Abstract
Purpose
Although most patients with stage I breast cancer have a good prognosis, their clinical outcomes may vary significantly. We assessed clinical outcomes and prognostic factors in stage I breast cancer patients with and without triple-negative breast cancer (TNBC) phenotype.
Methods
Of 2,489 patients undergoing breast cancer surgery between January 1998 and December 2002, 554 (22.3%) had stage I breast cancer (tumor size ≤2 cm, and lymph node-negative). TNBC was defined as a primary tumor negative for estrogen and progesterone receptors (Allred scores <3/8) and for HER2/neu (0-1+ by immunohistochemistry).
Results
Of the 554 patients with stage I breast cancer, 78 (14.1%) had TNBC. A significant proportion of TNBC patients had histologic grade 3 tumors (47.4% vs. 34.5%, p=0.031) and tumors >1 cm (87.2% vs. 75.8%, p=0.028) and received adjuvant chemotherapy (79.5% vs. 44.7%, p<0.001). During a median follow-up time of 8.7 years, 72 patients experienced tumor recurrences; 18 (23.1%) in the TNBC group and 54 (11.3%) in the non-TNBC group (p=0.010), with cumulative 3-year rate of recurrence of 12.8% and 5.3%, respectively (p=0.010). Ten-year relapse-free survival (RFS; 75.6% vs. 87.5%, p=0.004) and overall survival (OS; 83.0% vs. 91.4%, p=0.002) rates were significantly lower in the TNBC group. Multivariate analysis showed that triple negativity and histologic grade were independent predictors of shorter RFS and OS.
Screening mammography have increased detection of early breast cancers, and aggressive multimodal treatment has successfully reduced the mortality rate of breast cancer [1]. Although patients with stage I breast carcinoma (pT1N0) generally show very good prognosis, some patients experience disease recurrence and die of systemic disease [2].
Prognostic and predictive factors have been widely used in treatment decisions for breast cancer. Human epidermal growth factor receptor 2 (HER2)/neu overexpression has been associated with poorly differentiated high-grade tumors, high rates of cell proliferation and lymph node (LN) involvement, and relative resistance to certain types of chemotherapy [3,4]. Currently, however, HER2/neu positive patients can be treated with targeted agents, including trastuzumab, which have increased their survival in adjuvant settings [5-8].
Triple-negative breast cancer (TNBC) is defined as hormone receptor-negative and HER2/neu-negative breast cancer. In contrast to patients with hormone receptor-positive or HER2/neu-positive breast cancer, patients with TNBC derive no benefit from endocrine therapy or molecular targeted treatment due to the lack of the appropriate targets for these drugs. Moreover, several retrospective and epidemiologic studies have shown that the triple-negative (TN) phenotype is associated with a poorer prognosis and more aggressive clinical features than other subtypes [9-11]. Although most patients with TNBC present with advanced stage tumors at diagnosis, about 10% present with stage I [2,12]. However, predictive and prognostic values of TNBC phenotype, especially in patients with early stage breast carcinoma, are relatively undetermined [13-16].
We therefore investigated the clinical outcomes and prognostic factors of patients with stage I early breast cancer. Also, we compared the clinicopathologic characteristics and prognosis of TNBC with those of non-TNBC in a cohort of stage I breast carcinoma.
Of the 2,489 breast cancer patients who underwent surgery from January 1998 to December 2002, 565 (22.7%) were diagnosed with stage I breast carcinoma (tumor size ≤ 2 cm, and LN-negative on pathologic examination) and had available results of immunohistochemistry (IHC) for hormonal receptors and HER2/neu. From this, we excluded 11 patients with ER-negative, PR-negative, and HER2/neu 2+ by IHC without fluorescence in situ hybridization (FISH) results because no data from the FISH was available. Finally 554 patients were included in the study. This study was approved by the Institutional Review Board. Using a database from the tumor registry at Asan Medical Center, we collected their clinical information, including age at initial diagnosis, type of surgery, adjuvant therapy, tumor recurrence or distant metastases and follow-up status.
Pathologic parameters, including tumor size, histologic subtype, histologic grade, nuclear grade, and resection margin status were evaluated using archived hematoxylin and eosin (H&E)-stained slides. Histologic grade was assessed using a modified Bloom-Richardson classification, and nuclear grade was evaluated according to a modification of Black's nuclear grading system.
IHC assay was used to evaluate the levels of expression of estrogen receptor (ER), progesterone receptor (PR), and HER2/neu. Formalin-fixed, paraffin-embedded blocks of tumor tissue were sectioned at 4-µm thickness; the sections were deparaffinized in xylene, rehydrated for 5 minutes, immersed in citrate buffer (pH 6.0) and incubated in a microwave oven for antigen retrieval. The slides were subsequently incubated in 0.3% hydrogen peroxide for 20 minutes to block endogenous peroxidase activity, and then washed and incubated overnight at 4℃ with primary antibodies against ER (1:30 dilution; Dinona, Seoul, Korea), PR (1:100 dilution; Dinona), and HER2/neu (1:250 dilution; DAKO, Carpinteria, USA). The slides were washed, incubated with biotinylated secondary antigoat antibodies, washed, and incubated with peroxidase-labeled streptavidin. Reaction products were visualized by immersing the slides in diaminobenzidine tetrachloride and counterstaining with Harris hematoxylin.
ER and PR positivity was defined as strong nuclear staining in at least 3/8 of the tumor cells examined [4]. HER2/neu positivity was defined as strong (3+) membranous staining in at least 10% of tumor cells, whereas scores of 0 to 2+ were regarded as negative. A primary tumor was defined as a TNBC if ER, PR, and HER2/neu were all negative (0 or 1+ by IHC). Primary tumor with negative ER, PR, and HER2/neu 2+ by IHC without FISH results was not classified as TNBC.
The relationships between triple-negativity and other clinicopathological parameters were evaluated using the χ2 test or Fisher's exact test, as appropriate. The Kaplan-Meier method was used to estimate survival with differences analysis by the log-rank test. Relapse-free survival (RFS) was defined as the time from the date of surgery to the date of documented recurrence. Overall survival (OS) was defined as the time from the date of surgery to the date of last follow-up or death. Cox's proportional hazards model was employed for multivariate analysis of prognostic factors. A p-value less than 0.05 was defined as statistically significant (SPSS version 18.0; SPSS Inc., Chicago, USA).
The median age of the 554 included patients was 46 years (range, 18-79 years), and the major pathologic type was invasive ductal carcinoma (98.7%). IHC assays showed expression of HER2/neu in tumors from 179 patients (32.3%) and hormone receptors in 427 (77.1%) patients including 394 (71.1%) positive for ER and 374 (67.5%) positive for PR (Table 1). We found that 130 tumors (23.5%) were hormonal receptor (HR)- and HER2/neu-positive, 297 (53.6%) were HR-positive and HER2/neu-negative, 49 (8.8%) were HR-negative and HER2/neu-positive, and 78 (14.1%) were HR- and HER2/neu-negative. Thus, of the 554 patients, 78 (14.1%) were categorized as having TNBC, and 476 (85.9%) were categorized as non-TNBC. Moreover, 125 patients (22.6%) had tumors ≤1 cm in diameter and 201 (36.3%) had tumors of histologic grade 3.
Among the 554 patients, 310 (56.0%) underwent modified radical mastectomy, and 244 (44.0%) underwent breast conserving operations followed by adjuvant radiotherapy. After surgery, 279 patients received adjuvant chemotherapy, including 153 who received four cycles of adriamycin and cyclophosphamide (AC), 61 who received six cycles of cyclophosphamide, methotrexate, 5-fluorouracil (CMF) and 61 who received daily doxifluridine for 6 months.
When we compared the clinicopathologic characteristics of the TNBC and non-TNBC groups (Table 2), we found that the median age of each was 46 years (p=0.799). Significantly greater proportions of TNBC than non-TNBC patients had histologic grade 3 tumors (47.4% vs. 34.5%, p=0.031), tumor >1 cm (87.2% vs. 75.8%, p=0.028) and were more likely to have received adjuvant chemotherapy (79.5% vs. 44.7%, p<0.001).
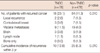
At a median follow-up of 8.7 years, 72 of the 554 patients (13.0%) experienced tumor recurrences in which 18 of 78 (23.1%) in the TNBC and 54 of 476 (11.3%) in the non-TNBC group (p=0.010). Sites of recurrence are shown in Table 3. The proportions of patients with brain (3 [3.8%] vs. 9 [1.9%]) and visceral (9 [11.8%] vs. 19 [4.0%]) metastases were significantly higher in the TNBC than in the non-TNBC group (p=0.027). The 3-year cumulative rate of recurrence was also significantly higher in the TNBC than in the non-TNBC group (12.8% vs. 5.3%, p=0.010).
The 10-year OS and RFS rates of all patients were 90.2% and 85.7%. We found that OS (hazard ratio, 0.364; 95% confidence interval [CI], 0.190-0.698) and RFS (hazard ratio, 0.468; 95% CI, 0.274-0.798) rates were significantly lower in the TNBC than in the non-TNBC group (Figure 1). The 10-year OS rates were 83.0% and 91.4%, respectively (p=0.002), whereas the 10-year RFS rates were 75.6% and 87.5%, respectively (p=0.004). When we compared survival in the 4 groups classified by HR and HER2/neu status-luminal A (HR-positive and HER2/neu-negative), luminal B (HR- and HER2/neu-positive), HER2+ (HR-negative and HER2/neu-positive), and TNBC, we found that survival rates were poorer in the TNBC than in the other 3 groups (Figure 2).
Univariate analysis of the prognostic impact of clinicopathological variables on patient survival showed that in addition to TNBC, histologic grade 3 and an absence of adjuvant chemotherapy as well as age <40 were significantly associated with poorer OS and RFS. On multivariate analysis using Cox's proportional hazards model, triple negativity was an independent prognostic factor for reduced RFS (hazard ratio, 1.816; 95% CI, 1.034-3.189) and OS (hazard ratio, 2.277; 95% CI, 1.135-4.571). Histologic grade 3 was also an independent predictor of shorter RFS (hazard ratio, 1.769; 95% CI, 1.100-2.847) and OS (hazard ratio, 2.369; 95% CI, 1.277-4.393) (Table 4).
Due to the low risk of relapse and death for stage I early breast cancer patients, a long-term follow-up is required to assess survival rates and detect statistically significant differences between RFS and OS. In present study, we analyzed 554 patients with stage I breast cancer, with a median follow-up period of 8.7 years. Of these patients, 14.1% (78/554) had TNBC and triple negativity served as the most important independent predictor of RFS and OS rates on multivariate analysis in stage I breast cancer patients. This suggests that triple negativity can be used as a reliable prognostic marker [9-11]. Furthermore, we found that the 3 year recurrence rate was significantly higher in patients with TNBC than non-TNBC breast cancer (12.8% vs. 5.3%), which is consistent with findings of TNBC being a more aggressive tumor phenotype [10,12,17]. We also found that visceral and brain metastases were more frequent in the TNBC group, which were consistent with previous results [18-23], indicating that prognosis of Korean patients with TNBC is similar to that of Western patients.
Fewer treatments are currently available for patients with TNBC than other subtypes, with cytotoxic chemotherapy being the only systemic modality available. A better response to chemotherapy in TNBC patients has suggested that their tumors are more chemosensitive, but a greater response to adjuvant or neoadjuvant chemotherapy did not guarantee better survival [14,19]. Similarly, we found that a higher percentage of TNBC than non-TNBC patients (79.5% vs. 44.7%) received adjuvant chemotherapy, but the former group had higher rates of recurrence and death, suggesting that adjuvant chemotherapy with current standard regimens did not overcome the poor prognosis of these patients [12,24].
Although our study was strengthened by the availability of survival data from the long term follow-up (median, 8.7 years), it also had several limitations. About 15% to 20% of HER2/neu 2+ patients at our center showed FISH positivity. Since HER2/neu 0-2+ determined by IHC was classified as HER2/neu 2-negative, some patients classified with the luminal A subtype may have had luminal B tumors. However, we excluded 11 patients who were ER-negative, PR-negative, and HER2/neu 2+ by IHC but without FISH results to avoid including any who may have been FISH-positive in the TNBC group. Although it is difficult to divide patients into exact molecular categories based on IHC alone, our grouping into the TNBC and non-TNBC groups seemed correct.
Several studies have reported that sporadic TNBC shares clinical and pathological features with hereditary BRCA1-related breast cancers [25]. The defect in DNA-repair pathways characteristic of BRCA1 related cancers may also occur in TNBC and may be more specifically targeted [26]. Cisplatin, a DNA damaging agent that has been shown to distrupt the BRCA1 pathway [27], has been used as neoadjuvant treatment in patients with TNBC [28]. In addition, poly (adenosine disphosphate-ribose) polymerase 1 (PARP1) has been targeted in patients with TNBC based on results which showed that combining PARP1 inhibitors with platinum chemotherapy induced DNA damage and potentiated chemotherapeutic cytotoxicity [29,30]. Therefore, new therapeutic strategies including platinum agents and PARP1 inhibitors may overcome the poor survival results observed in patients with TNBC. Many ongoing clinical trials are testing these regimens in patients with early stage and metastatic TNBC.
In conclusion, we found that triple negativity was a significant prognostic factor even in patients with stage 1 early breast cancer, being associated with a higher incidence of visceral metastases. Studies on novel therapeutic options targeting this aggressive type of breast cancer should be performed in larger groups of patients.
Figures and Tables
 | Figure 1Kaplan-Meier analysis of (A) relapse-free survival (RFS) and (B) overall survival according to triple-negative breast cancer (TNBC) phenotype. |
 | Figure 2Kaplan-Meier analysis of (A) relapse-free survival (RFS) and (B) overall survival according to hormonal receptor and HER2/neu status. TN=triple-negative. |
Table 1
Patient characteristics (n=554)

HR=hormonal receptor; TN=triple-negative; G=grade; Op=operation; MRM=modified radical mastectomy; BCO=breast conserving operation.
*Estrogen receptor (ER)+ (n=394), progesterone receptor (PR)+ (n=373), ER+ and PR+ (n=340); †Adriamycin with cyclophosphamide (AC; n=153), cyclophosphamide, methotrexate, and 5-fluorouracil (CMF; n=61), Doxifluridine (n=61); ‡Tamoxifen (n=269), aromatase inhibitor (n=116).
Notes
References
1. Wood WC, Muss HB, Solin LJ, Olopade OI. DeVita VT, Hellman S, Rosenberg SA, editors. Malignant tumors of the breast. Cancer: Principles and Practice of Oncology. 2005. 7th ed. Philadelphia: Lippincott Williams & Wilkins;610–615.
2. Bauer KR, Brown M, Cress RD, Parise CA, Caggiano V. Descriptive analysis of estrogen receptor (ER)-negative, progesterone receptor (PR)-negative, and HER2-negative invasive breast cancer, the so-called triplenegative phenotype: a population-based study from the California cancer Registry. Cancer. 2007. 109:1721–1728.

3. Allred DC, Clark GM, Tandon AK, Molina R, Tormey DC, Osborne CK, et al. HER-2/neu in node-negative breast cancer: prognostic significance of overexpression influenced by the presence of in situ carcinoma. J Clin Oncol. 1992. 10:599–605.

4. Le Doussal V, Tubiana-Hulin M, Friedman S, Hacene K, Spyratos F, Brunet M. Prognostic value of histologic grade nuclear components of Scarff-Bloom-Richardson (SBR). An improved score modification based on a multivariate analysis of 1262 invasive ductal breast carcinomas. Cancer. 1989. 64:1914–1921.

5. Piccart-Gebhart MJ, Procter M, Leyland-Jones B, Goldhirsch A, Untch M, Smith I, et al. Trastuzumab after adjuvant chemotherapy in HER2-positive breast cancer. N Engl J Med. 2005. 353:1659–1672.
6. Dahabreh IJ, Linardou H, Siannis F, Fountzilas G, Murray S. Trastuzumab in the adjuvant treatment of early-stage breast cancer: a systematic review and meta-analysis of randomized controlled trials. Oncologist. 2008. 13:620–630.

7. Romond EH, Perez EA, Bryant J, Suman VJ, Geyer CE Jr, Davidson NE, et al. Trastuzumab plus adjuvant chemotherapy for operable HER2-positive breast cancer. N Engl J Med. 2005. 353:1673–1684.

8. Joensuu H, Kellokumpu-Lehtinen PL, Bono P, Alanko T, Kataja V, Asola R, et al. Adjuvant docetaxel or vinorelbine with or without trastuzumab for breast cancer. N Engl J Med. 2006. 354:809–820.

9. Carey LA, Perou CM, Livasy CA, Dressler LG, Cowan D, Conway K, et al. Race, breast cancer subtypes, and survival in the Carolina Breast Cancer Study. JAMA. 2006. 295:2492–2502.

10. Dent R, Trudeau M, Pritchard KI, Hanna WM, Kahn HK, Sawka CA, et al. Triple-negative breast cancer: clinical features and patterns of recurrence. Clin Cancer Res. 2007. 13(15 Pt 1):4429–4434.

11. Gerson R, Alban F, Villalobos A, Serrano A. Recurrence and survival rates among early breast cancer cases with triple negative immunophenotype. Gac Med Mex. 2008. 144:27–34.
12. Kaplan HG, Malmgren JA, Atwood M. T1N0 triple negative breast cancer: risk of recurrence and adjuvant chemotherapy. Breast J. 2009. 15:454–460.

13. Parise CA, Bauer KR, Brown MM, Caggiano V. Breast cancer subtypes as defined by the estrogen receptor (ER), progesterone receptor (PR), and the human epidermal growth factor receptor 2 (HER2) among women with invasive breast cancer in California, 1999-2004. Breast J. 2009. 15:593–602.

14. Keam B, Im SA, Kim HJ, Oh DY, Kim JH, Lee SH, et al. Prognostic impact of clinicopathologic parameters in stage II/III breast cancer treated with neoadjuvant docetaxel and doxorubicin chemotherapy: paradoxical features of the triple negative breast cancer. BMC Cancer. 2007. 7:203.

15. Haffty BG, Yang Q, Reiss M, Kearney T, Higgins SA, Weidhaas J, et al. Locoregional relapse and distant metastasis in conservatively managed triple negative early-stage breast cancer. J Clin Oncol. 2006. 24:5652–5657.

16. Rhee J, Han SW, Oh DY, Kim JH, Im SA, Han W, et al. The clinicopathologic characteristics and prognostic significance of triple-negativity in node-negative breast cancer. BMC Cancer. 2008. 8:307.

17. Uhm JE, Park YH, Yi SY, Cho EY, Choi YL, Lee SJ, et al. Treatment outcomes and clinicopathologic characteristics of triple-negative breast cancer patients who received platinum-containing chemotherapy. Int J Cancer. 2009. 124:1457–1462.

18. Hines SL, Vallow LA, Tan WW, McNeil RB, Perez EA, Jain A. Clinical outcomes after a diagnosis of brain metastases in patients with estrogenand/ or human epidermal growth factor receptor 2-positive versus triplenegative breast cancer. Ann Oncol. 2008. 19:1561–1565.

19. Liedtke C, Mazouni C, Hess KR, André F, Tordai A, Mejia JA, et al. Response to neoadjuvant therapy and long-term survival in patients with triple-negative breast cancer. J Clin Oncol. 2008. 26:1275–1281.

20. Heitz F, Harter P, Lueck HJ, Fissler-Eckhoff A, Lorenz-Salehi F, Scheil-Bertram S, et al. Triple-negative and HER2-overexpressing breast cancers exhibit an elevated risk and an earlier occurrence of cerebral metastases. Eur J Cancer. 2009. 45:2792–2798.

21. Smid M, Wang Y, Zhang Y, Sieuwerts AM, Yu J, Klijn JG, et al. Subtypes of breast cancer show preferential site of relapse. Cancer Res. 2008. 68:3108–3114.

22. Ahn JS, Cho J, Kwon SY, Kang SH. Clinicopathologic characteristics and prognosis of early stage triple negative breast cancer: comparison with non-triple negative group. J Korean Surg Soc. 2009. 77:37–42.

23. Noh JM, Choi DH, Huh SJ, Park W, Yang JH, Nam SJ, et al. Patterns of recurrence after breast-conserving treatment for early stage breast cancer by molecular subtype. J Breast Cancer. 2011. 14:46–51.

24. Miller K, Wang M, Gralow J, Dickler M, Cobleigh M, Perez EA, et al. Paclitaxel plus bevacizumab versus paclitaxel alone for metastatic breast cancer. N Engl J Med. 2007. 357:2666–2676.

25. Lakhani SR, Reis-Filho JS, Fulford L, Penault-Llorca F, van der Vijver M, Parry S, et al. Prediction of BRCA1 status in patients with breast cancer using estrogen receptor and basal phenotype. Clin Cancer Res. 2005. 11:5175–5180.

26. Turner N, Tutt A, Ashworth A. Hallmarks of 'BRCAness' in sporadic cancers. Nat Rev Cancer. 2004. 4:814–819.

27. Tassone P, Tagliaferri P, Perricelli A, Blotta S, Quaresima B, Martelli ML, et al. BRCA1 expression modulates chemosensitivity of BRCA1-defective HCC1937 human breast cancer cells. Br J Cancer. 2003. 88:1285–1291.

28. Silver DP, Richardson AL, Eklund AC, Wang ZC, Szallasi Z, Li Q, et al. Efficacy of neoadjuvant Cisplatin in triple-negative breast cancer. J Clin Oncol. 2010. 28:1145–1153.

29. Alli E, Sharma VB, Sunderesakumar P, Ford JM. Defective repair of oxidative dna damage in triple-negative breast cancer confers sensitivity to inhibition of poly(ADP-ribose) polymerase. Cancer Res. 2009. 69:3589–3596.

30. O'Shaughnessy J, Osborne C, Pippen JE, Yoffe M, Patt D, Rocha C, et al. Iniparib plus chemotherapy in metastatic triple-negative breast cancer. N Engl J Med. 2011. 364:205–214.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download