Abstract
Purpose
Patients with recurrent breast cancer usually die of their disease, even after radical surgery and adjuvant therapies which could reduce the odds of dying. Many studies analyzed and compared patients who died of recurrent disease with those that died without recurrent disease. However, less attention has been paid to evaluating factors associated with the timing of recurrence. Thus, the objective of this study is to investigate the correlation between various factors and the timing of recurrence.
Methods
We retrospectively reviewed the data of 95 recurrent breast cancer patients who underwent curative surgery to determine the prognostic factors such as menopausal status, operation method, stage, nodal status, histologic grade, nuclear grade, extensive intraductal carcinoma component, hormone receptor, p53, c-erbB-2, Ki-67, and molecular subtype. We had attempted to compare the recurrent patients within 2 years after operation and adjuvant chemotherapies as the early recurrence with those over 2 years as the late recurrence.
Results
Histologic grade (p=0.005), nuclear grade (p<0.001), p53 (p=0.022), and Ki-67 (p<0.001) were significant different factors that influenced the systemic recurrence between early recurrence and late recurrence. In stage I/II, histologic grade (p=0.001), nuclear grade (p<0.001), and Ki-67 (p=0.005) were significant factors that influenced the systemic early recurrence. In stage III, nuclear grade (p=0.024), and Ki-67 (p=0.001) were significant factors that influenced the systemic early recurrence. But subtypes (p=0.189, p=0.132, p=0.593, p=0.083) are not associated with the timing of recur rence.
According to the Annual Report of Korea Central Cancer Registry in 2009 the number of breast cancer occurrences for women's in Korea in 2007 is 15.1%, the second highest one next to thyroid cancer [1].
Recently the treatment outcome of breast cancer has been improved owing to the development in curative surgery, chemotherapy and endocrine therapy; nevertheless, about 25% to 30% of the patients having no axillary lymph node metastasis and about 75% to 80% of the patients having axillary lymph node metastasis experience recurrence in 10 years, and most of them die due to the metastatic breast cancer [2,3]. As a result, studies on the factors that influence prognosis have been completed. The factors known up to now are the axillary lymph node metastasis, tumor's size, the histologic type and differentiation degree of tumors, the receptors of estrogen and progesterone, and overexpression of the genes p53 and c-erbB-2 [4].
However, these studies focused on comparing the patients who died due to recurrences and the patients who were alive, and they have not evaluated the important indexes which have relationship with recurrence period, though 70% of the breast cancer patients experience recurrences in 3 years [5,6] and patients with early recurrence experience a shorter median survival than patients with late recurrence [7].
In this context, this study was performed to evaluate the factors influencing recurrence period in the cases of the patients who experienced recurrence after first treatment of breast cancer.
The 95 cases of metastatic breast cancer patients who had systemic recurrences had curative surgeries at the Breast Cancer Clinic of Gachon University Gill Hospital between January 2002 to December 2008. This study was approved by the Institutional Review Board of Gachon University Gil Hospital (GIRBA 2769-2012).
We evaluated retrogressively the recurrence features in regard to patient's age, menopausal timing, method of surgery, stage, nodal status, histologic differentiation, existence of estrogen receptor, existence of progesterone receptor, existence of an extensive intraductal carcinoma component (EIC), existence of overexpression of genes p53 and c-erbB-2, expression degree of Ki-67, molecular subtype (luminal A type, luminal B type, HER2 positive type, triple negative type) and the supplementary curing such as chemotherapy, radiation therapy or endocrine therapy after curative surgery.
We evaluated the factors influencing the recurrence period for the patients who had recurrence after the first treatment of breast cancer by classifying them into two groups; the first group of early recurrence in which they had the recurrence before 2 years from the completion of curative surgery and chemotherapy and the second group of late recurrence in which they had the recurrence after 2 years from the completion of treatment. Because 70% of breast cancer patients experience recurrences within 3 years, we adopted these criteria and some of these patients were done with radiation therapy and others were with endocrine therapy when needed.
The data were processed with SPSS version 18.0 (SPSS Inc., Chicago, USA). The correlation between each clinopathologic factor and recurrent period was analyzed with chi-square test. And for the analysis of statistical significance of patient distribution between the groups nonparametric chi-square test was used. A p-value <0.05 was considered as statistically significant.
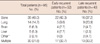
The average period of monitoring of the patients is 53.5 months (range, 6.4-116.5 months). The general characteristics of patients are presented in Table 1. Each patient was that was classified according to nodal status and stage. After curative surgery, chemotherapy and radiation therapy and endocrine therapy were done as supplementary curing. For chemotherapy all patients received chemotherapy and lymph node negative breast cancer patients received adjuvant systemic treatment with cyclophosphamide, methotrexate, 5-fluorouracil (CMF) chemotherapy and lymph node positive breast cancer patients received adjuvant systemic treatment with anthracycline based regimen chemotherapy.
Systemic recurrence sites are presented in Table 2. When bone scan was positive, bone metastasis was confirmed by magnetic resonance imaging (MRI). Lung metastasis was confirmed via lung biopsy, pleural cytology or serial follow up, when the chest computed tomography (CT) was positive. When the brain CT was positive, brain metastasis was confirmed by MRI and when liver CT was positive, liver metastasis was confirmed by MRI or serial follow up and other parts (mediastinal lymph node metastasis, supraclavicular lymph node metastasis) was confirmed by biopsy.
We checked the statistical significance between two groups: the first group of early recurrence (recurrence 2 years before the completion of curative surgery and chemotherapy) and the second group of late recurrence (recurrence after 2 years from the completion of treatment).
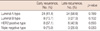
As for the stage, there was statistically significant difference (p=0.019) between early recurrence and late recurrence but in nodal status there was no statistically significant difference between them (p=0.365) (Table 3).
In histologic differentiation there was a statistically significant difference (p=0.005) between early recurrence and late recurrence. The nucleus differentiation also showed a statistically significant difference (p<0.001). A statistically significant difference was found in p53 (p=0.022) and Ki-67 (p<0.001) (Table 3).
We checked the statistical significance between two groups at each stage.
As for Stage I/II, the histologic differentiation there was statistically significant difference (p=0.001) between early recurrence and late recurrence and in nucleus differentiation there was also a statistically significant difference (p<0.001). A statistically significant difference was also found for Ki-67 (p=0.005) (Table 4).
As for Stage III, the nucleus differentiation (p=0.024) and Ki-67 (p=0.001) showed a statistically significant difference (Table 5).
As far as the subtype, the luminal A type has many instances of late recurrence but there was no statistical difference (p=0.189). Also luminal B type, HER2 positive type and triple negative type had many instances of early recurrence, but there was no statistical difference (p=0.132, p=0.593, p=0.083) (Table 6).
In general, metastasis after breast cancer treatment is relatively particular that it is exclusively concentrated on specific body parts. The most favorable systemic metastasis parts were reported by Kamby et al. [8] as: bones 31%, lungs 19%, and liver 15% and similar things were reported domestically. In this study metastasis was found in the bones 38 patients (40.0%), lungs 14 patients (14.7%), brain 6 patients (6.3%), liver 5 patients (5.3%) and other places 2 patients (2.1%), and 30 patients (31.6%) had recurrence in more than two parts. In early recurrence 17 patients (32.7%) had recurrence at more than two parts and in late recurrence 13 patients (34.2%) had recurrence at more than two parts; there is no statistically significant difference. Hence, it is thought that there is no relationship between the parts of recurrence and the period of recurrence.
We studied the factors influencing the recurrence period for the patients who had recurrence after the first treatment of breast cancer by classifying them into two groups: 1) early recurrence in which they had the recurrence before 2 years from the completion of curative surgery and chemotherapy and 2) which they had the recurrence after 2 years from the completion of treatment.
Debonis et al. [9] reported that metastasized parts, combined chemotherapy and disease-free interval influence the survival rate. And Pater et al. [10] reported that disease-free interval, metastasized parts and the pathologic stage of the cancer at the time of diagnosis, histologic subtype and primary tumor size influence the survival rate. In this study, positive axillary lymph node metastasis groups are for both the early recurrence and late recurrence, but there is no statistically significant difference between the groups. On the other hand, the stage is statistically significant between early recurrence and late recurrence. And it means that nodal status is not worth of a risk factor in early recurrence.
Breast cancers are diagnosed mostly for women in their 40's in Korea. In this study the patients were between ages 35 and 50 were 52.6% and occupied the biggest part. In case breast cancer appears when a client is young, it was generally thought that the more invasive and worse in prognosis, but it is known that there is no relationship between the prognosis and ages [11]. On the contrary, Retsky et al. [12] reported that there is significant difference in early recurrence danger between premenopausal women and postmenopausal ones. In this study premenopausal women are more for both of early recurrence and late recurrence, but there is no statistically significant difference between the groups. Also in each stage, there is no statistically significant difference between the groups.
The most widely used standard to measure the differentiation of breast cancer is Scaff-Bloom-Richardson Classification, in which grades from I to III are given after considering cell differentiation, the degree of polymorphism status and frequency of nucleus division. Kute et al. [13] reported that histologic differentiation is a prognostic factor for breast cancer. On the other hand, Younes and Laucirica [14] reported that it is not worth consideration as a prognostic factor. In this study, the histologic differentiation showed a statistically significant difference between early recurrence and late recurrence. And as for Stage I/II, in histologic differentiation there is statistically significant difference between early recurrence and late recurrence. But as for Stage III, in histologic differentiation there is not a statistically significant difference between early recurrence and late recurrence. So it means that histologic differentiation is worth being included as a risk factor in predicting early recurrence at early breast cancer. Also, in nucleus differentiation there is a statistically significant difference between early recurrence and late recurrence. And as for both stages, in nucleus differentiation there is statistically significant difference within them. So it means that nucleus differentiation is worth of a risk factor in early recurrence, irrespective of stage.
Noh et al. [15] reported that EIC can be a cause of local recurrence, because EIC can exist around invasive cancer and can exist around primary cancer that looks visually sound. Park et al. [16] reported that EIC has a relationship with systemic recurrence as well as local recurrence. In this study there is no statistical significance in all groups for EIC.
In many studies it is known that a positive hormone receptor is better than a negative one for prognosis [17,18]. In this study, there were many patients with a positive hormone receptor in both of early recurrence and late recurrence. But there is no statistically significant difference between the groups. So, there is no relationship with early recurrence.
It is reported that c-erbB-2 has a negative correlation with the estrogen receptor and progesterone receptor, appears well in high nucleus level, and it appears better in invasive cancer [19,20]. In the study of molecular biological factors it is the only indicator to have a bad prognosis in breast cancer [21,22]. In this study there is no statistical significance in all groups with c-erbB-2.
The p53 gene mutation appears in the early stage of breast cancer. Barnes et al. [23] argued that p53 has relationship with patients' prognosis regardless of lymph node metastasis. In this study there is a statistically significant difference between early recurrence and late recurrence as a whole. But there is no statistically significant difference between early recurrence and late recurrence at each stage. So there is relationship with early recurrence, but p53 is dependent factor associated with stage.
Among the predictive factors and prognostic factors under molecular biological study Ki-67 is a monoclonal antibody appearing in all cell cycles except G0 and is a good indicator of cell proliferation. It is under dispute that Ki-67 can be regarded as an independent predictive factor and prognostic factor; many studies reported Ki-67's effectiveness as a predictive factor and prognostic factor for breast cancer [24-26]. In this study there is a statistically significant difference between early recurrence and late recurrence. And as for both stages, in Ki-67 there is statistically significant difference with them. So it means that Ki-67 is worthy as a risk factor in early recurrence irrespective in stage. Ki-67 is an independent factor that is associated without stage.
Many studies have shown both the triple negative and HER2 positive subtypes to have poorer clinical, pathologic and molecular prognoses. The triple negative group has the worst overall and disease-free survival [27-29]. But in this study luminal A type had many late recurrences but there is no statistical difference. Also luminal B type, HER2 positive type and triple negative type had many early recurrences but there is no statistical difference. Therefore, subtype is not associated with the timing of recurrence.
In systemic recurrent breast cancer patients there is statistically significant difference between early recurrence and late recurrence in histologic differentiation, nucleus differentiation, p53 and Ki-67. When the recurrence periods depending on the each stage are compared, there is statistically significant difference between early recurrence and late recurrence in histologic differentiation, nucleus differentiation and Ki-67 for stage I/II. There is statistically significant difference between early recurrence and late recurrence in nucleus differentiation and Ki-67 for stage III. But subtypes are not associated with the timing of recurrence.
Hence, tailored therapy and detailed follow-up are thought to be necessary for these patients. Additional future predictive risk factor focused large scale investigations for molecular biological factors, which are currently under investigation, are required.
Figures and Tables
References
1. Ministry for Health, Welfare and Family Affairs. Annual Report of Cancer Incidence (2007), Cancer Prevalence (2007), and Survival (1993-2007) in Korea. 2009. Seoul: Ministry for Health, Welfare and Family Affairs;14–20.
2. Chevallier B, Fumoleau P, Kerbrat P, Dieras V, Roche H, Krakowski I, et al. Docetaxel is a major cytotoxic drug for the treatment of advanced breast cancer: a phase II trial of the Clinical Screening Cooperative Group of the European Organization for Research and Treatment of Cancer. J Clin Oncol. 1995. 13:314–322.

3. Khayat D, Antoine E. Docetaxel in combination chemotherapy for metastatic breast cancer. Semin Oncol. 1997. 24:4 Suppl 13. S13-9–S13-26.
4. Son BH, Ahn SH, Kwak BS, Kim JK, Kim HJ, Hong SJ, et al. The recurrence rate, risk factors and recurrence patterns after surgery in 3,700 patients with operable breast cancer. J Breast Cancer. 2006. 9:134–144.

5. Bland KI, Copeland EM III. Schwartz SI, Shires GT, Spencer FC, editors. Breast. Principles of Surgery. 1994. 6th ed. New York: McGraw-Hill;554–557.
6. Baum M, Badwe RA. Wise L, Johnson H, editors. Does surgery influence the natural history of breast cancer? Breast Cancer: Controversies in Management. 1994. Armonk: Futura Pub.;61–69.
7. Lyman GH, Kuderer NM, Lyman SL, Debus M, Minton S, Balducci L, et al. Survival following early versus late recurrence of breast cancer. 1997. American Society of Clinical Oncology (ASCO) Annual Meeting. 1997. Abstract #633.
8. Kamby C, Vejborg I, Kristensen B, Olsen LO, Mouridsen HT. Metastatic pattern in recurrent breast cancer. Special reference to intrathoracic recurrences. Cancer. 1988. 62:2226–2233.

9. Debonis D, Terz JJ, Eldar S, Hill LR. Survival of patients with metastatic breast cancer diagnosed between 1955 and 1980. J Surg Oncol. 1991. 48:158–163.

10. Pater JL, Mores D, Loeb M. Survival after recurrence of breast cancer. Can Med Assoc J. 1981. 124:1591–1595.
11. Min YK, Kim NR, Cho SJ, Kim A, Bae JW, Koo BH. The clinical significance and prognosis of Korean young age (younger or 35 year old) onset breast cancer. J Korean Breast Cancer Soc. 2001. 4:74–79.

12. Retsky M, Demicheli R, Hrushesky W. Premenopausal status accelerates relapse in node positive breast cancer: hypothesis links angiogenesis, screening controversy. Breast Cancer Res Treat. 2001. 65:217–224.

13. Kute TE, Russell GB, Zbieranski N, Long R, Johnston S, Williams H, et al. Prognostic markers in node-negative breast cancer: a prospective study. Cytometry B Clin Cytom. 2004. 59:24–31.

14. Younes M, Laucirica R. Lack of prognostic significance of histological grade in node-negative invasive breast carcinoma. Clin Cancer Res. 1997. 3:601–604.
15. Noh DY, Han SH, Lee ES, Lee SJ. Korean Breast Cancer Society. The prognostic factors and the predictive factors. The Breast. 1999. Seoul: Ilchokak;388–412.
16. Park SH, Kim SI, Park BW, Lee KS. Prognostic factors in axillary lymph node negative breast cancer. J Korean Breast Cancer Soc. 2004. 7:111–120.

17. Ma H, Bernstein L, Pike MC, Ursin G. Reproductive factors and breast cancer risk according to joint estrogen and progesterone receptor status: a meta-analysis of epidemiological studies. Breast Cancer Res. 2006. 8:R43.

18. Dunnwald LK, Rossing MA, Li CI. Hormone receptor status, tumor characteristics, and prognosis: a prospective cohort of breast cancer patients. Breast Cancer Res. 2007. 9:R6.

19. Prati R, Apple SK, He J, Gornbein JA, Chang HR. Histopathologic characteristics predicting HER-2/neu amplification in breast cancer. Breast J. 2005. 11:433–439.

20. Bilous M, Ades C, Armes J, Bishop J, Brown R, Cooke B, et al. Predicting the HER2 status of breast cancer from basic histopathology data: an analysis of 1500 breast cancers as part of the HER2000 International Study. Breast. 2003. 12:92–98.

21. Riou G, Mathieu MC, Barrois M, Le Bihan ML, Ahomadegbe JC, Bénard J, et al. c-erbB-2 (HER-2/neu) gene amplification is a better indicator of poor prognosis than protein over-expression in operable breast-cancer patients. Int J Cancer. 2001. 95:266–270.

22. Bianchi S, Palli D, Falchetti M, Saieva C, Masala G, Mancini B, et al. ErbB-receptors expression and survival in breast carcinoma: a 15-year follow-up study. J Cell Physiol. 2006. 206:702–708.

23. Barnes DM, Dublin EA, Fisher CJ, Levison DA, Millis RR. Immunohistochemical detection of p53 protein in mammary carcinoma: an important new independent indicator of prognosis? Hum Pathol. 1993. 24:469–476.

24. Trihia H, Murray S, Price K, Gelber RD, Golouh R, Goldhirsch A, et al. Ki-67 expression in breast carcinoma: its association with grading systems, clinical parameters, and other prognostic factors: a surrogate marker? Cancer. 2003. 97:1321–1331.
25. Pinto AE, André S, Pereira T, Nóbrega S, Soares J. Prognostic comparative study of S-phase fraction and Ki-67 index in breast carcinoma. J Clin Pathol. 2001. 54:543–549.

26. Jung SY, Han W, Shin HJ, Lee JE, Hwang KT, Hwang SE, et al. Usefulness of Ki-67 as a prognostic factor in lymph node-negative breast cancer. J Breast Cancer. 2006. 9:41–46.

27. Carey LA, Perou CM, Livasy CA, Dressler LG, Cowan D, Conway K, et al. Race, breast cancer subtypes, and survival in the Carolina Breast Cancer Study. JAMA. 2006. 295:2492–2502.





 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download