Abstract
Purpose
The purpose of this study is to evaluate the correlation between the conventional plan parameters and dosimetric parameters obtained from conformal radiotherapy (RT) planning, and between these parameters and radiation pneumontitis (RP) incidence.
Methods
Clinical and dosimetric data of 122 patients that were treated with mastectomy and adjuvant 3D conformal RT (39% received 2-field RT [2-FRT], and in addition, 61% received 4-field RT [4-FRT]) were retrospectively analyzed. Central lung depth (CLD), maximum lung depth (MLD), and lung length were measured by the conventional plan. Lung dose-volume histograms (DVH) were created with conformal planning, and the lung volumes receiving 5 to 50 Gy (V5Gy to V50Gy) were calculated. Minimum (Dmin), maximum (Dmax), and mean doses (Dmean) for the ipsilateral lung and bilateral lungs were measured by DVH. Correlations between 3D dosimetric data and 2D radiographic parameters were analyzed.
Results
The conventional plan parameters did not significantly differ between 2-FRT and 4-FRT. The conformal plan Dmin, Dmax, and Dmean values were higher in 4-FRT versus 2-FRT. CLD and MLD were correlated with DVH parameter V5Gy to V45Gy values for ipsilateral, as well as bilateral lungs for 2-FRT. MLD and ipsilateral Dmean via 2-FRT planning had the strongest positive correlation (r=0.76, p<0.01). Moderate correlations existed between CLD and ipsilateral and bilateral lung V5Gy-45Gy, and between MLD and bilateral lung V5Gy-45Gy values in 2-FRT. Only four patients developed symptomatic RP, 4 with 4-FRT and one with 2-FRT.
Conclusion
The conformal plan parameters were strongly correlated with dose-volume parameters for breast 2-FRT. With only 4 cases of Grade 3 RP observed, our study is limited in its ability to provide definitive guidance, however assuming that CLD is an indicator for RP, V20Gy could be used as a predictor for RP and for 2-FRT. A well-defined parameters are still required to predict RP in 4-FRT.
Radiotherapy (RT) is an important component of postoperative treatment in patients with locally advanced breast cancer [1,2]. Although conventional two-dimensional (2D) plans can produce good target coverage with good dose homogeneity, and clinical results from patients treated over the past 50 years with breast/postmastectomy RT, in current clinical practice, three-dimensional (3D) computed tomography (CT) based conformal planning techniques are replacing the 2D conventional planning techniques in breast RT. The main advantages of 3D conformal plans are both improvement in the evaluation of target volume coverage and organs at risk doses, which are vital for predicting the risk of radiation toxicities.
For the conventional plans, certain parameters that have been previously defined have been used to estimate the risk of radiation pneumontitis (RP). Neal and Yarnold [3] defined the central lung distance (CLD) as the distance between the midpoint of the posterior field, and the edge of the chest wall was a predictor of lung doses. It has been reported that CLD is the best predictor of the amount of ipsilateral lung included in the tangential fields [3,4]. The maximum lung depth (MLD) and lung length (LL) have also been used to predict irradiated lung volume [5]. However, these measurements are available only for 2-field tangential irradiation. In cases of additional lymphatic field irradiation, the predictive value of CLD and MLD in estimating the irradiated lung volume is diminished [4,6,7]. Thus, the relationship between the volume of irradiated lung and RP risk warrants further investigation for breast cancer patients treated with RT.
By using CT-based conformal RT plans, it makes it possible to directly measure the lung volume irradiated, with using dose-volume histograms (DVH) that have been generated by a treatment planning system, and help to identify certain parameters that are useful for the prediction of the RP risk. In the conformal RT, the mean V20Gy (the proportion of lung volume receiving ≥20 Gy) of the ipsilateral lung has been shown to positively correlate with RP risk [8]. Lind et al. [9] reported that the delivery of whole-breast RT alone resulted in a V20Gy of approximately 7%, which correlated with a <1% incidence of pneumonitis. However, if additional fields were added to treat regional nodes, the V20Gy increased to ≥20% and the incidence of pneumonitis rose to 7.5% to 11.5%. Additionally, the mean lung dose (MLD) has been used for predicting the RP risk [10,11].
Much of the dosimetric data currently available were derived from lung cancer RT studies, and less data exist, with respect to breast cancer, compared to that of lung cancer RT dosimetry for predicting the RP risk. The aim of this study was to evaluate the DVH data of the irradiated lung with adjuvant breast RT, using 3D-CT-guided planning techniques in patients with chest wall irradiation (2-field RT [2-FRT]), as well as chest wall and lymphatic irradiation (4-field RT [4-FRT]). Additionally, the correlation between DVH and conventional 2D parameters to assess the extent of lung irradiation, as well as the correlation of these parameters with the incidence of symptomatic pneumonitis requiring steroid medication was also investigated in this study.
The clinical and dosimetric data of 122 patients that have been treated with mastectomy and adjuvant RT were retrospectively analyzed. The inclusion criteria were female sex; >18 years-of-age; a histopathological diagnosis of breast cancer after mastectomy and axillary dissection; and having received adjuvant RT, using 3D-CT planning to the chest wall with supraclavicular and axillary irradiation (4-FRT), or without lymphatic RT (2-FRT). Exclusion criteria included unavailability of adequate dosimetric or clinical data; having received unconventional treatment techniques or dose/fractionation; having received previous irradiation; requirement of bilateral breast irradiation; and requirement of internal mammary lymphatic irradiation. These criteria allowed collection of data in a homogenous cohort of patients treated with standard doses and techniques.
The materials in this study were human blood sample from normal individuals and breast cancer patients during with chemotherapy.
Our study contains no private information about patients and has no problems causing any ethical issues or violation of human rights. Informed consent was obtained from all participants and the protocol used in our study was approved by the Institutional Ethics Committee of the Beni-Suef University (Beni-Univ-MSc 171-2010).
Treatment plans were implemented in patients with breast cancer, who had undergone mastectomy. Patients were scanned in the supine position with a Civco C-Qual breast inclined plane on a table-top compatible with the treatment table (Civco indexed carbon fiber MT-IL4101; Civco, Kalona, USA). The entire thorax was scanned with 2.5-mm slice thickness. CT data were then transferred to the treatment planning system (TPS) (Eclipse®, version 8.1; Varian Medical Systems, Palo Alto, USA) with a DICOM network connection.
The irradiation fields encompassed the chest wall, and supraclavicular and axillary lymphatics in 4-FRT, but only the chest wall in 2-FRT (Figure 1). Target volume delineation was performed with the help of atlases and previously-defined target volume contouring protocols [12-14]. The chest wall was contoured, according to contralateral breast tissue margins. Additionally, supraclavicular and level I, II, and III axillary lymphatics were contoured, according to atlases and guidelines. The planning target volume (PTV) for 2-FRT and 4-FRT included the chest wall with the pectoralis muscle, chest wall muscles, and ribs, while excluded the outermost 3 mm from the surface of superficial skin surface. For 4-FRT, level I-III axillary lymphatics and supraclavicular lymph nodes were also included. Both ipsilateral and contralateral lung volumes were contoured, using the TPS density-seeking tool with manual exclusion of the hilum, trachea, pulmonary vessels, and aortic branches.
Patients were treated with a previously-defined RT protocol [15]. Medial and lateral tangential fields were used to treat the entire chest wall. Tangential field borders ensured the coverage of the chest wall with a 1.5-cm margin. The supraclavicular nodes were treated with an anterior field, usually at a 15° gantry rotation to diminish the esophagus and the spinal cord doses. A mono-isocentric technique ensured that the inferior border of the supraclavicular area matched the superior border of the tangential fields, at the inferior aspect of the clavicular head. An anterior supraclavicular field encompassed the supraclavicular and the axillary lymph nodes. In order to increase the doses of axilla, especially to the level II-III lymphatics, a low-weighted posterior field was added.
At each plans, prescribed dose was normalized to target (PTV) the mean receiving 100% of prescribed doses. To achieve homogenous dose distribution, dynamic or hard wedges were used for corresponding fields. In order to increase skin doses, 0.5 to 1 cm bolus materials were used in some cases. All plans were calculated with a pencil beam convolution (PBC) algorithm, with Batho inhomogeneity corrections using the Eclipse® Treatment Planning System (version 8.1). The voxel size in the dose calculation matrix was 0.5×0.5×0.5 cm3.
All patients were treated with the conventional fractionation at 2 Gy fraction doses with a total dose of 50 Gy, using a 6 MV photon energy linear accelerator (Varian DBX 3323; Varian Medical Systems). Patients were treated from Monday to Friday for 5 weeks, and no boosts were allowed. Electronic portal images of each field were obtained before the first treatment and weekly, thereafter, with a therapeutic beam for verification.
Radiation pneumonitis is initially diagnosed with clinical findings, and additionally conventional chest X-ray and high resolution chest CT were required for clinically suspected patients for accurate diagnosis. Patients' medical records were reviewed for RP 6 months after completion of adjuvant breast RT. Clinical data, concerning factors, potentially contributes to the development of pneumonitis, including age, performance status, coexisting pulmonary disease, and smoking habits were recorded. Information concerning chemotherapy and hormonal therapy were also recorded. Toxicity criteria of the Radiation Therapy Oncology Group (RTOG)/the European Organization for Research and Treatment of Cancer (EORTC) was used for assessing respiratory complications [16]. According to this scoring system, symptomatic pneumonitis, which required steroid medication, is accepted as Grade 3 toxicity.
Lung DVHs were created, and data on V5Gy to V50Gy were generated at 5 Gy intervals, where Vx is defined as the percentage of lung volume receiving at least x Gy. Digitally reconstructed images (DRR) were generated to assess the following 2D parameters of lung irradiated: 1) CLD, defined as depth of lung, in centimeters, located within the irradiated field and measured at the central axis [17]; 2) MLD, defined as the maximum depth of lung irradiated [18]; and 3) LL, defined as the length of lung measured at the posterior edge of the tangential field, which extends through the diaphragm for right sided breast irradiation and through the shadow of the heart for the left sided breast irradiation. CLD was measured from the field border to the edge of the lung contour, at the central axis on the tangential simulation radiograph [7]. The 2D parameters were all generated from DRR's and were checked at conventional simulation. Minimum (Dmin), maximum (Dmax), and mean doses (Dmean) delivered to the ipsilateral lung, and bilateral lungs were also determined from the DVH. The 2D parameters, including CLD, MLD, and LL were measured on the conventional radiographs. Correlations between 3D dosimetric data and 2D radiographic parameters were analyzed, using the Pearson correlation test. Statistical analyses were performed using SPSS software version 17.0 (SPSS Inc., Chicago, USA). Additionally, the correlation of these parameters with Grade 3 pulmonary toxicity incidence was also investigated. Correlations were considered significant at p≤0.01. A good correlation between datasets was considered as a Pearson correlation coefficient (r)>0.7; moderate when 0.5<r<0.7; and poor when r<0.5.
A total of 184 mastectomized patients were treated with RT, between January 2008 and November 2009. Of these, 62 patients were excluded: 24 patients were treated with 2D planning, 16 patients underwent internal mammary lymphatic irradiation, 12 patients were treated with electron beams, 5 patients had bilateral breast irradiation, 3 patients left treatment, and 2 patients had incomplete data. Ultimately, 122 patients were included in this study.
Patient characteristics are summarized in Table 1. The mean age of all patients was 50 years, with a range of 32 to 75 years. All patients had good performance status, with a Karnofsky Performance Score of ≥90. Only 8 patients (7%) were smokers, and 12 patients (10%) had pre-existing respiratory illnesses. Chemotherapy, most of which were anthracycline-based regimens, was delivered postoperatively before RT and none of the patients received neoadjuvant chemotherapy. Ninety-three patients (76%) received hormonal therapy, which have begun after RT. Seventy patients (75%) received tamoxifen. The average duration of RT was 5.2 weeks (range, 5.0-6.7 weeks). Forty-eight patients (39%) were treated with 2-FRT and 74 patients (61%) received 4-FRT.
The mean volumes of ipsilateral and bilateral lung volumes were 1,250.9 cc (range, 707.7-2,062.6 cc) and 2,416.0 cc (range, 1,502.2-3,912.8 cc), respectively. The mean Dmin, Dmax, and Dmean for ipsilateral lungs were 0.40±0.18 Gy, 53.02±1.48 Gy, and 11.33±3.64 Gy, respectively. The mean Dmin, Dmax, and Dmean values for both lungs were 0.14±0.08 Gy, 53.09±1.57 2A, B and 6.38±2.05 Gy, respectively.
Conventional planning and dosimetric parameters are summarized in Table 2. Although conventional plan parameters did not differ significantly, between 2-FRT and 4-FRT plans, the conformal plan parameters were significantly higher in 4-FRT plans, compared to that of 2-FRT plans. Similarly, dose volume parameters derived from the conformal plans for the ipsilateral lung and both lungs measured at various dose levels, V5Gy to V50Gy at 5-Gy intervals, were also significantly higher with 4-FRT plans, compared to that of 2-FRT plans (Figure 2A and 2B).
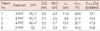
When we analyzed the correlation between CLD and MLD, measured from the conventional plan with DVH V5Gy to V45Gy values for the ipsilateral and bilateral lungs, significant correlation was found for 2-FRT (Figure 3). However this significant correlation was lost in 4-FRT plans. Notably, although a strong correlation between CLD, MLD and Dmean for ipsilateral and both lungs was evident with 2-FRT planning (Table 3), this correlation was diminished with 4-FRT. The correlation between LL and Dmean was significant for ipsilateral lung and nearly significant for both lungs in 2-FRT plans, but there were no significant correlation for 4-FRT plans.
The median follow-up was 26.4 months (range, 6.6-38.5 months) and only four patients (3%) developed Grade 3 RP (Table 4). The clinical findings were verified with chest X-ray and high resolution CT. Three of these female patients were treated with 4-FRT and one was treated with 2-FRT, after a modified radical mastectomy. All patients had no previous history of respiratory illness and were non-smokers. The median time of developing symptomatic RP was 7 months (range, 6-13 months). Dmean and V20Gy for the ipsilateral lung is higher in patients with Grade 3 RP, compared to the mean Dmean and V20Gy values of the entire cohort treated with both 2-FRT and 4-FRT. However CLD was less than the entire cohort mean CLD in one patient and higher in 2 patients treated with 4-FRT, and higher than the mean CLD in one patient treated with 2-FRT. In patients treated with 2-FRT, MLD was higher than that of the entire cohort MLD. However, MLD was equal to the mean MLD in one patient and higher than the mean MLD in 2 patients treated with 4-FRT.
Radiation pneumonitis is an early inflammatory reaction that can occur after RT in treating cancers of the lung, esophagus, and breast [19]. RP usually occurs within 1 to 6 months after completion of RT [20], but onset occasionally occurs, as late as 14 months after radiation [21]. The clinical findings are non-specific respiratory symptoms, such as sub-febrile fever, non-productive cough, or mild dyspnea, which usually resolve after high-dose corticosteroids. The development of RP depends on the treatment-related factors [22,23], such as radiation dose, fractionation schedule, volume and region of lung irradiated, use of concurrent chemotherapy, and patient-related factors [6,9], such as pre-existing lung disease, poor pulmonary function, being a smoker, and genetic predisposition. It has been previously reported that radiation-induced lung sequelae affect as many as 9% of patients with breast cancer being treated with RT [24]. However, using computer-based radiation treatment planning systems dramatically decreased the incidence of these lung sequelae [25,26].
The region irradiated with adjuvant breast RT was thin and peripherally located in tangential fields, and the apex region was irradiated in the supraclavicular field, whereas, the irradiated region in lung cancer RT tends to be more central. Therefore, the lung DVH criteria used to estimate RP risk in lung cancer RT may not be directly applicable to breast cancer patients. Although a CLD of <3 cm is widely accepted for breast cancer RT, this CLD has its limitations, particularly when the treatment technique is more complex. The correlation was evident using the 2-FRT technique, but this correlation diminished when additional fields were added. CLD and MLD are measured from tangential fields. In cases of additional lymphatic field irradiation, the lung doses increased, significantly, despite equivalent MLD and CLD values, as demonstrated in this current study. With 4-FRT, the apical portion of the lungs is at high risk for pneumonitis, and mostly fibrosis or consolidation was evident at the apex of the axilla. However, few patients ultimately develop symptomatic RP. CLD and MLD are, therefore, not adequate parameters that are indicative of lung doses and RP risk for 4-FRT and conformal dose-volume parameters are found to be more accurate in these cases. A correlation between CLD and dose-volume analysis of the ipsilateral lung has been previously established. Das et al. [4] demonstrated a linear relationship between a regression slope of 0.5% to 0.6% ipsilateral lung volume, irradiated per millimeter of lung depth, and a CLD of 0.5 to 3.5 cm. Kong et al. [6] and Teh et al. [5] identified strong correlations between CLD and lung volume irradiated at various dose levels in patients with early-stage breast cancer, who received RT using a 3D-CT technique to the breast or the chest wall. In this current study, we demonstrated a good correlation of MLD and CLD from conventional planning with lung doses obtained from conformal RT planning, only in patients with mastectomy treated with 2-FRT technique. However, this strong correlation was lost when extra fields were added (Table 3).
CLD has been accepted as a reference measure of lung volume irradiated for the prediction RP risk, as a result of conventional breast RT [3,4,27]. Guidelines published by the EORTC and the European Society of Mastology (EUSOMA) state that the CLD should be <3 cm to limit the incidence of RP in adjuvant breast RT [27]. Lingos et al. [28] reported that a CLD <3 cm resulted in no cases of pneumonitis, among 1,624 patients treated for breast cancer. For 2-FRT planning, achieving a CLD <3 cm is difficult in patients with larger PTV because larger fields are needed to encompass the PTV. Because 3D-CT planning tools are becoming increasingly available, the direct use of lung DVH may be a better tool to evaluate RP risk. Lind et al. [8] found a correlation between the risk of RP and the mean ipsilateral V20Gy values in patients with breast cancer treated with various RT techniques. The incidence of pneumonitis was <1% with V20Gy values of 7% using 2-field tangential technique. However, adding more fields to treat regional nodes resulted in a V20Gy increase of 20% to 30%, and the incidence of pneumonitis significantly increased to 7.5% to 11.5%. Similarly, Teh et al. [5] reported a 1.1% incidence of radiation pneumonitis with the mean ipsilateral V20Gy values of 14% with 2-field RT. When the supraclavicular field was added, the mean V20Gy as a proportion of the ipsilateral lung increased to 22%. Chie et al. [7] reported that the incidence of RP significantly increased from 2.4% to 12.1% (p=0.02), when local and regional RT was performed compared to that of local RT. The authors demonstrated a significant correlation between the percent of lung volume and CLD. In this current study, the V20Gy value for the ipsilateral lung was 15.6% with 2-FRT, and increased to 26.5% with 4-FRT. These values were similar to that of the previous studies, which supports the low incidence of RP in patients treated with 2-FRT. So, V20Gy can be recommended as a good indicator for predicting RP risk, especially for 2-FRT plans.
This study does have limitations. The retrospective nature of this study is the largest limitation. In contrast to retrospective studies, a prospective study would better evaluate RP, and should be more accurate in the prediction of RP risk. Although we analyzed patients retrospectively, we only evaluated one group of patients in order to overcome patient selection bias. For example, only patients who underwent radical mastectomy and were treated with RT within a set period of time were included in this study. Lastly, although CLD recommendation have been widely used to predict RP, several reports failed to show the significant correlation between CLD and RP [9,29]. However, as conventional parameters have limitations in their predictive power, 3D parameters have replaced their roles in current practice, such as Quantitative Analyses of Normal Tissue Effects in the Clinic (QUANTEC) [30]. In this study assuming that CLD is a predictor for RP, the conformal dosimetric parameters could be used for the prediction of RP risk.
Guidelines for limiting the incidence of RP in adjuvant breast RT are traditionally based on a 2D parameter, such as a CLD of <3 cm. However, this parameter is only applicable for tangential breast or chest wall irradiation. Previous studies have reported a correlation between CLD and the volume of lung irradiated, but a direct correlation between CLD and RP incidence has not been clearly demonstrated. In this study, we identified a strong correlation between the conformal plan parameters and the dose volume parameters for 2-field tangential breast RT. Additionally, although the V20Gy values were within previously defined limits, and symptomatic pneumonitis requiring steroid medication was a rare complication with computer-based treatment planning, dosimetric data for lungs, such as V20 could be an important parameter for predicting RP for 2-FRT, however further studies are required for analyzing the risk for RP in 4-FRT plans.
Figures and Tables
 | Figure 1Dose distribution in patients included in this study. The lung and target doses are demonstrated on (A) coronal and (B) sagittal sections with 2-field radiotherapy. The lung doses increased as a result of additional lymphatic fields, as demonstrated on (C) coronal and (D) sagittal sections with 4-field radiotherapy.
LL=lung length; CLD=central lung depth; MLD=maximum lung depth.
|
 | Figure 2(A) Dose volume analyses of ipsilateral lungs obtained from 2-field and 4-field treatment planning. The values from 2-field and 4-field planning are significantly different (p<0.05). (B) Dose volume analyses of both lungs obtained from 2-field and 4-field treatment planning. The values from 2-field and 4-field planning are significantly different (p<0.05). |
 | Figure 3(A) Correlation between maximum lung diameter and mean lung doses at treated chest wall for 2-field planning. (B) Correlation between maximum lung diameter and the percentage of ipsilateral lung volume that received at least 20 Gy (V20Gy) with 2-field planning. |
Table 2
Mean±SD values of lung conventional and conformal plan parameters data for 2-field and 4-field radiotherapy techniques
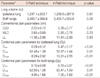
Table 3
Pearson correlation factors between conventional and conformal plan parameters for ipsilateral and both lungs in 2-field and 4-field techniques

References
1. Recht A. Integration of systemic therapy and radiation therapy for patients with early-stage breast cancer treated with conservative surgery. Clin Breast Cancer. 2003. 4:104–113.

2. Olivotto IA, Chua B, Elliott EA, Parda DS, Pierce LJ, Shepherd L, et al. A clinical trial of breast radiation therapy versus breast plus regional radiation therapy in early-stage breast cancer: the MA20 trial. Clin Breast Cancer. 2003. 4:361–363.

3. Neal AJ, Yarnold JR. Estimating the volume of lung irradiated during tangential breast irradiation using the central lung distance. Br J Radiol. 1995. 68:1004–1008.

4. Das IJ, Cheng EC, Freedman G, Fowble B. Lung and heart dose volume analyses with CT simulator in radiation treatment of breast cancer. Int J Radiat Oncol Biol Phys. 1998. 42:11–19.

5. Teh AY, Park EJ, Shen L, Chung HT. Three-dimensional volumetric analysis of irradiated lung with adjuvant breast irradiation. Int J Radiat Oncol Biol Phys. 2009. 75:1309–1315.

6. Kong FM, Klein EE, Bradley JD, Mansur DB, Taylor ME, Perez CA, et al. The impact of central lung distance, maximal heart distance, and radiation technique on the volumetric dose of the lung and heart for intact breast radiation. Int J Radiat Oncol Biol Phys. 2002. 54:963–971.

7. Chie EK, Shin KH, Kim DY, Kim TH, Kang HS, Lee ES, et al. Radiation pneumonitis after adjuvant radiotherapy for breast cancer: a volumetric analysis using CT simulator. J Breast Cancer. 2009. 12:73–78.

8. Lind PA, Wennberg B, Gagliardi G, Fornander T. Pulmonary complications following different radiotherapy techniques for breast cancer, and the association to irradiated lung volume and dose. Breast Cancer Res Treat. 2001. 68:199–210.

9. Lind PA, Marks LB, Hardenbergh PH, Clough R, Fan M, Hollis D, et al. Technical factors associated with radiation pneumonitis after local +/- regional radiation therapy for breast cancer. Int J Radiat Oncol Biol Phys. 2002. 52:137–143.

10. Hernando ML, Marks LB, Bentel GC, Zhou SM, Hollis D, Das SK, et al. Radiation-induced pulmonary toxicity: a dose-volume histogram analysis in 201 patients with lung cancer. Int J Radiat Oncol Biol Phys. 2001. 51:650–659.

11. Yorke ED, Jackson A, Rosenzweig KE, Merrick SA, Gabrys D, Venkatraman ES, et al. Dose-volume factors contributing to the incidence of radiation pneumonitis in non-small-cell lung cancer patients treated with three-dimensional conformal radiation therapy. Int J Radiat Oncol Biol Phys. 2002. 54:329–339.

12. Martinez-Monge R, Fernandes PS, Gupta N, Gahbauer R. Cross-sectional nodal atlas: a tool for the definition of clinical target volumes in three-dimensional radiation therapy planning. Radiology. 1999. 211:815–828.

13. Li XA, Tai A, Arthur DW, Buchholz TA, Macdonald S, Marks LB, et al. Variability of target and normal structure delineation for breast cancer radiotherapy: an RTOG Multi-Institutional and Multiobserver Study. Int J Radiat Oncol Biol Phys. 2009. 73:944–951.

14. Castro Pena P, Kirova YM, Campana F, Dendale R, Bollet MA, Fournier-Bidoz N, et al. Anatomical, clinical and radiological delineation of target volumes in breast cancer radiotherapy planning: individual variability, questions and answers. Br J Radiol. 2009. 82:595–599.

15. Atahan IL, Ozyigit G, Yildiz F, Gurkaynak M, Selek U, Sari S, et al. Percent positive axillary involvement predicts for the development of brain metastasis in high-risk patients with nonmetastatic breast cancer receiving post-mastectomy radiotherapy. Breast J. 2008. 14:245–249.

16. Cox JD, Stetz J, Pajak TF. Toxicity criteria of the Radiation Therapy Oncology Group (RTOG) and the European Organization for Research and Treatment of Cancer (EORTC). Int J Radiat Oncol Biol Phys. 1995. 31:1341–1346.

17. Maguire PD, Marks LB, Sibley GS, Herndon JE 2nd, Clough RW, Light KL, et al. 73.6 Gy and beyond: hyperfractionated, accelerated radiotherapy for non-small-cell lung cancer. J Clin Oncol. 2001. 19:705–711.

18. Chung HT, Xia P, Chan LW, Park-Somers E, Roach M 3rd. Does image-guided radiotherapy improve toxicity profile in whole pelvic-treated high-risk prostate cancer? Comparison between IG-IMRT and IMRT. Int J Radiat Oncol Biol Phys. 2009. 73:53–60.

19. Tsoutsou PG, Koukourakis MI. Radiation pneumonitis and fibrosis: mechanisms underlying its pathogenesis and implications for future research. Int J Radiat Oncol Biol Phys. 2006. 66:1281–1293.

20. Kim TH, Cho KH, Pyo HR, Lee JS, Zo JI, Lee DH, et al. Dose-volumetric parameters for predicting severe radiation pneumonitis after three-dimensional conformal radiation therapy for lung cancer. Radiology. 2005. 235:208–215.

21. Wang S, Liao Z, Wei X, Liu HH, Tucker SL, Hu CS, et al. Analysis of clinical and dosimetric factors associated with treatment-related pneumonitis (TRP) in patients with non-small-cell lung cancer (NSCLC) treated with concurrent chemotherapy and three-dimensional conformal radiotherapy (3D-CRT). Int J Radiat Oncol Biol Phys. 2006. 66:1399–1407.

22. Seppenwoolde Y, De Jaeger K, Boersma LJ, Belderbos JS, Lebesque JV. Regional differences in lung radiosensitivity after radiotherapy for non-small-cell lung cancer. Int J Radiat Oncol Biol Phys. 2004. 60:748–758.

23. Tsujino K, Hirota S, Endo M, Obayashi K, Kotani Y, Satouchi M, et al. Predictive value of dose-volume histogram parameters for predicting radiation pneumonitis after concurrent chemoradiation for lung cancer. Int J Radiat Oncol Biol Phys. 2003. 55:110–115.

24. Hurkmans CW, Borger JH, Bos LJ, van der Horst A, Pieters BR, Lebesque JV, et al. Cardiac and lung complication probabilities after breast cancer irradiation. Radiother Oncol. 2000. 55:145–151.

25. Kahan Z, Csenki M, Varga Z, Szil E, Cserháti A, Balogh A, et al. The risk of early and late lung sequelae after conformal radiotherapy in breast cancer patients. Int J Radiat Oncol Biol Phys. 2007. 68:673–681.

26. Varga Z, Cserháti A, Kelemen G, Boda K, Thurzó L, Kahán Z. Role of systemic therapy in the development of lung sequelae after conformal radiotherapy in breast cancer patients. Int J Radiat Oncol Biol Phys. 2011. 80:1109–1116.

27. Bartelink H, Garavaglia G, Johansson KA, Mijnheer BJ, Van den Bogaert W, van Tienhoven G, et al. Quality assurance in conservative treatment of early breast cancer. Report on a consensus meeting of the EORTC Radiotherapy and Breast Cancer Cooperative Groups and the EUSOMA (European Society of Mastology). Radiother Oncol. 1991. 22:323–326.
28. Lingos TI, Recht A, Vicini F, Abner A, Silver B, Harris JR. Radiation pneumonitis in breast cancer patients treated with conservative surgery and radiation therapy. Int J Radiat Oncol Biol Phys. 1991. 21:355–360.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download