Abstract
Purpose
Mucinous carcinoma (MC) of the breast is a rare histologic type of mammary neoplasm. The objective of this study was to evaluate the long-term disease-free survival (DFS) and overall survival (OS) of MC.
Methods
We conducted a retrospective analysis of all MC cases reported to a database between 1994 and 2010. Clinicopathological characteristics and survival of 268 MC cases were reviewed and compared with 2,455 invasive ductal carcinoma-not otherwise specified (IDC-NOS) cases.
Results
The MC cases were of a younger age, involved less lymph nodes, lower stage, more expression of hormonal receptors, and less HER2 overexpression compared to the IDC-NOS cases. The 5-year DFS rate for MC was 95.2% compared to 92.0% for IDC-NOS. The 5-year OS rate for MC was 98.9% compared to 94.9% for IDC-NOS. Multivariate analysis using Cox regression revealed that the mucinous type was a significant prognostic factor for DFS with lower nodal status (N stage) and hormonal therapy. For OS, only N stage was the most significant prognostic factor followed by adjuvant chemotherapy and adjuvant hormonal therapy.
Mucinous carcinoma (MC) of the breast is a rare histological type that is characterized by a large amount of mucin production. MC of the breast is defined as having a mucinous component of 50% or more [1-3]. The incidence of MC was reported to be 1-6% of all primary breast cancers [1-8]. MC usually occurs in elderly and the median age at diagnosis is older than 55-60 years [1,4-6,9-11].
The subgroups of MC, pure-type and mixed-type MC, are classified upon the quantification of cellularity [12,13]. The "pure" type consists exclusively of tumor tissue with extracellular mucin production, while the "mixed" type is defined by the World Health Organization (WHO) as a tumor where 50-90% of the area is mucinous and also admixing with infiltrating ductal epithelial component [14].
Fujii et al. [15] investigated the genomic features of pure-type MC and found that it does not have the extensive genomic alterations typically found in more common variants of breast cancer. Moreover, MC exhibited less genetic instability than other forms of breast cancer and its molecular pathogenesis appeared substantially different from that of the usual breast carcinoma. Recently, a study by Lacroix-Triki et al. [3] supported these findings and found that MCs were not only a histological pattern, but also a molecular entity, distinct from invasive ductal carcinoma-not otherwise specified (IDC-NOS).
Nevertheless, because of relative rarity of MC patients, the prognostic significance of clinicopathological characteristics is not well established and most reported MC series have a low number of patients and a limited long-term follow-up. Since the incidence of breast cancer is significantly increasing in Korea [16,17], the objective of this study was to evaluate the long term disease-free survival (DFS) and overall survival (OS) as well as the significance of the available clinical and pathological prognostic factors with the goal of using this information to develop an adequate treatment guideline.
Patients were selected from the database of the Breast Cancer Center at Samsung Medical Center, Korea between 1994 and 2010. Of these patients, 268 had been diagnosed with MC. These patients were compared to 2,455 patients diagnosed with IDC-NOS who were treated during the same period.
Pure-type MC was defined as having a mucinous component of more than 90%, using specialized pathologists with extensive experience in breast pathology performing a pathologic slide review. Among 268 patients, 215 (80.2%) were pure MC and 53 patients (19.8%) were mixed mucinous-ductal carcinoma.
We reviewed clinicopathologic factors, immunohistochemistries of biologic factors such as estrogen receptor (ER), progesterone receptor (PR), human epidermal growth factor receptor 2 (HER2), and treatment modalities (type of operation, use of chemotherapy, radiation therapy, and hormone therapy). The pathologic tumor stage was assessed according to the 6th American Joint Committee on Cancer (AJCC) Staging System [18]. The histological grade was determined according to the Bloom-Richardson classification. The Allred score was used to measure ER or PR positivity, and HER2 was scored as 0-3. Patients with an immunohistochemistry (IHC) score of 2+ or gene amplification determined by fluorescence in situ hybridization (FISH) were considered positive. Time to follow-up is the interval between the date of operation and the date of the most recently identified patient contact or database update.
Student's t-tests or Fisher's exact tests were used to compare the clinicopathological characteristics of the MC and IDC groups. The Kaplan-Meier method and Cox regression analysis were used to determine DFS rates and OS rates. Statistical analyses were performed using PASW Statistics 18 (International Business Machines Co., New York, USA).
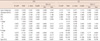
Clinicopathological characteristics and treatment patterns of all patients are shown in Table 1. Median age at diagnosis was 44 years for MC patients (range, 22-87 years), and the age at diagnosis was much younger in MC patients than in IDC-NOS patients (median age, 47 years; range, 21-84; p<0.001). Tumor size (T stage) was not significantly different from IDC-NOS. Of the MC patients, 217 (81.0%) had no axillary lymph node involvement and MC patients had a lower N stage than IDC-NOS patients (p<0.001). Expressions of ER or PR were higher in MC (96.0%) than in IDC-NOS (67.7%), and these differences were significant (p<0.001). Of the 202 patients whose HER2/neu status was available, only 11 (5.4%) showed HER2/neu overexpression. MC patients showed a more favorable histologic grade than IDC-NOS patients (p<0.001). Less chemotherapy and more hormone therapy were applied to MC patients, probably because of the favorable features associated with higher ER or PR expression and lower histologic grade in MC. However, the rates of radiation therapy were not significantly different between MC and IDC-NOS patients.
Clinicopathological characteristics and treatment patterns of pure-type MC were similar to those with mixed-type MC except for N stage (Table 2). No significant difference in age at diagnosis was observed between the pure-type MC and mixed-type MC (44 vs. 46 years, p=0.368). Pure-type MC was smaller in size (median, 2.0 cm; mean, 2.3 cm) than the mixed type (median, 2.5 cm; mean, 2.9 cm; p=0.033), although there were no significant differences in T stage. Pure-type MC also had a more differentiated histologic grade (p<0.001) and lower lymph node metastases than mixed-type MC (10.7% vs. 52.8%, p<0.001).
The median follow-up duration was 49.7 months for all patients (range, 0-181 months). For MC patients, the 5-year DFS rate was 95.2% and in IDC-NOS patients it was 92.0% (Figure 1). The 5-year OS rates of MC patients was 98.9% and IDC-NOS patients was 94.9% (Figure 2). The DFS and OS rates were not significantly different between MC and IDC-NOS (p=0.072 and p=0.061, respectively). Although a significant difference in DFS for MC was not observed in the univariate analysis by the Kaplan-Meier method, multivariate analysis by Cox regression revealed that mucinous type was a significant prognostic factor for DFS with lower N stage and hormonal therapy (Table 3). According to multivariate analysis for OS, nodal status (N stage) was the most significant prognostic factor, followed by adjuvant chemotherapy and adjuvant hormonal therapy. The mucinous type itself was not associated with an improvement in overall survival (Table 3).
The 5-year DFS rates were 96.1% for pure-type MC and 87.5% for mixed-type MC (Figure 1). Pure-type MC showed a better DFS than IDC-NOS (p=0.044), but was not significantly different from mixed-type MC (p=0.128). Pure-type MC had a better OS than IDC-NOS (p=0.025) and mixed-type MC (p=0.043). However, the DFS between mixed-type MC and IDC-NOS was not significantly different (p=0.848) or OS (p=0.77).
In stage-matched analysis for DFS and OS, MC showed a better survival than IDC-NOS (Figure 3), but no significant differences were observed between the group. This lack of significance was probably due to the small sample size and short follow-up duration. In T stage-matched analysis for DFS and OS, MC showed a better survival than IDC-NOS (Figure 4), but only the T2-stage MC group showed significantly better OS (p=0.028).
MC is a rare histologic type of mammary neoplasm. In the West, MC patients usually are postmenopausal women and older than IDC-NOS patients [2,5-7,10,11,19]. However, in our study, MC patients were younger than IDC-NOS patients. This is in agreement with Park's finding for Korean MC patients. Park et al. [20] suggested that breast cancer may have a younger age of onset in Korean women due to the wide use of ultrasonography, or genetic and environmental factors. In addition, a cohort effect may exist in younger generations, or the apparent increase in incidence may reflect the easy accessibility to breast cancer screening among middle-aged women, which is similar to the results reported in a Japanese study [21]. However, histological features and survival rates of MC were similar between Korean patients and Western patients.
Axillary nodal involvement in MC patients, although rare, seems to worsen the prognosis of breast cancer. A previous study found that patients with node-positive MC in the breast were significantly more likely to have recurrence and poor prognosis [2,5,7,12,22]. The incidence of axillary metastases ranged from 2% to 14% in pure MC [2,8,9,11,23,24] and 45% to 64% in mixed MC [2,12,24]. This trend was corroborated in our study (10.7% in pure MC and 52.8% in mixed MC). Because the status of the axillary lymph nodes, pure MC has a better prognosis than mixed MC [7,9,12,23,24]. Although pure-type MC has been associated with a better short-term prognosis than IDC, previous studies reported identical long-term survival curves [1,2,4,25].
Avisar et al. [9] identified certain factors that were associated with a higher incidence of axillary nodal disease in MC patients, which included younger age, aneuploidy, high nuclear grade, and a negative estrogen receptor status. In our study, patients with higher T stage and negative estrogen receptor had higher nodal metastases.
The prognostic significance of tumor size is an interesting issue in MC patients. Di Saverio et al. [1] utilized tumor size was an independent prognostic indicator, but it was less significant than nodal status and age in multivariate analysis of a large number of pure-type MC cases. Although some studies have not found any correlations between tumor size and the incidence of axillary nodal metastases [9,26], others found that the incidence of node positivity was directly related to tumor size [1,5]. Diab et al. [5] demonstrated that patients with tumor size ≤1 cm had a <5% risk of developing lymph node metastasis. In our study, MC showed significantly lower rates of nodal metastases than IDC-NOS in T1 and T2 stage (p<0.001), but no difference was observed in T3 and T4 stages. This may be explained by the survival difference with IDC-NOS, especially in stage II patients. Although no significant differences in stage II patients was observed, this OS difference in stage II patients was also seen in previous studies [2,20]. Diab et al. [5] demonstrated a significantly better DFS for MC versus IDC-NOS, even in a subset of patients with node negativity; however, we found no significant differences between the two groups in the node negative subset.
In Koreans, MC patients were in younger than IDC-NOS patients, and showed favorable characteristics including less involvement of lymph node, lower stage, more expression of hormonal receptors, and less HER2 overexpression. MC was shown to be associated with a better DFS than IDC-NOS, but it has a similar OS. Nodal status and adjuvant therapy appear to be more significant predictors of prognosis than histologic type.
Figures and Tables
 | Figure 1Comparison of disease-free survival (DFS) curves for invasive ducal carcinoma (IDC) and mucinous carcinoma. |
 | Figure 2Comparison of overall survival (OS) curves for invasive ducal carcinoma (IDC) and mucinous carcinoma. |
 | Figure 3Overall survival (OS) curves for invasive ducal carcinoma (IDC) and mucinous carcinoma, stratified by stage. |
 | Figure 4Overall survival (OS) curves for invasive ducal carcinoma (IDC) and mucinous carcinoma, stratified by tumor size (T stage). |
Table 1
Clinicopathological characteristics and treatment modalities of invasive ductal carcinoma (IDC) and mucinous carcinoma (MC)

Notes
References
1. Di Saverio S, Gutierrez J, Avisar E. A retrospective review with long term follow up of 11,400 cases of pure mucinous breast carcinoma. Breast Cancer Res Treat. 2008. 111:541–547.

2. Komaki K, Sakamoto G, Sugano H, Morimoto T, Monden Y. Mucinous carcinoma of the breast in Japan. A prognostic analysis based on morphologic features. Cancer. 1988. 61:989–996.

3. Lacroix-Triki M, Suarez PH, MacKay A, Lambros MB, Natrajan R, Savage K, et al. Mucinous carcinoma of the breast is genomically distinct from invasive ductal carcinomas of no special type. J Pathol. 2010. 222:282–298.

4. André S, Cunha F, Bernardo M, Meneses e Sousa J, Cortez F, Soares J. Mucinous carcinoma of the breast: a pathologic study of 82 cases. J Surg Oncol. 1995. 58:162–167.

5. Diab SG, Clark GM, Osborne CK, Libby A, Allred DC, Elledge RM. Tumor characteristics and clinical outcome of tubular and mucinous breast carcinomas. J Clin Oncol. 1999. 17:1442–1448.

6. Louwman MW, Vriezen M, van Beek MW, Nolthenius-Puylaert MC, van der, Roumen RM, et al. Uncommon breast tumors in perspective: incidence, treatment and survival in the Netherlands. Int J Cancer. 2007. 121:127–135.

7. Fisher ER, Gregorio RM, Fisher B, Redmond C, Vellios F, Sommers SC. The pathology of invasive breast cancer. A syllabus derived from findings of the National Surgical Adjuvant Breast Project (protocol no. 4). Cancer. 1975. 36:1–85.

8. Memis A, Ozdemir N, Parildar M, Ustun EE, Erhan Y. Mucinous (colloid) breast cancer: mammographic and US features with histologic correlation. Eur J Radiol. 2000. 35:39–43.

9. Avisar E, Khan MA, Axelrod D, Oza K. Pure mucinous carcinoma of the breast: a clinicopathologic correlation study. Ann Surg Oncol. 1998. 5:447–451.

10. Simpson JF, Page DL. Prognostic value of histopathology in the breast. Semin Oncol. 1992. 19:254–262.
11. Rosen PP, Lesser ML, Kinne DW. Breast carcinoma at the extremes of age: a comparison of patients younger than 35 years and older than 75 years. J Surg Oncol. 1985. 28:90–96.

12. Rasmussen BB, Rose C, Christensen IB. Prognostic factors in primary mucinous breast carcinoma. Am J Clin Pathol. 1987. 87:155–160.

13. Silverberg SG, Kay S, Chitale AR, Levitt SH. Colloid carcinoma of the breast. Am J Clin Pathol. 1971. 55:355–363.

14. Histological typing of breast tumors. Tumori. 1982. 68:181–198.
15. Fujii H, Anbazhagan R, Bornman DM, Garrett ES, Perlman E, Gabrielson E. Mucinous cancers have fewer genomic alterations than more common classes of breast cancer. Breast Cancer Res Treat. 2002. 76:255–260.

16. Ahn SH. Korean Breast Cancer Society. Clinical characteristics of breast cancer patients in Korea in 2000. Arch Surg. 2004. 139:27–30.

17. Ahn SH, Yoo KY. Korean Breast Cancer Society. Chronological changes of clinical characteristics in 31,115 new breast cancer patients among Koreans during 1996-2004. Breast Cancer Res Treat. 2006. 99:209–214.

18. Singletary SE, Allred C, Ashley P, Bassett LW, Berry D, Bland KI, et al. Staging system for breast cancer: revisions for the 6th edition of the AJCC Cancer Staging Manual. Surg Clin North Am. 2003. 83:803–819.

19. Lesser ML, Rosen PP, Senie RT, Duthie K, Menendez-Botet C, Schwartz MK. Estrogen and progesterone receptors in breast carcinoma: correlations with epidemiology and pathology. Cancer. 1981. 48:299–309.

20. Park S, Koo J, Kim JH, Yang WI, Park BW, Lee KS. Clinicopathological characteristics of mucinous carcinoma of the breast in Korea: comparison with invasive ductal carcinoma-not otherwise specified. J Korean Med Sci. 2010. 25:361–368.

21. Minami Y, Tsubono Y, Nishino Y, Ohuchi N, Shibuya D, Hisamichi S. The increase of female breast cancer incidence in Japan: emergence of birth cohort effect. Int J Cancer. 2004. 108:901–906.

22. Vo T, Xing Y, Meric-Bernstam F, Mirza N, Vlastos G, Symmans WF, et al. Long-term outcomes in patients with mucinous, medullary, tubular, and invasive ductal carcinomas after lumpectomy. Am J Surg. 2007. 194:527–531.

23. Norris HJ, Taylor HB. Prognosis of mucinous (gelatinous) carcinoma of the breast. Cancer. 1965. 18:879–885.

24. Fentiman IS, Millis RR, Smith P, Ellul JP, Lampejo O. Mucoid breast carcinomas: histology and prognosis. Br J Cancer. 1997. 75:1061–1065.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download