Abstract
Purpose
This study aimed to analyze the efficacy and prognostic significance of adjuvant tamoxifen in breast cancer patients with various hormone receptor statuses.
Methods
Typically, 1,260 female breast cancer patients were recruited in this study. The correlation between estrogen receptor (ER)/progesterone receptor (PR) phenotypes and clinical characteristics was investigated, and the survival rate was assessed after 5-year follow-up.
Results
The 5-year overall survival (85%) was better in women under the age of 50 years. Patients with ER+/PR+ tumors had a better 5-year survival rate (94%); those with ER-/PR- tumors experienced the worst outcome (74% survival rate); whereas single-positive cases were in between. In 97 out of 128 patients with ER-/PR+ tumors, tamoxifen was given as adjuvant hormonal therapy, and it increased the survival benefit in the lower grade group in terms of overall survival and disease-free survival (p=0.01 and p=0.03, respectively).
Adjuvant endocrine therapy is usually offered after surgery and radiotherapy for breast cancers. It is effective only among patients with hormone receptor-expressed tumors, such as estrogen receptor (ER)-positive and/or progesterone receptor (PR)-positive [1,2]. It can reduce the risk of deaths due to breast cancer and recurrence in those patients, who have been widely confirmed for breast cancer through many clinical trials [2-4]. It has been reported that after a long-term follow-up, more than 34% of significant reduction in the relative risk for recurrence and death was observed in patients with adjuvant hormonal therapy [2]. Thus, the ER and PR status of breast tumors are now routinely determined, so that physician can suggest an appropriate endocrine therapy for the patient.
In general, it has been reported that more than 67% of breast cancers are sensitive to tamoxifen therapy [5-8]. Typically, ER as a predictor of endocrine therapy efficacy is well accepted. Nevertheless, the role of PR in predicting the efficacy of endocrine therapy is still controversial. However, some reports have shown the limit value of PR as a therapeutic predictor [9], others highlighted the use of PR status as a predictive factor for benefit from adjuvant endocrine therapy, also demonstrating its significance in prognostic outcomes [10].
The first aim of this study was to identify the efficacy of adjuvant tamoxifen in patients with ER-/PR+ breast tumors. The second aim was to stratify the survival curve as well as risk factors of breast cancer, according to the hormone receptor status in Taiwanese women.
The studies were approved by the Institutional Review Board and Ethics Committee of the Changhua Christian Hospital. (Approval number 090902). Specifically, patients, diagnosed between 2002 and 2006, were identified from the Changhua Christian Hospital cancer registry databases. Due to incomplete information pertaining to hormone receptor status before 2002, analysis was initiated from 2002.
Using the registry software, well-trained case managers collected uniform information about all the patients with breast cancer, who have been examined at least once as outpatients or inpatients in the daily clinical service. The baseline data included demographic characteristics, tumor characteristics and ER/PR status. The Nottingham modification of the Scarff-Bloom-Richardson grading scheme was applied in the histologic grading of invasive breast cancer. Basically, this grading scheme is based on three morphologic features: degree of tumor tubule formation, tumor mitotic activity and nuclear pleomorphism of tumor cells. The sum of these scores stratifies breast tumors into Grade I (score 3-5, well differentiated), Grade II (score 6-7, moderately differentiated) and Grade III (score 8-9, poorly differentiated) malignancies. In this study, the AJCC staging system [11] was used, and a variety of edit checks and procedures were employed to omit duplicate records. The quality of the cancer registry database was reviewed and approved by a committee, which consisted of radiologists, oncologists, pathologists, surgeons, and an epidemiologist with special expertise in breast cancer.
For detection of the patients' ER and PR statuses, IHC analyses were performed on the formalin-fixed, paraffin-embedded breast cancer tissues, with anti-ER (clone SP1, dilution 1:200; Lab Vision, Fremont, USA) and anti-PR antibodies (clone SP2, dilution 1:250; Lab Vision) by an autostaining system (Ventana Medical Systems Inc., Tucson, USA). A report of 10% or greater of cells that had nuclear staining for ER was considered a positive result as well as PR.
The determination of HER2 gene amplification was also performed with IHC method (Dako, Carpinteria, USA). Assessment of staining was based on a semi quantitative score (range, 0 to 3+). Absence of or weak incomplete membrane staining (0 to 1+) was considered a negative result; 2+ staining with complete membrane was considered as equivocal overexpression; and 3+ staining was considered overexpression.
Data are expressed as the mean±standard deviation (SD) for continuous variables. ANOVA analysis was used for the comparison of continuous variables, and categorical variables were normally tested by the χ2 test when appropriate. In addition, for small numbers counted in categorical variables (e.g., grade and staging) a Fisher's exact test was performed. All p-values are two-tailed; a p-value of less than 0.05 was considered to indicate statistical significance. Cumulative survival rates of breast cancer cases were analyzed by the Kaplan-Meier method, and differences in cumulative survival were assessed using the Log-rank method. The SAS 9.1.3 (SAS Institute Inc., Cary, USA) for windows software package was used for analysis.
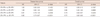
Typically, 1,260 female patients were included in this analysis with an average age of 51.5±12.0 years. A total of 92 deaths from breast cancer were ascertained after follow-up until 31, December 2007. Of these cases, ER+/PR+, ER+/PR-, ER-/PR+, and ER-/PR- were 680 (54%), 139 (11%), 128 (10%), and 313 cases (25%), respectively. In the subgroup analysis of ER-/PR+ tumors, tamoxifen was given as adjuvant hormonal therapy in 97 out of 128 cases. As shown in Table 1, tumor characteristics among women with breast cancer according to ER and PR status was analyzed. There was no significant difference among the 5 groups with regard to age, tumor size, lymph node status, distant metastasis and stage. Besides, the distributions of hormone receptor status among the series in this study compared to other studies were shown in Table 2. The ER+ phenotype was around 24% to 82%, and the ER-/PR+ status accounted for 3% to 11%. Furthermore, 15% to 66% were double-negative tumors.
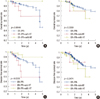
The mean 5-year overall survival was 85%; 5-year overall survival was higher in women <50 years as compared to women >50 years (p<0.0496) (Figure 1A). In Figure 1B, higher 5-year survival rate was detected in double-positive tumors (94%), and double-negative tumors were associated with a 5-year overall survival of 74%, which was statistically different from the double-positive tumors (p<0.0001).
Disease-free survival was also significantly different between the four groups (Figure 1C). Patients with double-positive tumors had the highest disease-free survival while the ER-/PR+ and double-negative groups had the lowest.
The relationship between total breast cancer deaths and ER and PR status were also analyzed (Table 3). In the ER-/PR- group, the mortality rate was high (15%) whereas the mortality rate in the ER+/PR+ group was low as 3%.
Table 3 shows the breast cancer death among women with breast cancer by ER and PR expression, there were 5 cases of breast cancer death in the group without tamoxifen (4 out of 5 were older than 50 years) and 8 in the group that received tamoxifen (4 cases were older than 50 years); the overall survival rate was not significant between these two groups.
In the univariate Cox regression analysis of factors associated with overall survival and disease-free survival, the significant differences were found in overall survival between the ER-positive groups (ER+/PR-, hazard ratio of 0.78; ER+/PR+, hazard ratio of 0.70) versus the double-negative (Table 4). Furthermore, differences in disease-free survival were detected between the double-positive versus the double-negative groups (hazard ratio of 0.80). In the multivariate Cox regression analysis, the significant differences were found in disease-free survival and overall survival between ER+/PR+ versus the double-negative. There was no survival significant difference between ER-/PR+ and double-negative tumors (Table 5). Although it is a well known evidence that double-positive versus double-negative patients had survival benefit after adjuvant hormonal therapy [2], the benefit between ER-/PR+ and double-negative patients were still controversial in our study.
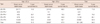
The patients were further stratified based on histological grade: low-grade (I and II) and high-grade (III). No survival benefit was detected with adjuvant tamoxifen therapy in the high-grade group. However, adjuvant tamoxifen treatment significantly improved survival in low-grade patients (Figure 2A and B). Significant differences between the double-negative and ER-/PR+ groups with or without tamoxifen were detected (Figure 2C and D). In low-grade tumors, patients with ER-/PR+ tumors who did not receive tamoxifen treatment had the worst outcome whereas the ER-/PR+ group who received the hormonal therapy had the best outcome in terms of overall survival and disease-free survival (p=0.0144 and p=0.0328, respectively).
Determination of ER and PR expression by IHC analysis is routinely used for the identification of patients, who are most likely to benefit from endocrine therapy. Currently, ER/PR status is probably the best predictive marker. Tamoxifen has been widely accepted as an adjuvant endocrine therapy after surgery, leading to improved disease-free and overall survival and reduced recurrence rate. As shown in Table 2, the data demonstrates that ER+ tumors accounted for about 65% of all tumors, whereas approximately 25% were double-negative tumors. Therefore, in Taiwan, the ER+ rate was lower than that reported in Western countries [6-8]. However, single-positive and double-negative tumors accounted for 21% and 25% of the tumors, respectively, which is consistent with data from other countries [5,6,8,12].
Who benefits from adjuvant endocrine therapy? Although the older endocrine therapies included surgical ablative procedures and high dose hormones in the early 1970s, current guidelines call for the determination of ER and PR status in all primary invasive breast cancers. Adjuvant endocrine therapy should be considered only in ER- or PR-positive patients [13]. In the 2000s, the gold standard for adjuvant endocrine therapy was tamoxifen, and the duration of treatment was 5 years. After 5 years of adjuvant tamoxifen treatment, the reduction in annual rate of recurrence and mortality was 41% and 34%, respectively [2]. Furthermore, the reduction in contralateral breast cancer was 39%, and the 15-year absolute reduction in recurrence and mortality was 12% and 9.2%, respectively, which were significantly different from patients not receiving tamoxifen [2].
ER-positive status included both ER+/PR+ and ER+/PR- phenotypes. Osborne et al. [14] demonstrated that double-positive tumors had higher response rate when compared with ER+/PR- tumors. Loprinzi et al. [15] also showed that PR level was responsive to the treatment benefit; the higher the ER expression, the more likely PR was to be positive.
In the present study, identification of breast cancer biomarkers was of great significance, and determination of the response to hormonal therapy was a key point to survival. Rakha et al. [6] reported a large series of primary invasive breast cancer with long-term follow-up. The clinical outcome showed that double-positive breast cancer had the best outcome followed by single-positive tumors; the double-negative phenotype had the worst outcome, which was consistent with the results from this study.
In Taiwan, a predominance of breast cancers was ER+, and adjuvant endocrine therapy was indicated in these cases. This study also demonstrates that adjuvant endocrine therapy was statistically more effective in ER+ tumors when compared with double-negative tumors in overall and disease-free survival.
There have been many controversies in breast cancer management. Novel drugs (i.e., aromatase inhibitors) were available for the treatment of hormone receptor-positive breast cancer patients. Recent adjuvant endocrine therapy trials included initial, initial and sequential, sequential, switching, and extended adjuvant therapies [4,16-20]. However, there were certain questions like, which treatment should be started first? What is the duration of treatment; how long the treatment should be continued? Thus, new strategies were needed for the treatment of hormone receptor-positive breast cancer.
In this study, 25% of breast cancers were ER-/PR-, and therefore, adjuvant hormone therapy was not indicated. This group experienced the worst disease-free survival and overall survival, which was consistent with previous studies [5,6,8,13]. PR- breast cancer may have impaired ER signaling, rendering them less responsive to tamoxifen treatment. Therefore, chemotherapy should be given in a more aggressive manner to these patients.
In previous studies, the frequency of ER-/PR+ phenotype has been reported to be 4% to 10% [5-8,10,12,21]. In this phenotype, some ER-/PR+ tumors in the elderly might be due to lower expression of ER level. However, Yu et al. [22] revealed that Chinese breast cancer patients with ER-/PR+ tumors were mainly premenopausal and younger in age. They received less benefit from adjuvant tamoxifen therapy. In this study, the frequency of ER-/PR+ tumors was about 10%, and there were no significant differences in age, tumor size, lymph node status, distant metastasis, and stage among the tumors (Table 1).
This study demonstrated an association with better outcome for the ER+/PR- phenotype when compared with the double-negative group. There was no significant difference between the ER-/PR+ and double-negative groups in overall and disease-free survival. In the previous study by Rakha et al. [6], patients with single-positive tumors (ER+/PR- and ER-/PR+) had prognostic and predictive differences in overall survival and disease-free interval when compared with patients who had double-positive tumors. Unfortunately, their study had only six patients treated with adjuvant tamoxifen after surgery in the ER-/PR+ group. The small number of cases in the group may lead to the false significant correlation and may not reflect the real response to hormonal therapy.
Still, the role of PR in endocrine treatment is unclear. In clinical practice, the effect of hormone therapy has been a matter of controversy for patients who had ER-/PR+ tumors [23,24]. In fact, the benefit of endocrine therapy was seldom discussed in the previous studies and to the best of our knowledge, this is for the first time that the treatment effect on PR status in Taiwanese women with breast cancer has been demonstrated. In the ER-/PR+ group, 97 cases were treated with tamoxifen and 31 cases were left untreated with tamoxifen. Tamoxifen demonstrated little benefit in this group when compared with the double-negative tumors, and the result was consistent with a previously reported study [6]. However, upon further stratification by histological grade, no survival difference was detected in high-grade patients treated with tamoxifen when compared with double-negative tumors in terms of overall survival and disease-free survival (p=0.5359 and p=0.3474). However, a survival benefit was observed within the low grade patients treated with tamoxifen (p=0.0144). Thus, the histological grade may be an important predictive factor for response to tamoxifen treatment in the sub-group of ER-/PR+ patients.
Chemotherapy was administered to the patients according to the breast cancer treatment guideline in our hospital. Adjuvant chemotherapy was given if the patient fulfilled the criteria. The addition of tamoxifen to chemotherapy certainly produced some additional benefits [3]. Our data showed that in subgroup of ER-/PR+, and in low grade cancers with or without tamoxifen treatment, the percentages of chemotherapy administered were 69% and 52%, respectively. Adjuvant chemotherapy might have imparted survival benefit to this group of patients, which is consistent with a previous study [3]. However, in high-grade subgroup with or without tamoxifen treatment, chemotherapy was administered in 78% and 33% of cases, respectively. High-grade tumor with ER-/PR+, adjuvant tamoxifen therapy may have no survival benefit even with high percentage of chemotherapy. Rakha et al. [25] reported that histological grade was an important independent prognostic factor when compared to lymph node status, tumor size, and vascular invasion in invasive breast carcinoma. Furthermore, some studies suggest that HER2/neu-positive patients may be less sensitive to endocrine therapies [26], and HER2/neu amplification is a marker of relative endocrine resistance [27,28]. In Taiwan, the use of trastuzumab (Herceptin) in an adjuvant setting was not covered by the national insurance due to the medical policy of Taiwan. In our study, a high percentage (48%) of patients was HER2/neu-positive in the ER-/PR+ group. Therefore, the benefit of trastuzumab and resistance of endocrine therapy through HER2/neu status was not assessed in this study.
There were several limitations in this study, such as the small number of patients (total 128 cases). Data from the Early Breast Cancer Trialist Collaborative Group (EBCTCG) meta-analyses demonstrated that the benefits of tamoxifen on survival only start to appear close to 5 years, and increase over the next 10 years [27,28]. However, we found significant difference in survival after 2 years follow-up. Although we believe that tamoxifen was effective in some ER-/PR+ patients with relative dependence on histological grade, randomized clinical trials are needed to understand the real treatment effect of hormonal therapy on ER-/PR+ tumors.
Differences in histological grade and outcome between hormonal receptor statuses were also detected. Patients with ER+/PR+ tumors had better clinical outcomes; patients with ER-/PR- tumors experienced the worst outcome; whereas single-positive cases were in between. Most of the oncologists would recommend adjuvant hormone therapy for any patient, whose tumor shows receptor positivity, as either ER and/or PR. However, according to our study, in cases of high-grade tumor with ER-/PR+, adjuvant tamoxifen therapy may have no survival benefit whereas for the patients with low-grade ER-/PR+ tumors, adjuvant tamoxifen therapy is highly suggestive.
Figures and Tables
 | Figure 1The 5-year survival rate. (A) Overall survival was determined by age. Overall survival (B) and disease-free survival (C) according to estrogen receptor (ER) and progesterone receptor (PR) status. |
 | Figure 2Effects of estrogen receptor (ER) and progesterone receptor (PR) status on overall survival in patients with low-grade (A) or high-grade (B) breast tumors. Disease-free survival in patients with low-grade (C) or high-grade (D) breast tumors according to ER and PR status. HT=hormone therapy. |
Table 1
Descriptive statistic for tumor characters among women with breast cancer according to ER/PR status

ACKNOWLEDGEMENTS
We would like to thank the Cancer Registry of Changhua Christian Hospital for providing the data used in this study and the Center of Biostatistic Consultation, National Taiwan University College of Public Health, for assistance with statistical analysis. Editorial support was provided by Ms. Yu-Fen Wang, M.S.
References
1. Fisher B, Anderson S, Tan-Chiu E, Wolmark N, Wickerham DL, Fisher ER, et al. Tamoxifen and chemotherapy for axillary node-negative, estrogen receptor-negative breast cancer: findings from National Surgical Adjuvant Breast and Bowel Project B-23. J Clin Oncol. 2001. 19:931–942.

2. Early Breast Cancer Trialists' Collaborative Group (EBCTCG). Effects of chemotherapy and hormonal therapy for early breast cancer on recurrence and 15-year survival: an overview of the randomised trials. Lancet. 2005. 365:1687–1717.
3. Early Breast Cancer Trialists' Collaborative Group. Tamoxifen for early breast cancer: an overview of the randomised trials. Lancet. 1998. 351:1451–1467.
4. Howell A, Cuzick J, Baum M, Buzdar A, Dowsett M, Forbes JF, et al. Results of the ATAC (Arimidex, Tamoxifen, Alone or in Combination) trial after completion of 5 years' adjuvant treatment for breast cancer. Lancet. 2005. 365:60–62.

5. Osborne CK, Schiff R, Arpino G, Lee AS, Hilsenbeck VG. Endocrine responsiveness: understanding how progesterone receptor can be used to select endocrine therapy. Breast. 2005. 14:458–465.

6. Rakha EA, El-Sayed ME, Green AR, Paish EC, Powe DG, Gee J, et al. Biologic and clinical characteristics of breast cancer with single hormone receptor positive phenotype. J Clin Oncol. 2007. 25:4772–4778.

7. Anderson WF, Chen BE, Jatoi I, Rosenberg PS. Effects of estrogen receptor expression and histopathology on annual hazard rates of death from breast cancer. Breast Cancer Res Treat. 2006. 100:121–126.

8. Arpino G, Weiss H, Lee AV, Schiff R, De Placido S, Osborne CK, et al. Estrogen receptor-positive, progesterone receptor-negative breast cancer: association with growth factor receptor expression and tamoxifen resistance. J Natl Cancer Inst. 2005. 97:1254–1261.

9. Olivotto IA, Truong PT, Speers CH, Bernstein V, Allan SJ, Kelly SJ, et al. Time to stop progesterone receptor testing in breast cancer management. J Clin Oncol. 2004. 22:1769–1770.

10. Bardou VJ, Arpino G, Elledge RM, Osborne CK, Clark GM. Progesterone receptor status significantly improves outcome prediction over estrogen receptor status alone for adjuvant endocrine therapy in two large breast cancer databases. J Clin Oncol. 2003. 21:1973–1979.

11. Greene FL. American Joint Committee on Cancer, American Cancer Society. AJCC Cancer Staging Manual. 2002. 6th ed. Philadelphia: Springer.
12. Carey LA, Perou CM, Livasy CA, Dressler LG, Cowan D, Conway K, et al. Race, breast cancer subtypes, and survival in the Carolina Breast Cancer Study. JAMA. 2006. 295:2492–2502.

13. National Comprehensive Cancer Network. Clinical practice guidelines in oncology: breast cancer- v.1. 2012. Accessed March 8th, 2012. http://www.nccn.org/professionals/physician_gls/f_guidelines.asp.
14. Osborne CK, Yochmowitz MG, Knight WA 3rd, McGuire WL. The value of estrogen and progesterone receptors in the treatment of breast cancer. Cancer. 1980. 46:12 Suppl. 2884–2888.

15. Loprinzi CL, Ravdin PM, de Laurentiis M, Novotny P. Do American oncologists know how to use prognostic variables for patients with newly diagnosed primary breast cancer? J Clin Oncol. 1994. 12:1422–1426.

16. Breast International Group (BIG) 1-98 Collaborative Group. Thürlimann B, Keshaviah A, Coates AS, Mouridsen H, Mauriac L, et al. A comparison of letrozole and tamoxifen in postmenopausal women with early breast cancer. N Engl J Med. 2005. 353:2747–2757.

17. Jakesz R, Jonat W, Gnant M, Mittlboeck M, Greil R, Tausch C, et al. Switching of postmenopausal women with endocrine-responsive early breast cancer to anastrozole after 2 years' adjuvant tamoxifen: combined results of ABCSG trial 8 and ARNO 95 trial. Lancet. 2005. 366:455–462.

18. Coombes RC, Hall E, Gibson LJ, Paridaens R, Jassem J, Delozier T, et al. A randomized trial of exemestane after two to three years of tamoxifen therapy in postmenopausal women with primary breast cancer. N Engl J Med. 2004. 350:1081–1092.

19. Kaufmann M, Jonat W, Hilfrich J, Eidtmann H, Gademann G, Zuna I, et al. Improved overall survival in postmenopausal women with early breast cancer after anastrozole initiated after treatment with tamoxifen compared with continued tamoxifen: the ARNO 95 Study. J Clin Oncol. 2007. 25:2664–2670.

20. Goss PE, Ingle JN, Martino S, Robert NJ, Muss HB, Piccart MJ, et al. Randomized trial of letrozole following tamoxifen as extended adjuvant therapy in receptor-positive breast cancer: updated findings from NCIC CTG MA.17. J Natl Cancer Inst. 2005. 97:1262–1271.

21. Bird PA, Hill AG, Houssami N. Poor hormone receptor expression in East African breast cancer: evidence of a biologically different disease? Ann Surg Oncol. 2008. 15:1983–1988.

22. Yu KD, Di GH, Wu J, Lu JS, Shen KW, Liu GY, et al. Breast cancer patients with estrogen receptor-negative/progesterone receptor-positive tumors: being younger and getting less benefit from adjuvant tamoxifen treatment. J Cancer Res Clin Oncol. 2008. 134:1347–1354.

23. Nikolic-Vukosavljevic D, Kanjer K, Neskovic-Konstantinovic Z, Vukotic D. Natural history of estrogen receptor-negative, progesterone receptor-positive breast cancer. Int J Biol Markers. 2002. 17:196–200.

24. Mc Cormack O, Harrison M, Kerin MJ, McCann A. Role of the progesterone receptor (PR) and the PR isoforms in breast cancer. Crit Rev Oncog. 2007. 13:283–301.

25. Rakha EA, El-Sayed ME, Lee AH, Elston CW, Grainge MJ, Hodi Z, et al. Prognostic significance of Nottingham histologic grade in invasive breast carcinoma. J Clin Oncol. 2008. 26:3153–3158.

26. Piccart MJ, Di Leo A, Hamilton A. HER2: a 'predictive factor' ready to use in the daily management of breast cancer patients? Eur J Cancer. 2000. 36:1755–1761.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download