Abstract
Purpose
This study evaluated the treatment results and the necessity to irradiate the supraclavicular lymph node (SCN) region in pathological N0-N1 (pN0-N1) patients with locally advanced breast cancer treated with neoadjuvant chemotherapy (NAC) followed by surgery and radiotherapy (RT).
Methods
Between 1996 and 2008, 184 patients with initial tumor size >5 cm or clinically positive lymph nodes were treated with NAC followed by surgery and RT. Among these patients, we retrospectively reviewed 98 patients with pN0-N1. Mastectomy was performed in 55%. The pathological lymph node stage was N0 in 49% and N1 in 51%. All patients received adjuvant RT to chest wall or breast and 56 patients (57%) also received RT to the SCN region (SCNRT).
Results
At 5 years, locoregional recurrence (LRR)-free survival, distant metastasis-free survival, disease-free survival (DFS), and overall survival rates were 93%, 83%, 81%, and 91%, respectively. In pN0 patients, LRR was 7% in SCNRT- group and 5% in SCNRT+ group. In pN1 patients, LRR was 7% in SCNRT- group and 6% in SCNRT+ group. There was no significant difference of LRR, regardless of SCNRT. However, in pN1 patients, there were more patients with poor prognostic factors in the SCNRT+ group compared to SCNRT- group. These factors might be associated with worse DFS in the SCNRT+ group, even though RT was administered to the SCN region.
Adjuvant radiation therapy (RT) improved locoregional control and overall survival in breast cancer patients treated with upfront surgery, as shown in three randomized trials and one meta-analysis [1-4]. These studies, which routinely included the supraclavicular lymph node (SCN) region in the radiation field of adjuvant RT group, showed that adjuvant RT reduced the locoregional recurrence (LRR) in pathological N1 and N2 (pN1-N2) patients. In contrast, several studies reported SCN recurrence rates as low as 1% to 8% when supraclavicular radiation therapy (SCNRT) was not used in pN0-N1 patients [5-8]. These conflicting findings have resulted in considerable debate regarding the use of SCNRT for pN1 breast cancer patients. Recently, prognostic factors associated with SCN recurrence were identified that might help in the selection of patients who will benefit from SCNRT [9,10].
In locally advanced breast cancer patients, neoadjuvant chemotherapy (NAC) followed by surgery showed similar failure rate and survival rate compared to surgery followed by chemotherapy [11-13]. Although NAC followed by surgery for locally advance breast cancer patients is increased, the indication for adjuvant RT and the optimal radiation field of the regional lymphatics are unclear because approximately 80% to 90% of patients had changes in the pathological extent of tumor compared to clinical tumor extent [11,14,15]. Patients who presented with clinically advanced stage III or IV disease but who subsequently achieved a pathologic complete response (pCR) to NAC still had a high rate of LRR, suggesting that RT should be considered. The National Comprehensive Cancer Network (NCCN) guidelines recommend indication for RT and fields of treatment should be based upon the pretreatment tumor characteristics in patients treated with NAC [16]. The recommended radiation field after NAC followed by surgery is breast or the chest wall and regional lymphatics. Recently, a study reported that isolated breast irradiation was enough for pN0 patients after NAC and breast conserving surgery (BCS) [17].
We retrospectively investigated treatment outcomes according to SCNRT in pN0-N1 patients treated with NAC followed by surgery and adjuvant RT for locally advanced breast cancer and evaluated the necessity to irradiate the SCN region.
We retrospectively reviewed the medical records of breast cancer patients treated with NAC followed by surgery and adjuvant RT for curative intent between 1996 and 2008 at Samsung Medical Center. We found 184 patients with initial tumor size >5 cm or with a clinically positive axillary lymph node involvement without initial SCN or internal mammary lymph node metastasis. Of these, 98 patients with pN0-N1 after NAC were included in this study.
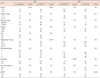
The age at diagnosis ranged from 31 to 67 years (median, 44 years). Invasive ductal carcinoma (80 patients, 82%) was the most common histologic type. Clinical stage and pathological stage were classified according to the seventh edition of American Joint Committee on Cancer (AJCC) Cancer Staging [18]. Clinical tumor size was evaluated with ultrasound. Clinical tumor stage at diagnosis was cT1 in 2 patients (2%), cT2 in 34 (35%), cT3 in 47 (48%), and cT4 in 15 (15%). A clinically axillary lymph node involvement was defined by imaging studies or by clinical examination. Axillary lymph node metastasis was confirmed in 27 patients (32%) by ultrasound guided fine needle aspiration biopsy. Eighty-five patients (87%) had initially axillary lymph node metastasis. NAC involved anthracycline-based drugs in 42 patients (43%), taxane-based drugs in 9 patients (9%), and combined anthacycline-taxane in 47 patients (48%), with a median of three NAC cycles (1-8 cycles). Modified radical mastectomy (MRM) was performed in 54 patients (55%) and BCS was performed in 44 patients (45%). The median number of dissected axillary lymph nodes was 17 (range, 4-42). The pCR in both the primary tumor and axillary lymph nodes was achieved in 11 patients (11%). The pathological stage was 0 in 15 patients (15%), I in 20 patients (21%), II in 49 patients (50%), and III in 14 patients (14%). Adjuvant chemotherapy was administered to 79 patients (81%). Hormone therapy was administered to 52 patients (53%). Patients' characteristics are summarized in Table 1.
All patients received adjuvant RT to the breast or chest wall in tangential fields with a median dose of 50 Gy (range, 50-50.4 Gy) at 1.8 to 2 Gy per fraction using 4- or 6-megavolt photon beams. All patients who received whole breast irradiation also received an electron boost to the tumor bed (median dose 9 Gy, in 3 fractions). Internal mammary lymph node irradiation was not administered. Because of lack of consensus on the RT field after NAC, individual clinicians decided whether RT would be applied to the SCN region. RT to the SCN region was administered to 56 patients (57%) (SCNRT+ group), while 42 (43%) received RT to the breast or chest wall only (SCNRT- group). In the SCNRT+ group, the SCNRT dose was 50 Gy in 25 fractions. Table 1 shows patients characteristics between the SCNRT+ and SCNRT- groups.
BCS was more common in the SCNRT- group. Patients with the SCNRT+ group had more advanced cT and pathological tumor stage (pT), pN, and pathological stage. The SCNRT- group had lower frequencies of a multiplicity and lymphovascular space invasion.
We defined LRR as the appearance of local or regional tumor in the ipsilateral breast, chest wall, axilla, internal mammary, supraclavicular or infraclavicular area. SCN recurrence was defined as any tumor recurrence in the supraclavicular or infraclavicular area. Distant metastasis (DM) was defined as any recurrence other than LRR. LRR was confirmed using cytological aspiration or surgical excision.
We compared the characteristics of the SCNRT+ and SCNRT- groups using a chi-square test or Fisher's exact test if the expected values are below 5. Survival rates were estimated with the Kaplan-Meier method and comparisons between the groups were determined using the log-rank test [19]. We conducted subgroup analysis according to pN status, using Fisher's exact test. All calculations were performed using SPSS version 13.0 (SPSS Inc., Chicago, USA), and statistical significance was accepted for p-values of <0.05.
The median follow-up period from the date of first cycle NAC was 42 months (range, 10-139 months). During follow-up, 19 patients (19%) experienced failure, 6 had LRR, and 18 had DM. Among 6 patients with LRR, 5 patients had both LRR and DM; of these, 4 had synchronous LRR and DM. The remaining 1 patient had LRR only at the ipsilateral SCN. LRR sites were chest wall in 1 patient, axillary lymph node in 1 patient, internal mammary lymph node in 1 patient, and SCN in 3 patients. Recurrence at the SCN was developed in 1 patient in the SCNRT- group and 2 patients in the SCNRT+ group. No additional SCN recurrence was observed after first failure detection.
At 5-years, the LRR-free survival (LRRFS) rate, the DM-free survival (DMFS) rate, and the disease-free survival (DFS) rate were 93%, 83%, and 81%, respectively. The overall survival (OS) rate at 5-years was 91%. On univariate analysis, patients' age, surgery type, pT, pN, pathological stage, multiplicity, hormone treatment and SCNRT were significant factors for survivals (Table 2). According to the SCNRT, 5-year DFS was 72% and 92% in the SCNRT+ and SCNRT- groups, respectively.
Table 3 shows the patients' characteristics between the SCNRT- and SCNRT+ groups according to pN stage. In 48 patients with pN0 after NAC, there was no significant difference in prognostic factors between the SCNRT- and SCNRT+ groups except surgery type (MRM vs. BCS). Locoregional recurrence was 7% in SCNRT- group and 5% in SCNRT+ group. Patients' age was the only significant factor for LRRFS (Table 4). Surgery type and pT were significant factors for DFS. The patients with pN0 had similar LRRFS and DFS, regardless of SCNRT (Figure 1).
In 50 patients with pN1 after NAC, there was a significant difference in prognostic factors between the SCNRT- and SCNRT+ groups. SCNRT+ group had more advanced cT, more frequent multiplicity and more advanced pathological stage. Especially, all patients with pathologic stage III received RT to the SCN region. Locoregional recurrence was 7% in SCNRT- group and 6% in SCNRT+ group. Multiplicity was the only significant factor for LRRFS. Clinical tumor stage and SCNRT were significant factors for DFS. The patients with pN1 had similar LRRFS, regardless of SCNRT, but worse DFS in SCNRT+ groups (Figure 2).
Our study showed favorable survival rates for NAC followed by surgery compared to those of published randomized studies such as the National Surgical Adjuvant Breast and Bowel Project (NSABP) B-18 and the European Organization of Research and Treatment of Cancer (EORTC) 10902 trials [11,13]. These previous studies reported approximately 10% LRR. Recent studies reported a good response to NAC with lower LRR rates. McGuire et al. [20] investigated the role of postmastectomy RT in patients with breast cancer who achieved a pCR to NAC. They reported 10-year LRR rates in patients with breast cancer who achieved a pCR to NAC and received adjuvant RT and in nonirradiated patients were 5% and 10%, respectively. Le Scodan et al. [21] evaluated the effect of postmastectomy RT in stage II-III breast cancer patients with pN0 after NAC and reported that 10 patients (8%) developed LRR; 3 patients (4%) who received RT and 7 (12%) who did not. The results showed no increase in the risk of LRR, DM or death when RT was omitted. We observed 6% overall LRR in patients with N0-N1 after NAC followed by surgery and adjuvant RT; 3 patients (7%) in the SCNRT- group and 3 patients (5%) in the SCNRT+ group, demonstrating similar locoregional control to that observed in previous studies.
NAC is commonly used to increase the chance for breast conservation and to intend to improve treatment outcome, especially for stage II and III breast cancer. After NAC, approximately 80% to 90% of patients have changes in the pathologic extent of the tumor and roughly 20% patients showed eradication of disease within the lymph nodes [11,14,15]. Consequently the indication of adjuvant RT and the role of the regional lymphatics for patients treated with NAC are still unclear. Until now, there are no prospective randomized trials to define the RT indication and the optimal RT field after NAC followed by surgery. NCCN guidelines recommend adjuvant RT according to prechemotherapy tumor characteristics. The MD Anderson Cancer Center, published a paper on retrospective treatment outcomes for adjuvant RT after NAC, reported that patients treated with MRM received comprehensive regional nodal irradiation consisting of SCN and internal mammary chain fields even if pCR is achieved after NAC. For patients treated with BCS, regional nodal radiation was delivered at the discretion of the radiation oncologist [20,22,23]. Generally, patients treated with BCS receive regional nodal irradiation. Min et al. [24], who reported LRR in patients with BCS and RT following NAC, treated the SCN region in all patients. LRR occurred in 26 patients (10%); of these, 4 (2%) showed SCN recurrence. Recently, only one study addressed the optimal radiation field for the regional lymphatics in breast cancer patients after NAC. Daveau et al. [17] retrospectively investigated the role of regional lymph node irradiation in clinical stage II and III breast patients with pN0 after NAC and BCS. They limited the study to patients treated with BCS, because all who were selected for postmastectomy RT underwent both chest wall and lymph node irradiation. LRR occurred in 46 patients (19%) and the 5-year LRRFS and OS rates were 89% and 89% with regional lymph node irradiation, 86% and 92% without regional lymph node irradiation, respectively, and the differences were not statistically significant. They concluded that isolated breast irradiation did not appear to be associated with a higher risk of LRR or death among cN0 to cN2 breast cancer patients with pN0 after NAC. Our study included patients who received BCS or MRM and pN1 patients after NAC. Our results showed lower LRR (6%), even though patients with more advanced disease were analyzed, and SCNRT did not affect LRR in patients with pN0-N1 after NAC.
A few studies reported the prognostic factors for LRR in breast cancer after NAC. The adjuvant RT after NAC followed by mastectomy was needed in patients with cT3 or cT4 tumors, stage IIB disease, pathological tumor size >2 cm, or four or more positive nodes [20,22]. Huang et al. [23] reported four prognostic factors for LRR: cN2 or cN3, lymphovascular space invasion, pathological tumor size >2 cm or multiplicity, assigning one point for the presence of each factor. For patients with a score of 3 to 4, LRR was significantly lower for those treated with MRM vs. BCS (19% vs. 61%, p=0.009). Min et al. [24] found that pN and hormone treatment were significant prognostic factors for LRR on both univariate and multivariate analysis. Our study found no significant factors affecting LRRFS. In addition to the known prognostic factors of pT, pN, pathological stage and multiplicity, the SCNRT+ group paradoxically showed worse DFS because the SCNRT+ group had more unfavorable prognostic factors compared to the SCNRT- group. However, in pN0 patients after NAC, the patients were evenly distributed in clinicopathologic characteristics according to SCNRT. There was no difference in LRRFS and DFS.
Our study has some limitations. First, this study was a retrospective analysis in which RT to the SCN region was not randomized. Second, this study had a small sample size and low LRR. Because of the limited number of patients and events for subgroup analysis, we could not define which pathologic group would not need for SCNRT after NAC.
In conclusion, LRR was similar regardless of SCNRT in pN0-N1 breast cancer patients after NAC followed by surgery. According to subgroup analysis, there was no significant difference in prognostic factors and survivals in pN0 patients between the SCNRT+ and SCNRT- groups. In pN1 patients, the SCNRT+ group had poorer prognostic factors compared to the SCNRT- group and worse survivals, even though RT was administered to the SCN region. Prospective randomized trial is called for to validate the role of SCNRT.
Figures and Tables
 | Figure 1Locoregional recurrence-free survival rate (A) and disease-free survival rate (B) according to radiation therapy (RT) to the supraclavicular lymph node (SCN) region (SCNRT+ group) or not (SCNRT- group) in pN0 breast cancer patients after neoadjuvant chemotherapy and followed by surgery and adjuvant RT. |
 | Figure 2Locoregional recurrence-free survival rate (A) and disease-free survival rate (B) according to radiation therapy (RT) to the supraclavicular lymph node (SCN) region (SCNRT+ group) or not (SCNRT- group) in pN1 breast cancer patients after neoadjuvant chemotherapy and followed by surgery and adjuvant RT. |
Table 1
Patients' characteristics

SCNRT=radiotherapy to the supraclavicular lymph node region; NS=not significant; MRM=modified radical mastectomy; BCS=breast conserving surgery; DALN=dissected axillary lymph node; RM=resection margin; IDC=invasive ductal carcinoma; pCR=pathologic complete response; LVI=lymphovascularspace invasion; ER=estrogen receptor; PR=progesterone receptor.
*Others include positive or close (≤1 mm) resection margin; †Others include invasive lobular carcinoma, infiltrating cribriform carcinoma, invasive micropapillary carcinoma, mucinous carcinoma, infiltrating apocrine carcinoma, and metaplastic carcinoma.
Table 2
Univariate analysis of locoregional recurrence-free survival (LRRFS), disease-free survival (DFS), and overall survival (OS)

References
1. Overgaard M, Hansen PS, Overgaard J, Rose C, Andersson M, Bach F, et al. Danish Breast Cancer Cooperative Group 82b Trial. Postoperative radiotherapy in high-risk premenopausal women with breast cancer who receive adjuvant chemotherapy. N Engl J Med. 1997. 337:949–955.

2. Overgaard M, Jensen MB, Overgaard J, Hansen PS, Rose C, Andersson M, et al. Postoperative radiotherapy in high-risk postmenopausal breast-cancer patients given adjuvant tamoxifen: Danish Breast Cancer Cooperative Group DBCG 82c randomised trial. Lancet. 1999. 353:1641–1648.

3. Ragaz J, Olivotto IA, Spinelli JJ, Phillips N, Jackson SM, Wilson KS, et al. Locoregional radiation therapy in patients with high-risk breast cancer receiving adjuvant chemotherapy: 20-year results of the British Columbia randomized trial. J Natl Cancer Inst. 2005. 97:116–126.

4. Clarke M, Collins R, Darby S, Davies C, Elphinstone P, Evans E, et al. Effects of radiotherapy and of differences in the extent of surgery for early breast cancer on local recurrence and 15-year survival: an overview of the randomised trials. Lancet. 2005. 366:2087–2106.

5. Fortin A, Dagnault A, Blondeau L, Vu TT, Larochelle M. The impact of the number of excised axillary nodes and of the percentage of involved nodes on regional nodal failure in patients treated by breast-conserving surgery with or without regional irradiation. Int J Radiat Oncol Biol Phys. 2006. 65:33–39.

6. Galper S, Recht A, Silver B, Manola J, Gelman R, Schnitt SJ, et al. Factors associated with regional nodal failure in patients with early stage breast cancer with 0-3 positive axillary nodes following tangential irradiation alone. Int J Radiat Oncol Biol Phys. 1999. 45:1157–1166.

7. Reddy SG, Kiel KD. Supraclavicular nodal failure in patients with one to three positive axillary lymph nodes treated with breast conserving surgery and breast irradiation, without supraclavicular node radiation. Breast J. 2007. 13:12–18.

8. Strom EA, Woodward WA, Katz A, Buchholz TA, Perkins GH, Jhingran A, et al. Clinical investigation: regional nodal failure patterns in breast cancer patients treated with mastectomy without radiotherapy. Int J Radiat Oncol Biol Phys. 2005. 63:1508–1513.

9. National Institute for Health and Clinical Excellence. Early and Locally Advanced Breast Cancer: Diagnosis and Treatment: NICE Clinical Guidelines 80. 2009. London: National Institute for Health and Clinical Excellence.
10. Yu JI, Park W, Huh SJ, Choi DH, Lim YH, Ahn JS, et al. Determining which patients require irradiation of the supraclavicular nodal area after surgery for N1 breast cancer. Int J Radiat Oncol Biol Phys. 2010. 78:1135–1141.

11. Fisher B, Brown A, Mamounas E, Wieand S, Robidoux A, Margolese RG, et al. Effect of preoperative chemotherapy on local-regional disease in women with operable breast cancer: findings from National Surgical Adjuvant Breast and Bowel Project B-18. J Clin Oncol. 1997. 15:2483–2493.

12. Rastogi P, Anderson SJ, Bear HD, Geyer CE, Kahlenberg MS, Robidoux A, et al. Preoperative chemotherapy: updates of National Surgical Adjuvant Breast and Bowel Project Protocols B-18 and B-27. J Clin Oncol. 2008. 26:778–785.

13. van der Hage JA, van de Velde CJ, Julien JP, Tubiana-Hulin M, Vandervelden C, Duchateau L. Preoperative chemotherapy in primary operable breast cancer: results from the European Organization for Research and Treatment of Cancer trial 10902. J Clin Oncol. 2001. 19:4224–4237.

14. Kuerer HM, Newman LA, Smith TL, Ames FC, Hunt KK, Dhingra K, et al. Clinical course of breast cancer patients with complete pathologic primary tumor and axillary lymph node response to doxorubicin-based neoadjuvant chemotherapy. J Clin Oncol. 1999. 17:460–469.

15. Kuerer HM, Sahin AA, Hunt KK, Newman LA, Breslin TM, Ames FC, et al. Incidence and impact of documented eradication of breast cancer axillary lymph node metastases before surgery in patients treated with neoadjuvant chemotherapy. Ann Surg. 1999. 230:72–78.

16. National Comprehensive Cancer Network. NCCN clinical practice guidelines in oncology: breast cancer: v.1.2012. Accessed January 20th, 2012. http://www.nccn.org/professionals/physician_gls/pdf/breast.pdf.
17. Daveau C, Stevens D, Brain E, Berges O, Villette S, Moisson P, et al. Is regional lymph node irradiation necessary in stage II to III breast cancer patients with negative pathologic node status after neoadjuvant chemotherapy? Int J Radiat Oncol Biol Phys. 2010. 78:337–342.

18. American Joint Committee on Cancer. American Cancer Society. American College of Surgeons. AJCC Cancer Staging Manual. 2010. 7th ed. New York: Springer.
19. Kaplan EL, Meier P. Nonparametric estimation from incomplete observations. J Am Stat Assoc. 1958. 53:457–481.

20. McGuire SE, Gonzalez-Angulo AM, Huang EH, Tucker SL, Kau SW, Yu TK, et al. Postmastectomy radiation improves the outcome of patients with locally advanced breast cancer who achieve a pathologic complete response to neoadjuvant chemotherapy. Int J Radiat Oncol Biol Phys. 2007. 68:1004–1009.

21. Le Scodan R, Selz J, Stevens D, Bollet MA, de la Lande B, Daveau C, et al. Radiotherapy for stage II and stage III breast cancer patients with negative lymph nodes after preoperative chemotherapy and mastectomy. Int J Radiat Oncol Biol Phys. 2012. 82:e1–e7.

22. Huang EH, Tucker SL, Strom EA, McNeese MD, Kuerer HM, Buzdar AU, et al. Postmastectomy radiation improves local-regional control and survival for selected patients with locally advanced breast cancer treated with neoadjuvant chemotherapy and mastectomy. J Clin Oncol. 2004. 22:4691–4699.

23. Huang EH, Strom EA, Perkins GH, Oh JL, Chen AM, Meric-Bernstam F, et al. Comparison of risk of local-regional recurrence after mastectomy or breast conservation therapy for patients treated with neoadjuvant chemotherapy and radiation stratified according to a prognostic index score. Int J Radiat Oncol Biol Phys. 2006. 66:352–357.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download