Abstract
Purpose
Idiopathic granulomatous lobular mastitis (IGLM) is a rare chronic inflammatory disease of the breast with obscure etiology that mimics invasive carcinoma both clinically and radiologically. The treatment of IGLM remains controversial. The aim of proper management is to use a combination of medical and surgical treatment of this benign condition to achieve a good cosmetic result and low recurrence rate.
Methods
A retrospective analysis of 19 patients with IGLM is performed based on the findings of clinical, radiological, and pathological examinations. The results of two treatments are presented: medical treatment with oral corticosteroids, and consecutive surgical excision after a follow-up period of 20 months (range, 6-75 months).
Results
The majority of patients treated in this paper were young (mean, 34 years) parous women with a history of hormonal medication use. The main clinical finding is large, irregular, and painful mass. Hypoechoic lobulated, irregular tubular or oval shaped masses had been imaged by ultrasound. Mammographic findings were an ill-defined mass, enlarged axillary lymph nodes, asymmetric density, and architectural distortion. Diagnoses of IGLM had been established by cytological or histological examination. Symptoms subside and inflammatory changes regressed with medical treatment. The remaining lesions were excised by consecutive breast conserving surgery. The disease recurred in one patient during the follow-up period.
Conclusion
IGLM is an inflammatory breast disease found in young women who present with a large painful irregular mass, which mimics carcinoma, as a physical change. Breast imaging modalities are not helpful to differentiate IGLM from invasive cancer. The correct diagnosis is established by cytological or histological examination. Medical treatment with corticosteroids provides significant regression of the inflammatory disease, allowing more conservative surgery. Consecutive surgical excision of the remaining lesions with good cosmetic results provides definitive treatment and reduces the risk of recurrence.
IGLM is a rare chronic inflammatory disease of the breast that mimics cancer both clinically and mammographically [1]. The etiology of IGLM is still obscure. The cause may be the autoimmune process, infection, a chemical reaction associated with oral contraceptive pills, or even lactation. Lymphocyte and macrophage migration occurs as a result of ductal epithelium damage, and a local immune response is produced [2,3]. The clinical and radiologic features of IGLM are very similar to tuberculosis and carcinoma of the breast. The most common clinical finding is a unilateral, discrete breast mass. Histopathology generally provides a definitive diagnosis, which is characterized by necrotizing chronic granulomatous lobulitis with micro-abscesses [3-6]. The treatment of IGLM remains controversial. Complete surgical excision with or without corticosteroids has been suggested in the literature. In some cases, the disease recurs in more than half of patients when limited excision is performed [3,7,8]. Although IGLM is a benign disease, repeated surgical interventions lead to poor cosmetic results.
The main purpose of this study is to present the clinicopathological features of patients with IGLM as well as the authors' experience with medical and surgical treatment of these patients.
We reviewed hospital records of 19 cases of IGLM histopathologically diagnosed between January 2005 and December 2010. Their clinical presentation, personal and family history were recorded, as were findings from physical examination of the breast. An ultrasound was carried out on all patients. A mammogram was obtained from patients older than 35 years. An magnetic resonance imaging (MRI) was used in three cases. Pathological diagnosis was established after fine needle aspiration cytology (FNAC), core biopsy or incisional biopsy. Incisional biopsies from the abscess wall were performed on three patients who presented with abscess drainage. All aspirates and tissue samples were stained with the Papanicolaou staining procedure (PAP) as well as special stains for tuberculosis and fungal infection. No micro-organisms were found via microbiologic testing of aspirate and/or tissue samples. In all cases, stains for acid-fast bacilli and fungus were negative in sections of cell blocks and tissue.
The initial prescription given to patients was oral methylprednisolone 0.8 mg/kg/day in the first week. The medical treatment was completed in 8 weeks, reducing the weekly corticosteroid dose by 0.1 mg/kg. At the end of the eighth week, patients were clinically and radiologically evaluated for regression of breast and skin lesions. For all patients, local excision was performed for remnant lesions in the 2 weeks following the evaluation of medical treatment results.
The mean age of patients is 34.1 years (range, 27-59 years). Most of the patients (14/19) are at a reproductive age. All patients have children. Eight patients (42%) have a history of oral contraceptive use. Fifteen (79%) patients have a history of lactation, and four were lactating in the last 6 months. None of the patients have a family history of breast cancer. The left breast is seen to be affected in 10 patients. Upon admission, the most common symptom, occurring in 15 patients, is a palpable mass of 2.5 to 9 cm (Table 1). Three patients present with ulcerative skin lesions (Figure 1).
Ultrasonography of the breast establishes a hipoechoic lobulated, irregular tubular or oval shaped mass in 13 patients (Table 2). Mammographic examination of the breast is performed in 13 patients. The major radiographic finding is an ill defined mass, occurring in six patients (Figure 2). Mammography detects enlarged axillary lymph nodes in five patients. Three patients are subjected to an MRI, which shows a heterogeneous mass with an irregular border in two, and a parenchymal distortion in the other (Figure 3).
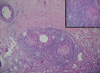
For three patients, a histopathological evaluation is performed with incisional biopsy from the abscess wall during the surgical drainage. An FNAC or core biopsy is performed for the remaining 16 patients. The FNA material is seen to contain chronic inflammation of the plasma cells, neutrophilic infiltration, non-caseating granulomas, and multinuclear giant cells (Figure 4). The major pathological changes in histological sections are found to be a granulomatous inflammatory reaction centered on the lobules. Granulomas composed of epitheloid histiocytes, langhans giant cells accompanied by lymphocytes, and plasma cells are generally found within and around dilated lobules (Figure 5).
Despite highly significant regression of inflammatory changes, none of the patients display a complete clinical response to steroid treatment (Figure 6). After steroid treatment, local excisions of the remaining lesions are performed with good cosmetic results in all patients (Figure 7). The median follow-up period is 20 months (range, 6-75 months). During the follow-up period, recurrence was observed in one patient. Recurrent lesions were treated with surgical re-excision.
IGLM is a rare chronic non-specific inflammatory lesion of the breast that can clinically mimic breast cancer. Originally described by Kessler and Wolloch in 1972, it is characterized by the presence of epitheloid and multinucleated giant cell granulomas limited to the mammary lobules with micro-abscesses in the absence of obvious etiology [9]. Local or systemic irritants as well as undetected infective causes may result in damage to the ductal epithelium. Luminal fat and protein rich secretion into the lobular connective tissue produces a localized granulomatous response [2,5]. This association has recently been challenged, because serologic and bacterial tests are usually negative in patients presenting with IGLM.
Based on our findings, it can be deduced that a recent history of pregnancy, lactation, and use of oral contraceptive play are factors that play an important role in the etiology of IGLM. Other authors have also suggested that the prior use of oral contraceptive, a history of breast feeding, and pregnancy are linked to IGLM. High levels of serum prolactin as well as distention of the acini and ducts may result in a rupture of these structures, inducing a granulomatous response [8-10]. Therefore, this history should be carefully evaluated in young women with a painful breast mass, and IGLM must be taken into account in when performing a diagnosis. In the present study, the mean age of the patients is 34.1 years (range, 27-59 years). Parous and young women are the most likely to contract IGLM. Despite the fact that the youngest patient reported in the literature is eleven years old, age at presentation is generally between 20 and 50 years [6-9]. In general, IGLM can be considered a disease of women at a reproductive age.
The most common clinical sign in patients at first admission is found to be a unilateral painful breast mass. Similarly, the most common presentation in previous studies was also a breast mass and pain [2-6]. This symptom of a breast mass easily mimics a malignant mass, which has a dramatic effect on differential diagnosis. Skin lesions and enlarged axillary lymph nodes are other suspicious signs of malignancy identified in this paper. In other recent papers on IGLM, authors have reported the presence of inflammation, swelling of the breast skin, and axillary lymphadenopathy as well as skin ulceration and fistula [2-6].
Ultrasound and mammography identify an irregular and ill defined mass in the majority of patients. The information, obtained from imaging techniques, is non-specific when it comes to diagnosis of IGLM. For this reason, the role of radiological imaging is limited in differentiating IGLM from other inflammatory and malignant conditions. Ultrasound findings are variable. Memis et al. [11] report that frequent sonographic features of IGLM are irregular hypoechoic mass lesions and tubular hypoechoic areas connecting to the mass. In other works, parenchymal heterogeneity and areas of mixed echo pattern with parenchymal deformity have been described in addition to the irregular hypoechoic mass lesion [4,7]. In the present work, ultrasound images of lobulated and tubular masses with parenchymal distortion are not disease specific. These images can lead to a misdiagnosis of malignant changes. However, ultrasound images of multiple abscess collections in addition to structural changes and a breast mass may indicate the presence of an inflammatory granulomatous process.
An ill defined mass with asymmetric diffuse density and skin thickening are the most common mammographic findings [4,11]. For patients in this study, an irregular mass and asymmetric density is non-specific mammographic findings, as they could be symptoms of various breast diseases. As well as these lesions, enlarged axillary lymph nodes, which are detected in five patients in this study, give the impression of a regional spread of breast malignancy. MRI is used for three patients but does not provide critical information for correct diagnosis. Other studies have also used MRI and found that it does not provide additional information for the differentiation of mastitis from carcinoma [4,6]. This process has high sensitivity, but low specificity for most breast lesions.
In this study, we found that clinical and radiological findings are insufficient for diagnosis of IGLM as they are not disease specific. Lesions identified clinically and radiologically could easily be misdiagnosed as carcinoma. Therefore, histopathological evaluation plays a very important role in differentiating these lesions from other granulomatous conditions, inflammatory changes, and carcinoma. Diagnosis of IGLM is established through the use of FNAC in the majority of patients in this study, while core and incisional biopsy is used to the rest. This result is confirmed by examination of removed tissue at the end of the medical treatment. A definitive diagnosis of IGLM can be made by FNAC, core biopsy or incisional and excisional biopsy [2,5,12]. The histopathological features of IGLM are non-caseating granuloma, composed of epitheloid histiocytes with giant cells within and around the lobules.
There is still no accepted management strategy for IGLM. Oral corticosteroids and surgery have both been used as treatment options. Limited excision alone has little benefit as there is a strong tendency of recurrence. However, initial excision of breast tissue ensures negative margins for inflammatory granulamatous tissue, but may have unfavorable cosmetic results. Oral corticosteroids have most often been used in recurrent cases in previous studies [7-10,13]. Initial medical treatment in the present study also takes the form of oral steroids. Proper treatment is evident by the regression of skin lesions and parenchymal enduration in nearly all patients at the end of the eighth week. In order to decrease the rate of relapse, surgical excision of the remaining lesions is carried out in the 2 weeks following the end of medical treatment. The initial use of a course of oral steroids provides important regression of breast mass and skin lesions, allowing more limited surgery. This may prevent repetitive deforming operations and recurrences. The recurrence rate has been reported as 16-50% in the literature [3,7]. In our follow-up period, IGLM is seen to recur in only one patient, on the sixth month, resulting in a need for re-excision.
IGLM is a chronic inflammatory breast disease found in young women of reproductive age. The use of hormonal treatments in the patient's past is found to play a role in the etiology of inflammatory change. A painful, irregular mass is a common physical finding. This irregular breast mass mimics carcinoma. When faced with this clinical picture, the most important step of diagnosis is to remember the possibility of IGLM as a cause. Awareness of IGLM in young women with painful breast mass leads to a more accurate diagnosis by medical practitioners. Radiological examinations do not result in specific findings able to differentiate this inflammatory condition from invasive carcinoma. However, imaging of multiple micro-abscess collections via ultrasound can reveal the presence of an inflammatory process. Cytological or histological examination establishes the correct diagnosis. Medical treatment with corticosteroids provides significant regression of the inflammatory disease, allowing more conservative surgery. Consecutive surgical excision of the remaining lesions provides definitive treatment and reduces the risk of recurrence. Thanks to regression of the inflammatory lesions through the use of oral corticosteroids and the evaluation of the conservative approach, good cosmetic results and low recurrence rates can be achieved for IGLM patients.
Figures and Tables
 | Figure 1Skin lesions of a patient with idiopathic granulomatous lobular mastitis. Clinical presentation may mimic locally advanced breast carcinoma. |
 | Figure 4Fine needle aspiration cytology finding. It shows a huge granuloma formation, with chronic inflammatory cells in the background (PAP, ×100 [Inlet magnification is ×200]). |
References
1. Dixon JM, Bundred NJ. Harris JR, Lippman EM, Morrow M, Osborne CK, editors. Management of disorders of the ductal system and infections. Disease of the Breast. 2010. 4th ed. Philadelphia: Lippincott Williams & Wilkins;42–52.
2. Al-Khaffaf B, Knox F, Bundred NJ. Idiopathic granulomatous mastitis: a 25-year experience. J Am Coll Surg. 2008. 206:269–273.

3. Bani-Hani KE, Yaghan RJ, Matalka II, Shatnawi NJ. Idiopathic granulomatous mastitis: time to avoid unnecessary mastectomies. Breast J. 2004. 10:318–322.

4. Lee JH, Oh KK, Kim EK, Kwack KS, Jung WH, Lee HK. Radiologic and clinical features of idiopathic granulomatous lobular mastitis mimicking advanced breast cancer. Yonsei Med J. 2006. 47:78–84.

5. Ocal K, Dag A, Turkmenoglu O, Kara T, Seyit H, Konca K. Granulomatous mastitis: clinical, pathological features, and management. Breast J. 2010. 16:176–182.

6. Asoglu O, Ozmen V, Karanlik H, Tunaci M, Cabioglu N, Igci A, et al. Feasibility of surgical management in patients with granulomatous mastitis. Breast J. 2005. 11:108–114.

7. Kok KY, Telisinghe PU. Granulomatous mastitis: presentation, treatment and outcome in 43 patients. Surgeon. 2010. 8:197–201.

8. Erozgen F, Ersoy YE, Akaydin M, Memmi N, Celik AS, Celebi F, et al. Corticosteroid treatment and timing of surgery in idiopathic granulomatous mastitis confusing with breast carcinoma. Breast Cancer Res Treat. 2010. 123:447–452.

9. Tuli R, O'Hara BJ, Hines J, Rosenberg AL. Idiopathic granulomatous mastitis masquerading as carcinoma of the breast: a case report and review of the literature. Int Semin Surg Oncol. 2007. 4:21.

10. Bakaris S, Yuksel M, Ciragil P, Guven MA, Ezberci F, Bulbuloglu E. Granulomatous mastitis including breast tuberculosis and idiopathic lobular granulomatous mastitis. Can J Surg. 2006. 49:427–430.
11. Memis A, Bilgen I, Ustun EE, Ozdemir N, Erhan Y, Kapkac M. Granulomatous mastitis: imaging findings with histopathologic correlation. Clin Radiol. 2002. 57:1001–1006.

12. Gupta RK. Fine needle aspiration cytology of granulomatous mastitis: a study of 18 cases. Acta Cytol. 2010. 54:138–141.




 PDF
PDF ePub
ePub Citation
Citation Print
Print








 XML Download
XML Download