl-2 has been attempted consistently in order to apply for clinical use in many areas such as chronic myeloid leukemia, malignant melanoma, multiple myeloma, etc. [12,13]. However, in breast cancer, the expression of Bcl-2 has been reported to be a good prognostic factor related with ER positive, high nuclear grade, low histologic grade and HER2 negative [2,14,15].
Elledge et al. [16] and Kim et al. [17] reported that Bcl-2 expression is associated with the prognosis and expression of ER and PR in breast cancer patients undergoing hormonal therapy. Ali et al. [18] investigated the expression of Ki-67 and Bcl-2 in ER positive breast cancer. They reported that Ki-67/Bcl-2 index is associated with breast cancer-specific survival as well as with the significant prognostic factor in ER positive breast cancer, and also has a strong relationship to luminal-type B breast cancer. In our study, we found that the low Bcl-2 expression group is associated with shorter DFS in luminal-type A breast cancer and luminal-type B breast cancer. Our study suggested that Bcl-2 expression is related to DFS in luminal-type A breast cancer and luminal-type B breast cancer.
Histologic grade was known as the independent prognostic factor in breast cancer [19-23]. In this study, luminal-type B breast cancer showed an increased proportion of high histologic grade and a shorter DFS than luminal-type A breast cancer. However, there is no significant difference in DFS according to histologic grade in the total group and the subgroup analysis. Further study should be performed for the analysis of prognosis according to histologic grade in luminal-type breast cancer.
This study has some limitations, however. First, selection bias was observed in this study. The numbers of patients should be similar for both luminal-type A and luminal-type B groups. Also, the overall survival comparison was not performed due to the limitation in the number of patients and the follow-up period. Therefore, further study with more polished design, such as patient selection, larger patient group, more variant factors and longer follow-up period should be performed.
In summary, luminal-type A breast cancer showed longer DFS than luminal-type B breast cancer, which was related with high grade tumor. Bcl-2 expression was significantly related with DFS in luminal-type breast cancer and its subgroup, such as type B. Therefore, Bcl-2 expression may be a potent prognostic factor in luminal-type breast cancer.
Figures and Tables
 | Figure 2Receiver operating characteristic (ROC) curve of Ki-67 with cutoff value 14% (A), 10% (B), and 20% (C).
AUC=area under the curve.
|
 | Figure 3Disease-free survival curves of luminal-type A (A) and B (B) breast cancer according to Bcl-2. |
Table 2
Analysis of clinicopathologic factors affecting to disease-free survival (DFS) in luminal type breast cancer

References
1. Zaha DC, Lazăr E, Lăzureanu C. Clinicopathologic features and five years survival analysis in molecular subtypes of breast cancer. Rom J Morphol Embryol. 2010. 51:85–89.
2. Kröger N, Milde-Langosch K, Riethdorf S, Schmoor C, Schumacher M, Zander AR, et al. Prognostic and predictive effects of immunohistochemical factors in high-risk primary breast cancer patients. Clin Cancer Res. 2006. 12:159–168.

3. Cheang MC, Chia SK, Voduc D, Gao D, Leung S, Snider J, et al. Ki67 index, HER2 status, and prognosis of patients with luminal B breast cancer. J Natl Cancer Inst. 2009. 101:736–750.

4. Brenton JD, Carey LA, Ahmed AA, Caldas C. Molecular classification and molecular forecasting of breast cancer: ready for clinical application? J Clin Oncol. 2005. 23:7350–7360.

5. Goldhirsch A, Ingle JN, Gelber RD, Coates AS, Thürlimann B, Senn HJ. Panel members. Thresholds for therapies: highlights of the St Gallen International Expert Consensus on the primary therapy of early breast cancer 2009. Ann Oncol. 2009. 20:1319–1329.

6. Ahlin C, Aaltonen K, Amini RM, Nevanlinna H, Fjällskog ML, Blomqvist C. Ki67 and cyclin A as prognostic factors in early breast cancer. What are the optimal cut-off values? Histopathology. 2007. 51:491–498.

7. Neri A, Marrelli D, Pedrazzani C, Caruso S, De Stefano A, Mariani F, et al. Prognostic relevance of proliferative activity evaluated by Mib-1 immunostaining in node negative breast cancer. Eur J Surg Oncol. 2008. 34:1299–1303.

8. Perou CM, Sørlie T, Eisen MB, van de Rijn M, Jeffrey SS, Rees CA, et al. Molecular portraits of human breast tumours. Nature. 2000. 406:747–752.

9. Osborne CK. Steroid hormone receptors in breast cancer management. Breast Cancer Res Treat. 1998. 51:227–238.

10. Hess KR, Pusztai L, Buzdar AU, Hortobagyi GN. Estrogen receptors and distinct patterns of breast cancer relapse. Breast Cancer Res Treat. 2003. 78:105–118.

11. Steroid receptors in breast cancer: an NIH Consensus Development Conference, Bethesda, Maryland, June 27-29, 1979. Cancer. 1980. 46:2759–2963.
12. O'Brien S, Moore JO, Boyd TE, Larratt LM, Skotnicki AB, Koziner B, et al. 5-year survival in patients with relapsed or refractory chronic lymphocytic leukemia in a randomized, phase III trial of fludarabine plus cyclophosphamide with or without oblimersen. J Clin Oncol. 2009. 27:5208–5212.
13. Bedikian AY, Millward M, Pehamberger H, Conry R, Gore M, Trefzer U, et al. Bcl-2 antisense (oblimersen sodium) plus dacarbazine in patients with advanced melanoma: the Oblimersen Melanoma Study Group. J Clin Oncol. 2006. 24:4738–4745.

14. Hellemans P, van Dam PA, Weyler J, van Oosterom AT, Buytaert P, Van Marck E. Prognostic value of bcl-2 expression in invasive breast cancer. Br J Cancer. 1995. 72:354–360.

15. Chen HH, Su WC, Guo HR, Chang TW, Lee WY. p53 and c-erbB-2 but not bcl-2 are predictive of metastasis-free survival in breast cancer patients receiving post-mastectomy adjuvant radiotherapy in Taiwan. Jpn J Clin Oncol. 2002. 32:332–339.

16. Elledge RM, Green S, Howes L, Clark GM, Berardo M, Allred DC, et al. bcl-2, p53, and response to tamoxifen in estrogen receptor-positive metastatic breast cancer: a Southwest Oncology Group study. J Clin Oncol. 1997. 15:1916–1922.

17. Kim K, Chie EK, Han W, Noh DY, Park IA, Oh DY, et al. Prognostic value of p53 and bcl-2 expression in patients treated with breast conservative therapy. J Korean Med Sci. 2010. 25:235–239.

18. Ali HR, Dawson SJ, Blows FM, Provenzano E, Leung S, Nielsen T, et al. A Ki67/BCL2 index based on immunohistochemistry is highly prognostic in ER-positive breast cancer. J Pathol. 2012. 226:97–107.

19. Lundin J, Lundin M, Holli K, Kataja V, Elomaa L, Pylkkänen L, et al. Omission of histologic grading from clinical decision making may result in overuse of adjuvant therapies in breast cancer: results from a nationwide study. J Clin Oncol. 2001. 19:28–36.

20. Trudeau ME, Pritchard KI, Chapman JA, Hanna WM, Kahn HJ, Murray D, et al. Prognostic factors affecting the natural history of node-negative breast cancer. Breast Cancer Res Treat. 2005. 89:35–45.

21. Ivshina AV, George J, Senko O, Mow B, Putti TC, Smeds J, et al. Genetic reclassification of histologic grade delineates new clinical subtypes of breast cancer. Cancer Res. 2006. 66:10292–10301.





 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download