Abstract
Purpose
Percutaneous removal of benign breast tumors using ultrasound-guided vacuum-assisted breast biopsy (VABB) has been recently regarded as a feasible and safe method without serious complications. The aim of this study was to evaluate the efficacy and safety of the VABB in the treatment of benign phyllodes tumors, and to identify whether or not surgical re-excision is necessary for benign phyllodes tumors diagnosed and excised by VABB.
Methods
From January 2003 to December 2011, a total of 6,923 VABB were performed in 5,434 patients. Out of 6,923 lesions, 53 were benign phyllodes tumors. Among these, 31 lesions, with a follow-up period of longer than 24 months, were enrolled in this study. Ultrasonography follow-up was performed at 3 to 6 month intervals in order to assess recurrence. The mean follow-up period was 75.9±13.5 months (range, 24-94 months).
Results
The mean patient age at presentation was 31.6±9.4 years. The mean size of the lesion was 1.60±0.88 cm. The majority of lesions, 74.2% (23 cases), were palpable, and 25.8% (8 cases) were non-palpable. Twenty-two lesions (71.0%) were classified as Breast Imaging Reporting and Data System category 3, and nine lesions (29.0%) were classified as category 4a, by ultrasonography. During the follow-up period, local recurrence developed in one lesion, making the local recurrence rate 3.2%.
In Western societies, one woman in eight develops breast cancer during her lifetime; it has been reported that approximately 60% of women have benign breast diseases [1]. While fibroadenoma and fibrocystic diseases are among the most common benign breast diseases, phyllodes tumors are rare fibroepithelial lesions that account for approximately 1% of breast tumors [2]. A phyllodes tumor has stromal hypercellularity, which is different from fibroadenoma, and tends to grow like a leaf as interstitium intensively grows in ducts. This type of tumor was named 'cystosarcoma phyllodes' by Müller in 1838 [3] and renamed 'phyllodes tumor' by World Health Organization (WHO), in 1982, because 70% of patients have a benign course, and little cystic change is observed [4]. A phyllodes tumor is clinically similar to fibroadenoma, but shows characteristic findings, including rather high occurrence at a younger age; non-calcareous, well-defined, round or oval lobular nodules on mammography or ultrasonography; and heterogeneous interior with cystic components. Generally, phyllodes tumors are classified as benign, borderline, or malignant, according to the mitotic rate upon high-power microscopic examination. Wide local excision, including the minimum 1 cm of surrounding normal tissue, has been recommended as the treatment of choice [5], and it has been reported that local recurrence rate is as high as 8% to 40% and distant metastasis rate 1% to 21% [6,7]. Prognostic evaluation, depending only on histological findings can be questionable because metastasis may be reported even with histologically benign lesions, and lesions may not recur or metastasize despite malignancy [8].
With the development of vacuum-assisted breast biopsy (VABB) (Mammotome®; Devicore Medical, Cincinnati, USA), benign breast tumors can be excised, including surrounding normal tissue in a minimally invasive way; complete excision, without residual tissues is possible in most cases [9,10]. In this study, follow-up without reoperation was carried out at intervals of 3 to 6 months on patients who were definitely diagnosed with benign phyllodes tumor, with VABB for benign tumors, and who were judged to have been completely excised without residual tissue on ultrasonography.
From January 2003 to December 2011, a total of 6,923 VABBs were performed on 5,434 patients at the Department of Surgery of Kangnam CHA Hospital, Seoul, Korea. Out of 6,923 lesions, 53 were benign phyllodes tumors. Among these, 31 lesions of 28 patients with a follow-up period longer than 24 months were included in this study. The mean follow-up period was 75.9±13.5 months (range, 24-94 months). The follow-up was carried out with ultrasonography and mammography, at intervals of 3 to 6 months, in order to identify recurrences. In all cases, preoperative core-needle gun biopsy was not performed prior to VABB. VABB was performed mostly in patients who were expected to have a difficult follow-up for lesions 3 cm or smaller according to the Breast Imaging Reporting and Data System (BI-RADS) [11] category 3 or 4a on ultrasonography, who planned to be pregnant, who felt extremely uneasy from their lesions, whose lesions enlarged during follow-up, and who complained of pains or symptoms. Additionally, this was performed in some patients who refused to undergo excision, though their lesions were larger than 3 cm, because they were concerned about breast scars. In cases of BI-RADS category 5, VABB was not performed. All lesions were taken out by eight-gauge needles. Local anesthesia, using a mixture of 1% lidocaine and epinephrine was administered; skin was incised 3 to 5 mm. The needle was rotated at an angle of 45 degrees, to both sides, during the procedure, in order to completely excise the hypoechic lesion on intraoperative ultrasonography and until normal fat tissue was verified grossly on core pieces. For hemostasis, direct compression was applied for 5 to 10 minutes immediately following the procedure; an elastic bandage was attached, and the patient took bed rest for 6 hours. This study is approved by Institutional Review Board (IRB) (IRB No. KNC 12-022).
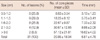
VABB procedures from January 2003 to December 2011, at the author's hospital, revealed that benign phyllodes tumors accounted for 0.77% (53/6,923) of the lesions. Benign phyllodes tumor patients with follow-up periods longer than 24 months were enrolled; most of these individuals were in their twenties or thirties (82.1%); 14 in their twenties (50.0%), 9 in their thirties (32.1%), 3 in their forties (10.7%), and 2 aged fifty or older (7.2%). The mean age was 31.6±9.4 years (Table 1). The tumors were classified into five groups, according to size; 0.6-1.0 cm, 1.1-1.5 cm, 1.6-2.0 cm, 2.1-3.0 cm, and 3.1 cm or greater. Each of the groups included: 8 cases (25.8%), 9 cases (29.0%), 8 cases (25.8%), 4 cases (12.9%) and 2 cases (6.5%), respectively. Mean core pieces acquired from each group were 3.13±1.23, 5.75±3.41, 7.33±2.32, 8.66±2.08, 16.62±4.02, respectively. The mean size was 1.60±0.88 cm, mean core pieces acquisition was 20.85±18.94, and mean procedure time was 6.61±4.78 minutes (Table 2). Upon physical examination, palpable and non-palpable lesions were observed in 23 (74.2%) and 8 cases (25.8%), respectively, and lesions were found slightly more on the right breast than the left (16 vs. 15). Nineteen (61.4%) and 10 cases (36.7%) were observed in the upper outer and the upper inner quadrants, respectively. One case (3.2%) each was noted in the lower outer and the lower inner quadrants, respectively. There were 3 patients presenting with two foci of benign phyllodes lesions, 2 patients exhibited this on the same side of breast and the other patient experienced it bilaterally. On preoperative ultrasonography, BI-RADS category 3 and 4a were observed in 22 (71.0%) and 9 cases (29.0%), respectively. On mammography, category 0 was observed in 12 cases (38.7%), and category 1 in 8 (25.8%) (Table 1). In all cases, there were no complications other than minor ecchymosis after the VABB procedure.
A phyllodes tumor recurred in 1 case, during the follow-up period; the patient was 33 years old at presentation, and the size of the mass was 1.3 cm according to the ultrasonography taken before the VABB procedure. The lesion was a well-defined oval benign tumor of BI-RADS category 3, and was palpable at the lower outer quadrant of the right breast (Figure 1). A residual lesion was not observed upon follow-up ultrasonography, taken 3 months after the VABB procedure, but after 11 months a nodule was palpable, and a local recurrence of BI-RADS category 4a was found on ultrasonography. The recurring lesion was 1.5 cm, undefined, and segment-like. Wide local excision and pathologic examination were performed, and the lesion was confirmed to be a benign phyllodes tumor; resection margins were all negative (Figure 2). Local recurrence or distant metastasis was not observed in other cases.
The causes of phyllodes tumors are not clearly understood, nor is their relationship to fibroadenoma. In many cases, fibroadenoma occurs concurrently or successively with a phyllodes tumor. The question of whether a phyllodes tumor originates from fibroadenoma or is caused by to a completely different process would benefit from further study [12]. Noguchi et al. [13] stated that fibroadenoma should be regarded as a hyperplasic lesion rather than a neoplasm because it contained polyclonal components in most cases; additionally, somatic mutation-based monoclonal proliferation, shown in some fibroadenoma, might progress to develop the recurrent tendency and phyllodes tumors.
Microscopic findings of phyllodes tumors are different from those of fibroadenoma. Fibroadenoma shows low stromal cellularity, true capsule, and no evidence of mitoses or pleomorphism in most cases. Phyllodes tumors are classified into benign, borderline, or malignant, based on the conditions of interface, stromal cellularity, mitotic rate, and pleomorphism. In this study, the criterion for benign phyllodes tumors, according to the number of mitoses on a high-power microscope, was 0 to 1; 2 to 5 for borderline, and 6 or more for malignant. The frequency of malignancy has been variously reported, 2% to 45% [14,15]. Heterogeneity of tumors, errors in collecting specimens, and different criteria for interpreting histological results are potential reasons for the variation. Until now, 61 phyllodes tumors were diagnosed by VABB, in our hospital, including 5 borderline, 3 malignant, and 53 benign cases. Additional wide local excision was performed for borderline and malignant tumors.
Surgical excision is not required for all fibroadenoma [16] because the natural history of fibroadenoma rarely shows development to cancer, and the tumor size decreases over time, in some cases. However, histological examinations should be performed in case the tumor grows rapidly, even if the nodule appears to be benign, because it may be a phyllodes tumor rather than fibroadenoma. Surgical treatment, according to the literature, should be performed if histological examinations concluded that it is a phyllodes tumor. For borderline or malignant tumors diagnosed on preoperative core-needle gun biopsies, wide local excision should be performed, including surrounding normal tissue of 1 cm or greater. However, a watch-and-wait policy is reported to be safe in case the excised tissue is histologically diagnosed as a benign phyllodes tumor [17]. Reinfuss et al. [18] observed in this manner, and reported that benign phyllodes tumors locally recurred in 4% of patients and that the 5-year survival rate was 96%. It has been debated whether or not additional surgical treatment is required, or whether follow-up should be performed, for cases diagnosed with benign phyllodes tumor with a positive resection margin.
The local recurrence rate of phyllodes tumors has been reported to range from 10% to 40%, with a mean value of approximately 15% [14,15]. Local recurrence is primarily related to the range of the first operation and is considered to arise from the failure of the first operation [15,19-21]. Usually, local recurrence occurs within several years of the operation, and its histological characteristics are similar to those of the primary tumor [15]. A recurrent lesion is often more aggressive histologically than the primary tumor [22], and it has been reported that most local recurrence is not related to distant metastasis and that distant metastasis occurs without local recurrence [23]. It was reported that survival rate was not remarkably different, even in occasional cases when a phyllodes tumor continuously recurred over a long period of time, and that local recurrence was unrelated to histological characteristics or the conditions of interface [24].
The prognostic factors related to local recurrence have been widely studied. Age has been regarded a relatively unimportant factor, but some researchers reported that phyllodes tumors during adolescence were less aggressive [25,26]. The effect of size of the primary tumor is unclear. Most reports show that local recurrence rate is low in the tumors of 2 cm or smaller [15,27], but reports professing the contrary exist as well [18]. A small tumor is likely to have a negative resection margin by local excision of sufficient range, and eventually incomplete excision may be associated with local recurrence. Additionally, it is not clear whether local recurrence occurs more frequently in malignant phyllodes tumors. Most distant metastases occur with borderline or malignant phyllodes tumors, and they occur differently from local recurrence; the size of primary tumor is a major prognostic factor for distant metastasis. Stromal overgrowth, mass necrosis, infiltrative interface, high mitotic index, and stromal atypical cells have also been reported as histological characteristics related to distant metastasis [20,21].
VABB, which has in the recent years been commonly used for breast benign tumors, is a minimally invasive procedure that can remove lesions under ultrasonography guidance, without re-aim or re-insertion. Initially, VABB was used for biopsy; later, with advancements in the understanding of the technique, it was used in attempts to excise lesions suspected to be benign tumors. Its application has been extended to most benign breast diseases, including fibroadenoma, intraductal papilloma, fibrocystic change, and complicated cysts; and we reported that complete recovery could be reached through complete excision by VABB, for benign tumors of 3 cm or smaller [10,11]. Among the tumors excised by VABB in this study, benign phyllodes tumors accounted for only 0.77%. The frequency is comparable to other reports. As we did not perform the preoperative core-needle gun biopsy, we performed excision of the benign tumor without knowing of the phyllodes tumor. When a patient was diagnosed with a benign phyllodes tumor, on permanent biopsy, additional re-excision issues were discussed, but most patients chose observation as a clinical course. Our previous articles reported a high rate of complete excision that was attributable to rich experience with VABB, as well as a residual rate of only 5% upon follow-up ultrasonography taken at intervals of 3 to 6 months [10,11]. In these cases, the 'Watch and Wait' program was run instead of performing immediate surgical re-excision because additional wide local excision can be performed later in case recurrence is observed upon active follow-up.
The mean age of patients with phyllodes tumors is 45 years, which is approximately 20 years older than the average age of patients with fibroadenoma [28]; phyllodes tumors are rare in juveniles [25,26] and Latin-American whites [29] and Asians [14] have the highest incidence rate. In this study, patients in their twenties or thirties accounted for about 82%, with a mean age of 31.6 years. This is low compared with findings of other reports. It has been reported that phyllodes tumors are equally observed in the right and left breast, and that they frequently occur at the upper outer quadrant [14]. In this study, the right to left ratio was 52:48, and the frequency of tumors in the upper outer quadrant was the highest, with 61.4%. It is reported that a phyllodes tumor is smooth, well-defined, and as segment-like as fibroadenoma on mammography, and that it shows homogenous internal echo or smooth, well-defined features (including cystoma) on ultrasonography. It is reported to be difficult to distinguish benign phyllodes tumors from malignant ones on mammography or ultrasonography [30]. In this study, BI-RADS categories 3 and 4a were observed in 22 (71.0%) and 9 cases (29.0%), respectively, on ultrasonography, meaning it is difficult to distinguish benign phyllodes tumors and malignant ones until a biopsy is performed, and that the frequency of category 4a is high even with those diagnosed as benign phyllodes tumor. Clinically, phyllodes tumors show the appearance of rapid-growing benign nodules, and in some cases they suddenly enlarge after having grown slowly for several years. Malignant tumors grow more rapidly and are larger than benign ones, and sometimes a tumor over 20 cm in size is observed. However, such clinical findings cannot be used as an index for distinguishing benign tumors from malignant ones [15]. In this study, VABB was performed in small nodules, due to the characteristics of the procedure, and 67.4% of the nodules were 2 cm or smaller, with a mean size of 1.60 cm. The authors of this study believe that wide local excision is more appropriate than VABB in reducing local recurrence for lesions suspected to be phyllodes tumors upon core-needle biopsy; this is the case because it is difficult to ensure the tumor is sufficiently excised, by VABB, to expect the resection margin to be negative in cases of large lumps of over 3 cm. However, to conclude the clinical outcome of VABB versus conventional surgical excision in benign phyllodes tumors, a randomized prospective study should be performed.
In this study, with a mean follow-up period of 75.9 months, local recurrence was observed in 1 case 11 months after VABB, giving a local recurrence rate of 3.2%. Taking into account that follow-up period was not short, local recurrence rate is considerably low compared to local recurrence rate of conventional surgical excision, previously reported as ranging from 10% to 40%, with a mean value of approximately 15% [14,15]. This result, which can be explained by accurate and complete excision, was achieved via real-time ultrasonographic targeting of hypoechoic lesion during the entirety of VABB procedures. Consequently, an immediate reoperation may not always be required for benign phyllodes tumors diagnosed after VABB. In case residual tissues are not observed upon the 3-month follow-up ultrasonography, elaborate follow-up is carried out, and wide local excision may be performed when recurrence is confirmed later. Results from a more prolonged follow-up will be reported in the future.
VABB is an effective and safe procedure; it can remove most benign lesions in breasts in a short period of time and through a small window, without scars or complications. In this study, follow-up without reoperation was carried out at intervals of 3 to 6 months on the 31 lesions of 28 patients definitively diagnosed with benign phyllodes tumors, by VABB, for benign tumors; these individuals were judged as completely excised, without residual tissues on ultrasonography. No cases of local recurrence or distant metastasis were observed, with the exception of 1 case of local recurrence. If benign phyllodes tumors are diagnosed and sufficiently excised by VABB, observing the clinical course may be considered, rather than performing immediate wide local excision, although more prolonged observation is necessary.
Figures and Tables
 | Figure 1(A) A 1.3-cm palpable mass was located in lower outer quadrant of right breast. On ultrasonography, the lesion was a well-defined oval benign tumor of Breast Imaging Reporting and Data System (BI-RADS) category 3. The specimen was a benign biphasic tumor with a prominent stroma. The epithelial component showed adenosis. The stroma was widened and the stromal cellularity was increased. The mitoses were rare (H&E stain, B: ×40, C: ×200). |
 | Figure 2(A) A palpable local recurrence of Breast Imaging Reporting and Data System (BI-RADS) category 4a was found on follow-up ultrasonography. The recurred mass was also a benign biphasic tumor very similar to the primary lesion (H&E stain, B: ×40, C: ×200). |
References
1. Feuer EJ, Wun LM, Boring CC, Flanders WD, Timmel MJ, Tong T. The lifetime risk of developing breast cancer. J Natl Cancer Inst. 1993. 85:892–897.

2. Buchanan EB. Cystosarcoma phyllodes and its surgical management. Am Surg. 1995. 61:350–355.
3. Müller J. Uber den feineren Ban und Die Formen der Krankaften Geschwulste. 1838. Berlin: G. Reimer;54–57. Cited from Chen WH, Cheng SP, Tzen CY, Yang TL, Jeng KS, Liu CL, et al. Surgical treatment of phyllodes tumors of the breast: retrospective review of 172 cases. J Surg Oncol 2005;91:185-94.
4. World Health Organization. Histological typing of breast tumors. Tumori. 1982. 68:181–198.
5. Joshi SC, Sharma DN, Bahadur AK, Maurya R, Kumar S, Khurana N. Cystosarcoma phyllodes: our institutional experience. Australas Radiol. 2003. 47:434–437.

6. Deeming G, Divakaran R, Butterworth D, Foster M. Temporomandibular region metastasis from cystosarcoma phyllodes: a case report and review of the literature. J Craniomaxillofac Surg. 2003. 31:325–328.

7. Guerrero MA, Ballard BR, Grau AM. Malignant phyllodes tumor of the breast: review of the literature and case report of stromal overgrowth. Surg Oncol. 2003. 12:27–37.

8. Shabahang M, Franceschi D, Sundaram M, Castillo MH, Moffat FL, Frank DS, et al. Surgical management of primary breast sarcoma. Am Surg. 2002. 68:673–677.
9. Park HL, Kwak JY, Lee SH, Kim JY, Kim KI, Kim WW, et al. Excision of benign breast disease by ultrasound-guided vacuum assisted biopsy device (Mammotome). J Korean Surg Soc. 2005. 68:96–101.
10. Park HL, Kwak JY, Jung H, Lee SH, Shim JY, Kim JY, et al. Is mammotome excision feasible for benign breast mass bigger than 3 cm in greatest dimension? J Korean Surg Soc. 2006. 70:25–29.
11. American College of Radiology, BI-RADS Committee. ACR BI-RADS Breast Imaging and Reporting Data System: Breast Imaging Atlas. 2003. 4th ed. Reston: American College of Radiology.
12. Treves N, Sunderland DA. Cystosarcoma phyllodes of the breast: a malignant and a benign tumor: a clinicopathological study of seventy-seven cases. Cancer. 1951. 4:1286–1332.

13. Noguchi S, Motomura K, Inaji H, Imaoka S, Koyama H. Clonal analysis of fibroadenoma and phyllodes tumor of the breast. Cancer Res. 1993. 53:4071–4074.
14. Chua CL, Thomas A, Ng BK. Cystosarcoma phyllodes: a review of surgical options. Surgery. 1989. 105(2 Pt 1):141–147.
15. Ciatto S, Bonardi R, Cataliotti L, Cardona G. Phyllodes tumor of the breast: a multicenter series of 59 cases. Coordinating Center and Writing Committee of FONCAM (National Task Force for Breast Cancer), Italy. Eur J Surg Oncol. 1992. 18:545–549.
16. Cant PJ, Madden MV, Close PM, Learmonth GM, Hacking EA, Dent DM. Case for conservative management of selected fibro-adenomas of the breast. Br J Surg. 1987. 74:857–859.

17. Zurrida S, Bartoli C, Galimberti V, Squicciarini P, Delledonne V, Veronesi P, et al. Which therapy for unexpected phyllode tumour of the breast? Eur J Cancer. 1992. 28:654–657.

18. Reinfuss M, Mituś J, Duda K, Stelmach A, Ryś J, Smolak K. The treatment and prognosis of patients with phyllodes tumor of the breast: an analysis of 170 cases. Cancer. 1996. 77:910–916.

19. Pietruszka M, Barnes L. Cystosarcoma phyllodes: a clinicopathologic analysis of 42 cases. Cancer. 1978. 41:1974–1983.

20. Ward RM, Evans HL. Cystosarcoma phyllodes. A clinicopathologic study of 26 cases. Cancer. 1986. 58:2282–2289.

21. Hart WR, Bauer RC, Oberman HA. Cystosarcoma phyllodes. A clinicopathologic study of twenty-six hypercellular periductal stromal tumors of the breast. Am J Clin Pathol. 1978. 70:211–216.

22. Moffat CJ, Pinder SE, Dixon AR, Elston CW, Blamey RW, Ellis IO. Phyllodes tumours of the breast: a clinicopathological review of thirty-two cases. Histopathology. 1995. 27:205–218.

23. Cohn-Cedermark G, Rutqvist LE, Rosendahl I, Silfverswärd C. Prognostic factors in cystosarcoma phyllodes. A clinicopathologic study of 77 patients. Cancer. 1991. 68:2017–2022.

24. Palmer ML, De Risi DC, Pelikan A, Patel J, Nemoto T, Rosner D, et al. Treatment options and recurrence potential for cystosarcoma phyllodes. Surg Gynecol Obstet. 1990. 170:193–196.
25. Amerson JR. Cystosarcoma phyllodes in adolescent females. A report of seven patients. Ann Surg. 1970. 171:849–856.
26. Adachi Y, Matsushima T, Kido A. Phyllodes tumor in adolescents. Report of two cases and and review of the literature. Breast Dis. 1993. 6:285–293.
27. Bartoli C, Zurrida S, Veronesi P, Bono A, Chiesa F, Cosmacini P, et al. Small sized phyllodes tumor of the breast. Eur J Surg Oncol. 1990. 16:215–219.
28. Oberman HA. Cystosarcoma phyllodes: a clinicopathologic study of hypercellular periductal stromal neoplasms of breast. Cancer. 1965. 18:697–710.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download