Abstract
Purpose
Introducing the relationship between the surgical instruments used in modified radical mastectomy and wound complications is important for preventing and decreasing complications. This prospective randomized trial was designed to assess the impact of scalpel, electrocautery, and ultrasonic dissector usage on wound complications and tissue damage.
Methods
Eighty-two consecutive patients operated with mastectomy were studied. The postoperative time period needed for hemovac drainage, the amount and duration of seroma, infection, flap ecchymosis and necrosis rates were compared. Tumor necrosis factor alpha (TNF-α) and interleukin-6 (IL-6) levels in drainage fluids were determined to confirm the inflammatory response and tissue damage.
Results
The numbers of patients included in the scalpel, electrocautery and ultrasonic dissector groups were 27, 26, and 29, respectively. The groups were homogenous with respect to age, body mass index, stage, cormorbidities, breast volume and flap area. Operation time and the amount of bleeding were statistically higher in the scalpel group. The incidence of seroma was higher in the electrocautery group and arm mobilization had to be delayed in this group. There were no differences between groups with respect to hematoma, infection, ecchymosis, necrosis, hemovac drainage and the total and first 3 days of seroma volume. TNF-α and IL-6 levels were significantly higher in samples obtained from the drains of patients operated with electrocautery.
Conclusion
Ultrasonic dissector decreases operation time by decreasing the amount of bleeding without increasing the seroma incidence. High cytokine levels in drainage fluids from patients operated with elecrocautery indicates that electrocautery induces more tissue damage and acute inflammatory response. Therefore, seroma, due to acute inflammatory response, was seen more frequently in the electrocautery group. Ultrasonic dissector coagulates protein by breaking hydrogen bonds which may close vascular and lymphatic channels more precisely. But, its actual preventive effect on seroma formation might be related to diminished inflammatory response.
Although breast conserving and oncoplastic techniques are being used with increasing frequency, modified radical mastectomy (MRM) is still an important alternative for the surgical treatment of breast cancer. The most frequent complications seen during the wound healing process of MRM are seroma, surgical site infections (SSI), flap necrosis, and hematoma. These complications may give rise to more serious complications such as wound dehiscence and delay adjuvant treatments by prolonging wound healing process. The surgical instruments used in making skin flaps and dissecting breast tissue with underlying pectoral fascia are related to these complications. Introducing the relationship between surgical instruments used in surgery and wound complications might be one of the basic steps for preventing and decreasing the number of complications. Besides the scalpel, electrocautery has also been used in MRM to decrease bleeding. In recent years, ultrasonic dissector has also been used, which is thought to cause less tissue damage.
The levels of proinflammatory cytokines in wounds or wound fluids can be used as a reliable parameter reflecting tissue damage [1,2]. The biochemical analysis of the seroma fluid after MRM has shown that this fluid is exudate containing immunoglobulins, leukocytes, granulocytes and lymphocytes [3]. In other words, seroma fluid is a suitable material for examining proinflammatory cytokines. This prospective randomized trial was planned to assess the impact of surgical instruments (scalpel, electrocautery, and ultrasonic dissector) used in MRM on wound complications and tissue damage.
Eighty-two consecutive patients, surgically treated with MRM between January 2009 and May 2010 were enrolled in our prospective study. The numbers of patients included in the scalpel, electrocautery, and ultrasonic dissector groups were 27, 26, and 29, respectively (Figure 1). After obtaining informed consent, scalpel, electrocautery (Olympus EUS 10; Kyoritsu Electric Co., Shizuoka, Japan) or harmonic scalpel (Ultrasicion® Harmonic Scalpel, Generator 300; Ethicon Endosurgery, Cincinnati, USA) were used individually on each patient to create skin flaps and excise breast tissue with underlying pectoralis fascia. Randomization was arranged sequentially. The postoperative time period needed for vacuum drainage, the amount and duration of seroma, surgical site infection, hematoma, flap ecchymosis and necrosis rates were compared. Patient age, body mass index (BMI), smoking history, breast volume, disease stage, the number of total and metastatic lymph nodes, comorbidities, biopsy type, biochemical tests that may alter wound healing, flap areas, the duration of surgery, and hemorrhage occurring during surgery (measured by sponge numbers and weight) were recorded.
A seroma sample (20 mL) during the first 24 hours of drainage was taken for analysis. The samples were centrifuged at 2,000 rpm for 10 minutes and then stored at -20℃. The levels of tumor necrosis factor alpha (TNF-α) and interleukin-6 (IL-6) were determined. Patients with locally advanced breast cancer who were undergoing neoadjuvant chemotherapy, and the patients who had undergone breast preserving surgery or simple mastectomy were excluded.
After a skin incision was made with a scalpel, the skin flaps were lifted up with the help of hooks. In cases in which the skin flaps were prepared by using harmonic scalpel, sharp and curved tips were used on level five during dissection and on level three during hemostasis. All vessels larger than 3 mm in diameter were sealed with ultrasonic dissector. After flap preparation, the ultrasonic dissector was also used for pectoralis fascia and breast tissue removal. Ultrasonic dissector was also used for interpectoral dissection and cutting the head of the pectoralis minor muscle.
Axillary dissection of all patients was performed with scalpel in all patients. Electrocautery was used in coagulation mode within 20 to 30 volt range. The thoracodorsal pedicle and thoracicus longus nerves were preserved. Standard level 2 dissection was carried out in all patients. However, level-three dissection was also performed in patients with macroscopic involvement during surgery. Closed suction drains were used for all patients after hemostasis. Subcutaneous tissue was approximated with absorbable sutures and the skin was closed with subcuticular continuous sutures. Daily drainage volume was recorded and the drains were not removed untill the daily drainage decreased to less than 50 mL. All drains requiring more than 7 days were removed irrespective of daily drainage amount and the patients were instructed to attend arm physiotherapy.
Prophylactic antibiotics were not used in any of the patients. Fluids collected under the skin flaps and axilla that presented clinical findings were accepted as seroma. The presence of erythema, purulent drainage, localized heat increase, cellulitis, pain, redness, sensitivity and related wound dehiscence was regarded as SSI irrespective of the presence of wound culture. While the hemorrhagic drainage at the incision or drains for more than two days were accepted as hemorrhage, the collections made in operation fields with skin colour changes and mass effect were accepted as hematoma.
Samples were collected from drain fluid within 24 hour postoperatively. TNF-α and IL-6 were measured in wound fluid by quantitative ELISA analysis using human TNF-α (hTNF-α) and IL-6 (hIL-6) kits (Biosource International Inc., Camarillo, USA). Monoclonal antibodies specific for hTNF-α and hIL-6 had been coated onto the wells of the microtiter strips provided. Samples, including standards with known hTNF-α content, control specimens and unknowns were pipetted into wells. During the first incubation, antigens bind to the immobilized (capture) antibody on one site. After washing, biotinylated monoclonal antibodies are added. During the second incubation, antibodies bind to the immobilized hTNF-α and hIL-6 captured during the first incubation. Streptavidin peroxidase is added after removing the excess second antibody. This enzyme binds to the biotinylated antibody to complete the four-member sandwich. After a third incubation and washing to remove all of the unbound enzyme, a substrate solution is added, which is acted upon by the bound enzyme to produce color. The intensity of this colored product is directly proportional to the concentrations of hTNF-α and hIL-6 present in the original specimen.
All numerical data are expressed as mean±SEM. The adverse outcomes in the groups were compared by using the chi-square test. Mann-Whitney U-test, computed with SPSS software program (version 10.0; SPSS Inc., Chicago, USA), was used to evaluate the mean values of continuous variables to assess the statistical significance of inter-group differences. A p<0.05 was considered as statistically significant.
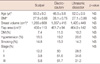
The numbers of patients included in scalpel, electrocautery and ultrasonic dissector groups were 27, 26, and 29, respectively. The groups were homogenous with respect to age, BMI, stage, comorbidities, smoking, biopsy type, breast volume and flap areas (Table 1). In comparison with other groups, operation time and bleeding were significantly higher in the scalpel group than the other groups. Seroma incidence was higher in the electrocautery group than the other groups, and arm physiotherapy had to be delayed for this group. There was no difference between groups with respect to hematoma, SSI, ecchymosis, days needed for vacuum drain removal, the amount of seroma on the first postoperative day or total drainage levels (Table 2).
Mean TNF-α levels in scalpel, electrocautery, and ultrasonic dissector groups were 283±144, 600±382, and 307±140 pg/mL, respectively. Mean IL-6 levels in scalpel, electrocautery and ultrasonic dissector groups were 1,416±214, 2,484±441, and 1,664±310 pg/mL, respectively. TNF-α and IL-6 levels in electrocautery group were significantly higher (Table 3).
Seroma is the most frequent wound complication of MRM and the incidence varies between 30 and 40% [4]. At the beginning, lymphatic channels opened during dissection were blamed to cause seroma formation whereas later on the dead space, the irregular anatomy of the chest wall and flap dislodgement related to arm movements were considered as factors causing seroma formation [5]. In their studies about the pathophysiology of seroma, Watt-Boolsen et al. [6] concluded that seroma is an exudate related to the acute inflammatory response phase of wound healing. Wu et al. [7] also described increased level of vascular endothelial growth factor and decreased level of endostatin as an angiogenesis inhibitor and they suggested that seroma resulted from a physiological angiogenesis cascade of trauma. After the discovery that the decreased excudative phase of wound healing decreases the incidence for seromas, attention has been drawn to the surgical instruments used for a mastectomy.
Electrocautery is used during mastectomy for its ability to decrease bleeding and also been to increase the seroma incidence compared with scalpel. Beside this, other wound complications such as cellulitis, infection, and necrosis have been suggested to increase with electrocautery [8,9]. It has been shown that skin flaps created by scalpel have better tension strength, contain more fibroblasts and collagen and fewer leukocytes and have less wound drainage compared to skin flaps created by electrocautery [10].
The following reasons may be the probable causes for adverse effects of electrocautery on wound healing. Electrocautery uses direct thermal energy that can diffuse into deeper tissues. Although high thermal energy leaves huge amount of devitalized tissues, it also causes lysis of subcutaneous tissues. Thus, the protective effect of subcutaneous tissue disappears. It has also been shown that electrocautery results in thrombosis of subdermal vasculature [8]. However, it has yet to be validated whether electrocautery causes more tissue damage and acute inflammatory response.
Ultrasonic dissector instrument is made up of a disposable cutting device and a generator. Electrical energy generated is converted into mechanical energy by "piezoelectric crystal system." A resonance at 55,000 Hz is produced at the hand unit. This energy is conducted to the tissues as ultrasonic waves and presents as cavitation, coagulation and cutting abilities. This energy penetrates the tissues to a depth of 25-100 µm at five levels.
Most studies on cutting devices used during mastectomies are retrospective and non-randomized. In these studies, ultrasonic dissector has generally been compared to cold scalpel. Although the superiority of ultrasonic dissector to scalpel with respect to wound complications has not be demonstrated, it is obvious that the ultrasonic dissector shortens the operation time by decreasing intraoperative bleeding [11,12]. In a study of 23 patients, Deo et al. [13] compared ultrasonic dissector with electrocautery and there was no difference was observed between the groups with respect to operation time and incidence of seroma. Blood loss and amount of drainage were significantly lower in the ultrasonic dissector group than the electrocautery group. The time needed for drain removal was also shorter in the ultrasonic dissector group.
Adwani and Ebbs [14] employed a pilot study to determine whether ultracision reduces intraoperative blood loss complications and seroma formation. Their findings suggest that acute blood loss was significantly reduced in the harmonic scalpel group compared to the control group. Yet, they detected little difference between the two groups in terms of hospital stay, volume or duration of postoperative drainage or subsequent aspiration of seroma.
Ultrasound scissors have recently been more frequently used as an alternative surgical tool for dissection and haemostasis. Sanguinetti et al. [15] studied the utility and advantages of this instrument compared with electrocautery to perform axillary dissection and found no significant difference in the operating time between the ultrasound scissors and electrocautery group. In contrast, they found that there were significant differences in terms of blood loss, drainage volume, the number of drainage days and seroma rate.
Proinflammatory cytokines play a role in many biological processes such as inflammation, sepsis and wound healing. IL-6 and TNF-α play a key role in the cross-talk between cytokines and they are the most readily measurable ones [16,17]. Cytokines in wound healing process play an important role in initiating, controlling, and terminating of cellular events such as angiogenesis and extracellular matrix formation [18,19]. TNF-α in surgical wound is secreted into the surgical field with the first stimulation of extravasated and activated monocytes and macrophages. Their rise in blood is limited and slow. The minimum level detectable in the blood is 2 pg/mL. IL-6 is secreted from activated monocytes and macrophages and the secretion period and half-life is longer than TNF-α. The minimum detectable level in the blood is 1 pg/mL and its detection in the blood is relatively easier than TNF-α [20]. Although TNF-α levels begin to increase earlier than those of IL-6, both cytokines reach their maximum levels within 24 hours [21]. In the light of these findings, it can be said that IL-6 and TNF-α levels in seroma fluid detected at 24 hour reflect the severity of tissue damage authentically. Besides, as the mastectomy does not have a direct adverse effect on organ functions like liver or kidneys, the inflammation created might be directly attributable to the surgery.
The amounts of cytokines secreted are also being associated with the duration of surgery. It has been postulated that longer operations are associated with higher cytokine levels [22]. It was also shown by Reith et al. [23] and Kristiansson et al. [24] that laparoscopic cholecystectomies with less tissue trauma and shorter duration of surgery induce less cytokine release than open surgery. The high cytokine levels with shorter duration of surgery in electrocautery group of patients makes the accusation about the surgical instrument easier.
In summary, the scalpel increased bleeding and duration of surgery compared with the other two cutting devices. Although the bleeding and duration of surgery was lower in the electrocautery group, the seroma incidence was found to be higher and the start of arm physiotherapy was delayed. Ultrasonic dissector was found to decrease the duration of surgery by diminishing the bleeding without increasing the seroma incidence. High cytokine levels detected in seroma fluids of the patients in the electrocautery group were an indicator of greater issue damage and inflammatory response. Therefore, it can be argued that seroma as a result of acute inflammatory response was observed at higher frequencies in the electrocautery group. Ultrasonic dissector might be influential for closing the small vascular and lymphatic vessels created by hydrogen bond degradation. Moreover, the seroma preventive effect might be related to its ability to induce less of an acute inflammatory response. Perhaps both of these mechanisms work together. Ultrasonic dissector was as efficient as electrocautery in terms of hemostasis and decreasing the operation time yet it is as harmless as scissor in terms of seroma formation. In short, ultrasonic dissector was advantageous compared to the other two devices.
Figures and Tables
 | Figure 1Outline of study design followed by Consolidated Standards of Reporting Trials (CONSORT) statement. |
References
1. Henry G, Garner WL. Inflammatory mediators in wound healing. Surg Clin North Am. 2003. 83:483–507.

2. Grellner W, Georg T, Wilske J. Quantitative analysis of proinflammatory cytokines (IL-1beta, IL-6, TNF-alpha) in human skin wounds. Forensic Sci Int. 2000. 113:251–264.

3. Shamley DR, Barker K, Simonite V, Beardshaw A. Delayed versus immediate exercises following surgery for breast cancer: a systematic review. Breast Cancer Res Treat. 2005. 90:263–271.

4. Coveney EC, O'Dwyer PJ, Geraghty JG, O'Higgins NJ. Effect of closing dead space on seroma formation after mastectomy-a prospective randomized clinical trial. Eur J Surg Oncol. 1993. 19:143–146.
5. Kuroi K, Shimozuma K, Taguchi T, Imai H, Yamashiro H, Ohsumi S, et al. Pathophysiology of seroma in breast cancer. Breast Cancer. 2005. 12:288–293.

6. Watt-Boolsen S, Nielsen VB, Jensen J, Bak S. Postmastectomy seroma. A study of the nature and origin of seroma after mastectomy. Dan Med Bull. 1989. 36:487–489.
7. Wu FP, Hoekman K, Meijer S, Cuesta MA. VEGF and endostatin levels in wound fluid and plasma after breast surgery. Angiogenesis. 2003. 6:255–257.

8. Hoefer RA Jr, DuBois JJ, Ostrow LB, Silver LF. Wound complications following modified radical mastectomy: an analysis of perioperative factors. J Am Osteopath Assoc. 1990. 90:47–53.

9. Miller E, Paull DE, Morrissey K, Cortese A, Nowak E. Scalpel versus electrocautery in modified radical mastectomy. Am Surg. 1988. 54:284–286.
10. Gelman CL, Barroso EG, Britton CT, Haklin MF, Staren ED. The effect of lasers, electrocautery, and sharp dissection on cutaneous flaps. Plast Reconstr Surg. 1994. 94:829–833.

11. Lumachi F, Brandes AA, Burelli P, Basso SM, Iacobone M, Ermani M. Seroma prevention following axillary dissection in patients with breast cancer by using ultrasound scissors: a prospective clinical study. Eur J Surg Oncol. 2004. 30:526–530.

12. Galatius H, Okholm M, Hoffmann J. Mastectomy using ultrasonic dissection: effect on seroma formation. Breast. 2003. 12:338–341.

13. Deo SV, Shukla NK, Asthana S, Niranjan B, Srinivas G. A comparative study of modified radical mastectomy using harmonic scalpel and electrocautery. Singapore Med J. 2002. 43:226–228.
14. Adwani A, Ebbs SR. Ultracision reduces acute blood loss but not seroma formation after mastectomy and axillary dissection: a pilot study. Int J Clin Pract. 2006. 60:562–564.

15. Sanguinetti A, Docimo G, Ragusa M, Calzolari F, D'Ajello F, Ruggiero R, et al. Ultrasound scissors versus electrocautery in axillary dissection: our experience. G Chir. 2010. 31:151–153.
16. Bennett NT, Schultz GS. Growth factors and wound healing: biochemical properties of growth factors and their receptors. Am J Surg. 1993. 165:728–737.

17. Gailit J, Clark RA. Wound repair in the context of extracellular matrix. Curr Opin Cell Biol. 1994. 6:717–725.

18. Lin E, Calvano SE, Lowry SF. Inflammatory cytokines and cell response in surgery. Surgery. 2000. 127:117–126.

19. Gallucci RM, Simeonova PP, Matheson JM, Kommineni C, Guriel JL, Sugawara T, et al. Impaired cutaneous wound healing in interleukin-6-deficient and immunosuppressed mice. FASEB J. 2000. 14:2525–2531.

20. Schmidt A, Bengtsson A, Tylman M, Blomqvist L. Pro-inflammatory cytokines in elective flap surgery. J Surg Res. 2007. 137:117–121.

21. Loo WT, Sasano H, Chow LW. Pro-inflammatory cytokine, matrix metalloproteinases and TIMP-1 are involved in wound healing after mastectomy in invasive breast cancer patients. Biomed Pharmacother. 2007. 61:548–552.

22. Reber PU, Andren-Sandberg A, Schmied B, Büchler MW. Cytokines in surgical trauma: cholecystectomy as an example. Dig Surg. 1998. 15:92–101.

23. Reith HB, Kaman S, Mittelkötter O, Kilic Y, Kozuschek W. Cytokine activation in patients undergoing open or laparoscopic cholecystectomy. Int Surg. 1997. 82:389–393.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download