Abstract
Purpose
The available research work on types of treatment and the efficacy of adjuvant chemotherapy in older Korean patients is insufficient. Henceforth, this report assessed treatment patterns and the relationship between chemotherapy and survival in elderly Korean breast cancer patients.
Methods
We identified women over 55 years of age diagnosed with breast cancer from the period 1995 to 2006. Clinicopathologic features and treatment methods were compared for three groups divided on the basis of age: 55 to 59 years, 60 to 69 years, and over 70 years old. The effects of chemotherapy on survival were compared overall and individually for each group.
Results
A total of 832 patients over 55 years of age were included in the present investigation. No statistical differences were observed between the three age groups in clinicopathologic features including tumor size, grade, and stage. However, patients in the elderly group received mastectomy more often when compared to the younger groups (p<0.001). In contrast, there was a decline in radiation treatment and chemotherapy with older age (p<0.001). Overall, patients who received chemotherapy had a significantly increased breast cancer specific survival and overall survival rate when compared to the non-chemotherapy groups (p=0.022). Among the estrogen receptor positive group, no statistical significance was achieved in the survival benefit of chemotherapy. However, in estrogen receptor-negative patients, overall, the chemotherapy groups showed a better survival rate than the non-chemotherapy patients and a similar trend was observed in each age group except in the group comprising of 70 years old patients.
Conclusion
This study describes the survival benefit of adjuvant chemotherapy in Korean patients over 55 years of age, especially in hormone receptor-negative patients. Hence, based on the results of the present report and considering the similarity of clinicopathologic features between age groups, it is proposed that age alone should not be a determinant factor of treatment methods.
Breast cancer survival and disease-free periods have experienced improvement with advancements in diagnostic methods and treatment modalities. However, breast carcinoma is the most common malignancy in women in Western countries [1]. In Korean women, breast cancer is the second most common types of cancer and the leading cause of death [2,3]. One of the considerable reasons for this increased incidence would be an aging population and changes in lifestyle [4,5]. Worldwide, more than one-half of breast cancers cases occur in women over the age of 60 years [6]. Definition of "older people" or "elderly" is somewhat arbitrary. Although some developed countries have accepted the chronological age of 65 years as "elderly," United Nations and World Health Organization have agreed cutoff of 60 years to refer to the older population [7]. Older women represent the fastest growing segment of the population in Asia, with a resultant increase in the number of diagnosed cases of breast carcinoma in older women [2,8].
Although the number of older women with breast cancer is increasing, treatment guidelines for this segment of the population are less definitive than for younger patients. Moreover, breast cancer treatment in older women is influenced by a number of misconceptions [9], and considerable controversies exists about cancer aggressiveness and treatment policies [10]. Along with having multiple comorbid conditions, less social support, poor performance status and lower life expectancy, older patients are more likely to receive substandard care for breast cancer [11,12]. In addition, older women are less commonly included in clinical trials, and this lack of data might result in less aggressive treatment. Consequently, chemotherapy guidelines for older breast cancer patients are less definite than guidelines for younger patients, even when randomized clinical trials have demonstrated the efficacy of adjuvant chemotherapy [13,14]. Although several studies have demonstrated that providing older women with chemotherapy has beneficial effects on survival [13,15], older women are less likely to receive adjuvant chemotherapy regardless of the stage of breast cancer [16,17].
According to statistical projections, Korea is entering quickly into the category of aging society and experiencing low fertility rate, so an increased rate of breast cancer is expected, especially in older age groups [18,19]. Compared to Western patient populations, Korean patient populations have many parallels as well as known differences in host disease and epidemiological characteristics. However, only a few studies have been conducted on older breast carcinoma patients, including on treatment methods, with accompanying outcomes. For this reason, in the present report, we assessed the characteristics, treatment and follow-up results for Korean women older than 55 years. In particular, we compared the relationship between adjuvant chemotherapy and survival.
We evaluated 1,054 breast cancer patients aged 55 years and older, who were referred for surgery at the Samsung Medical Center between August 1995 and November 2006. Patients satisfying the study criteria were women 1) without preoperative distant metastasis and neoadjuvant chemotherapy; and 2) with equal to or higher than T1 breast cancer stage according to the seventh edition of tumor, node, metastasis system (TNM) by the American Joint Committee on Cancer (AJCC) [20]. We identified 832 cases appropriate for inclusion and assessed clinicopathologic features and follow-up results using our hospital's electronic database. Patients were divided into three comparison groups based on age: 55 to 59 years, 60 to 69 years, and ≥70 years.
Data were extracted on the following variables: patient's age, tumor grade, resection margin, lymphovascular invasion, TNM system, hormone receptor status, HER2/neu status and details of treatment with surgery, chemotherapy, radiation and hormonal therapy. Receipt of chemotherapy was defined as receipt within 6 months after diagnosis. Disease-specific survival (DSS) and overall survival (OS) were measured as the time from breast cancer diagnosis until death as a result of a breast cancer-related cause (e.g., cancer-specific mortality, CSM) and as a result of an all-cause, respectively, or until date of last follow-up.
The tumor specimens were evaluated for estrogen and progesterone receptor status by standard immunohistochemistry, and tumors were considered receptor-positive if more than 5% of cells showed nuclear staining or if they scored equal to or higher than 3+ on the Allred scoring system. HER2 status was determined on tumor tissues using anti-HER2 polyclonal antibody and tissues were considered receptor positive if the staining intensity was 3+. Scores of zero or 1+ were negative and scores of 2+ were further evaluated with fluorescence in situ hybridization.
Descriptive analyses were performed to explore clinicopathologic characteristics and treatment methods based on the subgroup. Pearson's χ2 test or the Kruskal-Wallis test was used to compare the use of adjuvant chemotherapy and each covariate based on the age group. We used the Kaplan-Meier method and the log-rank test to estimate DSS between the three groups. For multivariate analysis, Cox-Hazard regression method was performed.
Data were analyzed using Microsoft Excel 2007 (Microsoft, Redmond, USA). Statistical analyses were performed using PASW Statistics 18.0 (SPSS Inc., Chicago, USA). Reported p-values are two-sided and statistical significance was set at p<0.05.
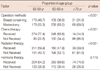
This retrospective cohort study included 832 patients. The median age of the patients at the time of diagnosis was 61 years (range, 55-84 years) and the median follow-up period was 68 months (range, 1-179 months). The mean tumor size was 23.3 mm (range, 1.0-145.0 mm). Out of the 854 patients, 354 (42.5%) were between 55 and 59 years of age, 378 (45.4%) were between 60 and 69 years of age, and 100 (12.0%) were either 70 years or older. Patient's characteristics by age group are given in Table 1.
Tumor size distribution was not significantly different among each age groups (p=0.938). Tumor histology, grade and stage were similar in the all age groups (p=0.357, p=0.421, and p=0.932). The proportion of women with hormone receptor expression increased with age. For example, 55.8% of patients aged ≥70 years showed positive expression of the progesterone receptor when compared with 40.8% of patients aged between 55 and 59 years (p=0.027). For estrogen receptor expression, a larger percent of patients with age ≥70 years had a high degree of expression (age 55-59 years, 60.1%; age 60-69 years, 66.8%; age over 70 years, 69.5%), but it was not significant (p=0.094).
Table 2 shows treatment methods according to age group. Patients in the elderly group received mastectomy more often than younger patients (age over 70 years, 69.0%; age 60-69 years, 63.2%; age 55-59 years, 50.3%; p<0.001). As expected, the use of radiation treatment declined with increase in age (p<0.001). The proportion of patients, who were treated with chemotherapy, was also decreased in elderly group (p<0.001). Although more patients in elderly group were treated with hormone therapy (age over 70 years, 74.0%; age 60-69 years, 69.6%; age 55-59 years, 64.2%), this differences were not statistically significant (p=0.110).
After a median follow-up of 68 months, there were occurrence of 98 cases of breast cancer-related death and 108 cases of all cause death. The 5-year cumulative CSM incidence was 8.5±1.1% (standard error, 0.5%). For patients aged between 55 and 59 years, the 5-year cumulative CSM incidence was 7.0±1.5% when compared with incidence of 7.5±1.5% for 60 to 69 years group, and 18.8±4.7% for the patients aged 70 years and above (Figure 1). Clinicopathologic characteristics according to use of chemotherapy are described in Table 3. Chemotherapy group had aggressive prognostic factors including poorer tumor grade and high T, N stage. To exclude potential confounders, databases were adjusted for tumor size, histology, tumor grade, nodal status, presence of lymphovascular invasion, expression of estrogen receptor and use of hormone therapy. Figure 2 shows the adjusted DSS and OS in total patients and age-related subgroups. In the overall age group, patients who received chemotherapy had a significantly increased DSS rate (p=0.022) than the non-chemotherapy group. For all subgroups, the patients with chemotherapy had a tendency to have a better DSS rate; however this was not significant (age 55-59 years, p=0.420; age 60-69 years, p=0.140; age over 70 years, p=0.554). Similar with DSS, overall age group (p=0.006) and 60 to 69 years group (p=0.025) showed significant survival benefit of chemotherapy, however, no statistical significance was observed in both 55 to 59 years group and over 70 years group (p=0.256 and p=1.000, respectively).
We subdivided each age group based on hormone receptor expression. Among the estrogen receptor-positive group (n=511), the chemotherapy group (n=292) showed better DSS than the non-chemotherapy group (n=219) in the overall population and in the 60 to 69 age group; however this was not significant for the overall population and each age group (overall, p=0.311; age 50-59 years, p=0.221; age 60-69 years, p=0.094; age over 70 years, p=1.000) (Figure 3). Figure 4 shows adjusted DSS and OS rates in estrogen receptor-negative groups. In the overall population (n=285), use of chemotherapy (n=232) was found to be significantly associated with a better DSS rate than non-chemotherapy treatment (n=53, p=0.004). Moreover, the 55 to 59 years group and the 60 to 69 years group showed DSS benefits with chemotherapy (p=0.005 and p=0.018). Although there was no statistical significance in the over 70 years group due to the small sample size (p=0.277), recipients of chemotherapy in this group also showed a better DSS rate. Adjusted OS rate in estrogen receptor negative group were found to be similar with DSS rate. There were significant survival benefit of chemotherapy in overall age group (p=0.011) and 55 to 59 years group (p=0.016). In 60 to 69 years group, patients who were treated with chemotherapy showed a tendency of an increase in OS (p=0.062).
Aging is a major risk factor for the development of new breast cancer [5]. Unlike in Western countries, diagnosis of breast cancer in Korean women peaks in the 45- to 49-year age group. Although the breast cancer incidence has doubled in the last decades, peak age has remained same [21]. However, in Korea, the number of people aged 60 years and above has increased, and the Korean population is expected to enter an aged society in the near future [18]. Consequently, there will be more incidences and cases of cancer in older Korean women. Until now, few studies have reported treatment and consequent survival in older women, especially in Korean population. Therefore, in the present report, we describe treatment patterns and the efficacy of adjuvant chemotherapy in Korean elderly people. This study compared characteristics and treatment between three age groups (55-59 years, 60-69 years, and ≥70 years old) and analyzed adjuvant chemotherapy and survival rate in Korean women with breast cancer.
Korean patients have different ethnic features and life style when compared with American patients. Beside peak age of the disease, Korean women have more dense breast than American women [22]. High breast density has been suggested as a risk factor of breast cancer [23]. Other differences in Korean women such as early age at menarche, late age at menopause and late age at first full term pregnancy leads to changes in the breast tissue susceptibility to hormonal stimulus and increases the risk of cancer development and progression [24]. Not only racial difference, but aging is another distinctive feature in breast cancer aggressiveness and treatment. Aging itself is a major risk factor for the development and prognosis of breast cancer [5,25]. In general, breast cancer-specific survival in elderly patients is poorer when compared to younger patients. The reason for poorer survival is complicated and may be related with advanced stage at diagnosis, lower rates of screening, less aggressive treatment due to multiple or severe comorbidities and poorer general health status [25]. Considering the distinctive characters of Korean elderly people, we have described clinicopathologic characteristics, treatment patterns and the efficacy of adjuvant chemotherapy in Korean elderly people.
We observed no statistical differences in histology, tumor grade and stage, even in elderly patients. Infiltrating ductal carcinoma was the most common histologic type in all groups. Although differences were not significant, mucinous carcinoma was noted about 7% in the over 70 years group. Mucinous carcinoma represents only 1% of breast cancers in premenopausal women, however, this type of breast cancers is seen more frequently in postmenopausal women (4% to 6%) [10]. In this study, cancer in the older patients more commonly expressed hormone receptors, as has also been reported in other reports [5,26].
In general, older women are less likely to undergo breast-conserving surgery, radiation therapy, and adjuvant systemic therapy [11,12]. Our results showed similar results with respect to patterns of treatment. As has been previously described, no significant differences in cancer stage were observed between the three age groups, however, older patients received less aggressive management than younger patients. The reason for this different treatment pattern may be multifactorial. The first possible explanation is the presence of multiple comorbid conditions. In our hospital, surgeons and oncologists determined treatment methods on case-by-case basis. Along with the high incidence of comorbidities, patient preference, degree of independence and patient access to hospitals were included in our treatment decisions. General function and socioeconomic status of patients might also be a reason for the observed differences in treatment pattern.
In this study, we compared the DSS rate for patients, who did and did not receive adjuvant chemotherapy. Chemotherapy improved the survival of postmenopausal patients. The results of our survival analysis were similar to previously published reports on patients in Western countries [15,27]. Our results describe a benefit for adjuvant chemotherapy in improving breast cancer-specific survival in Korean women. Moreover, in all age groups, hormone receptor-negative patients had survival benefits from chemotherapy. The survival benefit of chemotherapy in hormone receptor-negative patients implies two meaningful values. First, these patients had no adjuvant systemic treatment besides chemotherapy because hormonal treatment is not effective for hormone receptor negative cancers [15,28]. Second, because of the ineffectiveness of hormone therapy, many clinicians do not recommend hormonal treatment for these patients. Therefore, hormone treatment did not confound the relationship between chemotherapy and survival.
This study has three limitations resulting from the retrospective and uncontrolled study design. The two groups divided on the basis of chemotherapy were different from each other with respect to clinical characteristics and disease aggressiveness. Because the chemotherapy groups had higher tumor grades and advanced cancer stages, we adjusted for these different clinical characteristics with multivariate analysis (e.g., Cox-Hazard regression method) for an unbiased statistical interpretation. Another limitation is that we could not fully evaluate the comorbidities of the breast cancer patients and the decision making process of use of chemotherapy because of retrospective study design and insufficient hospital electronic records. Generally, clinicians tend to recommend a less aggressive treatment including adjuvant chemotherapy for patients with multiple or severe comorbidities. These limitations might result in bias for patient selection and for analysis of the survival benefit from chemotherapy. For avoiding these confounding factors, we compared not only OS rate but also breast cancer-specific mortality as an endpoint. Our patients experienced 98 cases of cancer-specific mortalities and 108 cases of all cause mortalities. After adjusting clinical factors using multivariate analysis, DSS and OS showed similar results that chemotherapy attributed to increased survival in overall patients and hormone receptor negative patients. Finally, the oldest age group (≥70 years old) had a small sample size. As has been previously described, receipt of chemotherapy in patients over 70 years of age with estrogen receptor-negative cancer had better survival rates; however, this result was not significant because of the small number of patients in this group. We could not provide the statistical significant benefit of adjuvant chemotherapy in over 70 years group, although 70 years is the commonly used cutoff age amongst the oncologists [29].
This study describes the benefits of adjuvant chemotherapy in Korean women with hormone receptor-negative breast cancer. Our study found similar clinicopathologic features between age groups, hence age alone should not be considered as a determinant of treatment methods. Despite limitations including retrospective study design and insufficient information on the general health status of patients, this study suggests important implications for the establishment of breast cancer treatment guidelines and future prospective trials for elderly Korean patients. We hope that future studies will be focused on the survival benefits of chemotherapy with large prospective studies for older Korean women.
Figures and Tables
 | Figure 1Cumulative incidence of breast cancer-specific mortality. (A) Total population. (B) Subgroup by age. |
 | Figure 2Survival results by chemotherapy. (A) Disease-specific survival of total patients. (B) Disease-specific survival of 55 to 59 years group. (C) Disease-specific survival of 60 to 69 years group. (D) Disease-specific survival of ≥70 years group. (E) Overall survival of total patients. (F) Overall survival of 55 to 59 years group. (G) Overall survival of 60 to 69 years group. (H) Overall survival of ≥70 years group.
CTx+=chemotherapy received group; CTx-=chemotherapy non-received group.
|
 | Figure 3Survival results by chemotherapy in estrogen receptor-positive patients. (A) Disease-specific survival of total patients. (B) Disease-specific survival of 55 to 59 years group. (C) Disease-specific survival of 60 to 69 years group. (D) Disease-specific survival of ≥70 years group. (E) Overall survival of total patients. (F) Overall survival of 55 to 59 years group. (G) Overall survival of 60 to 69 years group. (H) Overall survival of ≥70 years group.
CTx+=chemotherapy received group; CTx-=chemotherapy non-received group.
|
 | Figure 4Survival results by chemotherapy in estrogen receptor-negative patients. (A) Disease-specific survival of total patients. (B) Disease-specific survival of 55 to 59 years group. (C) Disease-specific survival of 60 to 69 years group. (D) Disease-specific survival of ≥70 years group. (E) Overall survival of total patients. (F) Overall survival of 55 to 59 years group. (G) Overall survival of 60 to 69 years group. (H) Overall survival of ≥70 years group.
CTx+=chemotherapy received group; CTx-=chemotherapy non-received group.
|
References
1. Siegel R, Ward E, Brawley O, Jemal A. Cancer statistics, 2011: the impact of eliminating socioeconomic and racial disparities on premature cancer deaths. CA Cancer J Clin. 2011. 61:212–236.
2. Yoo KY, Kang D, Park SK, Kim SU, Shin A, Yoon H, et al. Epidemiology of breast cancer in Korea: occurrence, high-risk groups, and prevention. J Korean Med Sci. 2002. 17:1–6.

3. Jung KW, Park S, Kong HJ, Won YJ, Lee JY, Park EC, et al. Cancer statistics in Korea: incidence, mortality, survival, and prevalence in 2008. Cancer Res Treat. 2011. 43:1–11.

4. Leonard R, Ballinger R, Cameron D, Ellis P, Fallowfield L, Gosney M, et al. Adjuvant chemotherapy in older women (ACTION) study: what did we learn from the pilot phase? Br J Cancer. 2011. 105:1260–1266.

5. Gennari R, Curigliano G, Rotmensz N, Robertson C, Colleoni M, Zurrida S, et al. Breast carcinoma in elderly women: features of disease presentation, choice of local and systemic treatments compared with younger postmenopasual patients. Cancer. 2004. 101:1302–1310.
6. Jemal A, Bray F, Center MM, Ferlay J, Ward E, Forman D. Global cancer statistics. CA Cancer J Clin. 2011. 61:69–90.

7. Health of the elderly. Report of a WHO Expert Committee. World Health Organ Tech Rep Ser. 1989. 779:1–98.
8. Yoo KY, Kim Y, Park SK, Kang D. Lifestyle, genetic susceptibility and future trends of breast cancer in Korea. Asian Pac J Cancer Prev. 2006. 7:679–682.
9. Singh R, Hellman S, Heimann R. The natural history of breast carcinoma in the elderly: implications for screening and treatment. Cancer. 2004. 100:1807–1813.

10. Diab SG, Elledge RM, Clark GM. Tumor characteristics and clinical outcome of elderly women with breast cancer. J Natl Cancer Inst. 2000. 92:550–556.

11. Bernardi D, Errante D, Gallligioni E, Crivellari D, Bianco A, Salvagno L, et al. Treatment of breast cancer in older women. Acta Oncol. 2008. 47:187–198.

12. Giordano SH, Hortobagyi GN, Kau SW, Theriault RL, Bondy ML. Breast cancer treatment guidelines in older women. J Clin Oncol. 2005. 23:783–791.

13. Elkin EB, Hurria A, Mitra N, Schrag D, Panageas KS. Adjuvant chemotherapy and survival in older women with hormone receptor-negative breast cancer: assessing outcome in a population-based, observational cohort. J Clin Oncol. 2006. 24:2757–2764.

14. Muss HB. Factors used to select adjuvant therapy of breast cancer in the United States: an overview of age, race, and socioeconomic status. J Natl Cancer Inst Monogr. 2001. 52–55.

15. Early Breast Cancer Trialists' Collaborative Group (EBCTCG). Effects of chemotherapy and hormonal therapy for early breast cancer on recurrence and 15-year survival: an overview of the randomised trials. Lancet. 2005. 365:1687–1717.
16. Woodard S, Nadella PC, Kotur L, Wilson J, Burak WE, Shapiro CL. Older women with breast carcinoma are less likely to receive adjuvant chemotherapy: evidence of possible age bias? Cancer. 2003. 98:1141–1149.

17. Du X, Goodwin JS. Increase of chemotherapy use in older women with breast carcinoma from 1991 to 1996. Cancer. 2001. 92:730–737.

18. Choi Y, Kim YJ, Shin HR, Noh DY, Yoo KY. Long-term prediction of female breast cancer mortality in Korea. Asian Pac J Cancer Prev. 2005. 6:16–21.
19. Park SK, Kim Y, Kang D, Jung EJ, Yoo KY. Risk factors and control strategies for the rapidly rising rate of breast cancer in Korea. J Breast Cancer. 2011. 14:79–87.

20. Edge SB, Compton CC. The American Joint Committee on Cancer: the 7th edition of the AJCC cancer staging manual and the future of TNM. Ann Surg Oncol. 2010. 17:1471–1474.

21. Lee JH, Yim SH, Won YJ, Jung KW, Son BH, Lee HD, et al. Population-based breast cancer statistics in Korea during 1993-2002: incidence, mortality, and survival. J Korean Med Sci. 2007. 22:Suppl. S11–S16.

22. Kim SH, Kim MH, Oh KK. Analysis and comparison of breast density according to age on mammogram between Korean and Western women. J Korean Radiol Soc. 2000. 42:1009–1014.

23. McCormack VA, dos Santos Silva I. Breast density and parenchymal patterns as markers of breast cancer risk: a meta-analysis. Cancer Epidemiol Biomarkers Prev. 2006. 15:1159–1169.

24. Suh JS, Yoo KY, Kwon OJ, Yun IJ, Han SH, Noh DY, et al. Menstrual and reproductive factors related to the risk of breast cancer in Korea. Ovarian hormone effect on breast cancer. J Korean Med Sci. 1996. 11:501–508.

25. Herbsman H, Feldman J, Seldera J, Gardner B, Alfonso AE. Survival following breast cancer surgery in the elderly. Cancer. 1981. 47:2358–2363.

26. Pierga JY, Girre V, Laurence V, Asselain B, Diéras V, Jouve M, et al. Characteristics and outcome of 1755 operable breast cancers in women over 70 years of age. Breast. 2004. 13:369–375.

27. Giordano SH, Duan Z, Kuo YF, Hortobagyi GN, Goodwin JS. Use and outcomes of adjuvant chemotherapy in older women with breast cancer. J Clin Oncol. 2006. 24:2750–2756.





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download