Abstract
Purpose
Our study aimed to evaluate the feasibility of adjuvant cyclophosphamide/vinorelbine/5-fluorourail (CVF) chemotherapy as an alternative to cyclophosphamide/methotrexate/5-fluorouracil (CMF) chemotherapy for treating early breast cancer.
Methods
One hundred and forty-nine patients were randomly assigned to CMF or CVF adjuvant chemotherapy for treating their early stage breast cancer between September 2000 and December 2007. The disease-free survival (DFS), the overall survival (OS), and the toxicity profiles of both groups were compared.
Results
Sixty-seven patients underwent CMF chemotherapy whereas 82 patients underwent CVF chemotherapy. The DFS and OS were 88 months (95% confidence interval [CI], 76-101 months) and 94 months (95% CI, 83-104 months), respectively for the CMF group, and 97 months (95% CI, 93-101 months), and 101 months (95% CI, 98-104 months), respectively for the CVF group. However, those survival gains of the CVF group were not statistically significant (p-value=0.069 for the DFS and 0.99 for the OS). The CVF group showed a favorable toxicity profile in terms of the grade 3/4 hematologic toxicities as compared to that of the CMF group.
Adjuvant systemic chemotherapy is the standard treatment modality to improve the survival of breast cancer patients. Breast cancer is more responsive to the systemic chemotherapy than other solid tumors are [1,2]. Cyclophosphamide, methotrexate, and 5-fluorouracil (CMF) regimen, which was introduced in the 1970s, is the most commonly used chemotherapeutic regimen in breast cancer. CMF regimen has shown treatment associated survival benefit for over 40 years and it still is the standard chemotherapeutic regimen in breast cancer although the use of anthracycline and taxane based chemotherapy has been extended to early breast cancer [3,4].
However, in spite of its many merits as chemotherapeutic regimen, it frequently has been pointed out that cyclophosphamide, as an alkylating agent, induces permanent amenorrhea in premenopausal women who plan to have conception after treatment. In addition, methotrexate and 5-fluorouracil have the same anticancer mechanism as anti-metabolites [5-8].
Since 2000, we have administered cyclophosphamide, vinorelbine and 5-fluorouracil (CVF) instead of CMF regimen in early breast cancer patients because the authors considered that CVF regimen is more reasonable than the latter for early breast cancer considering the drug combination. Vinorelbine is frequently used in advanced breast cancer and has an acceptable overall response rate of about over 40% when used in first line [9-16]. Recently, one study group conducted a clinical trial with vinorelbine in early breast cancer patients with poor prognostic factors and they concluded that vinorelbine containing regimen provided a reliable efficacy [17].
The current study was performed to evaluate the feasibility of CVF regimen in early breast cancer when the disease-free survival and overall survival of CVF regimen are compared with those of CMF regimen.
We randomly assigned 149 breast cancer patients to either CMF or CVF adjuvant chemotherapy after the breast surgery and axillary lymph node dissection (or sentinel lymph node biopsy) at Inje University Sanggye Paik Hospital.
All patients were early breast cancer (stage I, II) patients with World Health Organization (WHO) performance status 0-2 and have proper bone marrow, liver, and renal functions. The Institutional Review Board (99-32) approved the study.
All patients agreed on the informed consents and were provided with enough counseling for surgery and adjuvant systemic chemotherapy. Patient with active infection, severe systemic disease (i.e., uncontrolled diabetes, liver cirrhosis, congestive heart failure, etc.), or serious psychiatric problem were excluded from the systemic adjuvant chemotherapy.
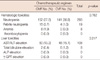
Regarding the clinical stage, 52 (77.6%) were stage I and 15 (22.4%) were stage II in the CMF group, and 43 (52.4%) were stage I and 39 (47.6%) were stage II in the CVF group (Table 1). Although the latter had a slightly larger numbe r of stage II patients, there was no statistical difference between the two (p=0.052). Also the CVF group had a larger number of patients with a tumor size more than 2 cm (p=0.422) or lymph node metastasis (p=0.192), but they were also statistically not significant (Table 1).
In comparison of the histological grade and the nuclear grade between the two groups, there was no statistical significance between the two groups. When the hormonal receptor status and the expression of HER2/neu were compared between the two groups, the CMF group had more patients with the two receptors and also HER2/neu expression, but there was no statistical significance (p=0.621). The CMF group had significantly higher bcl-2 expression (p=0.026), whereas the Ki-67 labeling index was not statistically significant
In control group, CMF regimen consisting of cyclophosphamide (600 mg/m2 intravenously on day 1), methotrexate (40 mg/m2 intravenously on day 1) and 5-fluorouracil (600 mg/m2 intravenously on day 1), was repeated every three weeks for six cycles. In the study group, six cycles of CVF regimen consisting of cyclophosphamide (600 mg/m2 intravenously on day 1), vinorelbine (30 mg/m2 intravenously on day 1) and 5-fluorouracil (600 mg/m2 intravenously on day 1) was repeated every three weeks.
Blood samples of all patients were obtained on the fourteenth and 20th days after the start of chemotherapy for the surveillance of toxicities and recovery from nadir. When the pretreatment evaluations were acceptable to continue chemotherapy, the patients were administered for the next cycle of chemotherapy as scheduled.
Locoregional radiation therapy after the surgery were conducted in patients who received breast conserving surgery and in those who were confirmed to have axillary lymph node metastasis in the pathology report, axilla was included in the radiation field as well. Also in those who received modified radical mastectomy but whose pathology report showed presence of cancer cell in less than 1 mm from the deep margin or axillary lymph node metastasis, locoregional radiation treatment was done. The entire breast parenchyma was included in the tangential field for radiation of 6MV X-ray and an additional irradiation was done on the tumor bed. The mean radiation dose was 56 Gy (range, 52-63 Gy) and the fractional dose was 56 Gy (range, 52-63 Gy). Each fraction dose was 1.8 Gy and the mean number of fraction was 30 (range, 28-33), and it took 6-7 weeks in total [18].
Radiation therapy was conducted concomitantly with the chemotherapy. Post-operative hormone therapy was indicated in hormone receptor-positive patients and those whose receptor status was not known. Anti-estrogen was the primary choice for the hormonal therapy and in post-menopausal patients with hypercholesterolemia, pulmonary embolism, or deep vein thrombosis, but without osteoporosis, aromatase-inhibitors were considered secondarily.
For calculation of sample size, we expected the systemic recurrence rate of both CVF and CMF chemotherapy as 10% (7-15%). The sample size was calculated on the basis of expected dropout rate of 10%. Around 95 subjects per each group were needed to evaluate the equivalent therapeutic efficacy of CVF chemotherapy to CMF chemotherapy.
Neutropenia, febrile neutropenia, anemia, thrombocytopenia, hepatotoxicity, and nephrotoxicity during the period of chemotherapy in the two groups were analyzed by Pearson's chi-square test using SPSS software version 11.0 (SPSS Inc., Chicago, USA), and the p-value of less than or equal to 0.05 was considered statistically significant.
Treatment results in each group according to the patient age, tumor size, number of lymph node metastases, stage, surgical strategy, histologic grade, nuclear grade, estrogen receptor, progesterone receptor, HER2/neu expression, Ki-67 labeling index, bcl-2 expression, hormonal therapy, and radiation therapy were evaluated by Cox regression analysis and the p-value of less than or equal to 0.05 was considered statistically significant.
Between September 2000 and December 2007, only 149 patients were enrolled to the study. The study was closed at December 2007 because of slow enrollment although the planned number of patients had not been enrolled.
Out of the 149 patients, 67 received CMF regimen and the remaining 82 received CVF regimen. The age range was 23-71 (mean, 48.5) for the former and 31-66 (mean, 49.1) for the latter. The menopausal status of each patient was not recorded, but patients less than the age 50 were 42 (62.7%) in the CMF group and 48 (58.5%) in the CVF group. The number of patients aged more than 50 was 25 (37.3%) in the former and 34 (41.5%) in the latter. The age (p=0.354) and the menopausal status (p=0.387) were not statistically significant between the two groups (Table 1).
The surgical methods in each group were 52 (77.6%) cases of breast conserving surgery and 15 (22.4%) cases of modified radical mastectomy in the CMF group, and 64 (78.%) cases of breast conserving surgery and 18 (22%) cases of modified radical mastectomy in the CVF group. There was no statistical difference between the two groups. Adjuvant hormonal therapy after the surgery and chemotherapy was administered in 51 patients of CMF group and in 67 patients of CVF group. Locoregional radiation treatment was done in 47 of CMF group and in 50 of CVF group (Table 1). There was no statistical difference between the two groups regarding adjuvant hormonal therapy (p=0.310) and locoregional radiation (p=0.347).
The median follow-up period was 59 months (range, 18-105 months). In the CVF group, 5 patients had recurrent disease whereas 6 patients of the CMF group had recurrent disease. The disease-free survival rate was 93.9% for the former and 91.0% for the latter (p=0.057) (Figure 1).
During the follow-up, 2 patients (2.4%) of CVF group died of recurrent breast cancer, whereas 3 patients (4.4%) of CMF group expired. There was no significant difference in overall survival of the patients between the two groups (p=0.155) (Figure 2).
Both disease-free survival and overall survival rates appeared to be lower in the CMF group compared with CVF group, but its statistical significance could not be verified due to the small number of patients.
In evaluation of chemotoxicity, neutropenia in CMF group was observed in 152 cycles out of 403 cycles (37.7%), of which grade 3 or 4 neutropenia was in 20 cycles (4.9%). Similarly, neutropenia in CVF group was observed in 141 cycles out of 381 cycles and grade 3 or 4 neutropenia was in 19 cycles (4.9%). There was no statistical difference between the two groups regarding neutropenia (p=0.762). Anemia was noted in 8 cycles in the CMF group and thrombocytopenia was not observed in both groups (Table 2).
Liver enzyme level was abnormal in 118 out of 788 cycles and grade 3 or 4 hepatotoxicity was in 1 cycle in the CMF group and in 7 cycles in the CVF group. They were all grade 3 hepatotoxicity and all the patients recovered after chemotherapy. There was no statistical difference in terms of adverse effect from chemotherapy between the 2 groups (p=0.217).
Systemic adjuvant chemotherapy is one of the standard treatment modalities for the breast cancer since the 1970s when Bonadonna et al. [5] started to use CMF regimen for the chemotherapy of breast cancer. But from the 1990s, anthracycline and taxane became the key chemotherapeutic agents for the breast cancer because the results of large clinical trials showed additional survival benefits when compared with CMF [19,20]. Although anthracycline containing regimens have marginal superiority in terms of disease free and overall survival, several toxicities from anthracycline such as cardiotoxicity and alopecia are still the main obstacle to wide use of anthracycline regimens in adjuvant setting for early breast cancer. Alopecia is specifically a main complaint in Korean women with breast cancer. Many women hesitate to return to their social activity due to alopecia even after the completion of adjuvant chemotherapy. There was no grade 3 or 4 alopecia in both CMF and CVF group in the current study. Thus, the compliance to the CVF chemotherapy was good in studied patients.
Subset analysis of recent clinical trials has indicated that the benefit of anthracycline might confine to small subset of patients who harbor HER2 and/or topoisomerase2-alpha amplification [21,22]. The results of those clinical trials suggest that the patients who do not have HER2 and/or topoisomerase2-alpha amplification may not benefit from anthracycline containing regimens. The results of recent clinical trials in terms of anthracycline sensitivity have to be verified by further study, since the meta-analysis of early breast cancer treatment trials consistently shows the increased survival benefit of anthracycline containing regimens compared with CMF [23]. However, obligatory use of anthracycline in early breast cancer needs to be reconsidered when we consider the increased incidence of adverse effects by anthracycline. That is a reason why we have designed the current study.
The authors speculated that since methotrexate and 5-fluorouracil have the same anticancer mechanism, methotrexate can be substituted by another drug with different anticancer mechanism and the results would not be inferior. As aforementioned, vinorelbine, a potent inhibitor of mitotic microtubule polymerization and whose chemotherapeutic effect has been validated in progressive and metastatic breast cancer, started to be used in the place of methotrexate, an antimetabolite [9,15,16].
There was one study reporting the chemotherapeutic effect of vinorelbine combined with other drugs on progressive and recurrent breast cancer. Ardavanis et al. [24] reported complete remission rate of 12%, partial remission rate of 38%, and overall response rate of 51% in metastatic, locally progressive, or recurrent breast cancer patients with CVF regimen. Recently, vinorelbine containing chemotherapeutic regimen has been tried in early breast cancers in clinical trials [25] and a French study has reported in a clinical trial that epirubicin and vinorelbine (EV) regimen is not inferior to 5-fluorouracil, epirubicin and cyclophosphamide (FEC) regimen in lymph node positive early breast cancer [17].
Our study, the first to use CVF regimen in stage I and II early breast cancer, showed an almost equal or slightly better results with respect to the disease-free survival and overall survival when compared to CMF regimen. The CVF regimen had no statistically significant difference to the CMF regimen with respect to the bone marrow toxicity or hepatotoxicity. Thus, CVF regimen is expected to be the reasonable effective substitute for the CMF regimen in early breast cancer.
In conclusion, CVF regimen, when compared to the CMF regimen, seems to be a safe and effective chemotherapeutic regimen in early breast cancer with comparable outcomes to CMF. However, our study was limited by small number patients. Prospective clinical study with a larger number of patients is necessary to verify the efficacy of CVF regimen as an adjuvant chemotherapeutic agent in early breast cancer.
Figures and Tables
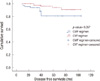 | Figure 1Disease-free survival curves of CVF (cyclophosphamide+vinorelbine+5-fluorouracil) and CMF (cyclophosphamide+methotrexate+5-fluorouracil) groups. |
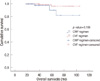 | Figure 2Overall survival curves of CVF (cyclophosphamide+vinorelbine+5-fluorouracil) and CMF (cyclophosphamide+methotrexate+5-fluorouracil) groups. |
References
1. Shackney SE, McCormack GW, Cuchural GJ Jr. Growth rate patterns of solid tumors and their relation to responsiveness to therapy: an analytical review. Ann Intern Med. 1978. 89:107–121.

2. Cosse JP, Michiels C. Tumour hypoxia affects the responsiveness of cancer cells to chemotherapy and promotes cancer progression. Anticancer Agents Med Chem. 2008. 8:790–797.

3. Heys SD, Sarkar T, Hutcheon AW. Primary docetaxel chemotherapy in patients with breast cancer: impact on response and survival. Breast Cancer Res Treat. 2005. 90:169–185.

4. Julka PK, Awasthy BS, Sharma DN, Gairola M, Rath GK. Paclitaxel-epirubicin in advanced breast cancer. J Assoc Physicians India. 1999. 47:499–502.
5. Bonadonna G, Rossi A, Valagussa P, Veronesi U. Actual data on efficacy of surgical adjuvant chemotherapy with CMF in breast cancer. Arch Geschwulstforsch. 1978. 48:659.
6. Tancini G, Bajetta E, Marchini S, Valagussa P, Bonadonna G, Veronesi U. Preliminary 3-year results of 12 versus 6 cycles of surgical adjuvant CMF in premenopausal breast cancer. Cancer Clin Trials. 1979. 2:285–292.
7. Bonadonna G, Valagussa P, Rossi A, Tancini G, Brambilla C, Zambetti M, et al. Ten-year experience with CMF-based adjuvant chemotherapy in resectable breast cancer. Breast Cancer Res Treat. 1985. 5:95–115.

8. Bonadonna G, Moliterni A, Zambetti M, Daidone MG, Pilotti S, Gianni L, et al. 30 years' follow up of randomised studies of adjuvant CMF in operable breast cancer: cohort study. BMJ. 2005. 330:217.

9. Krikorian A, Breillout F. Vinorelbine (Navelbine). A new semisynthetic vinca alkaloid. Onkologie. 1991. 14:7–12.

10. Fumoleau P, Delgado FM, Delozier T, Monnier A, Gil Delgado MA, Kerbrat P, et al. Phase II trial of weekly intravenous vinorelbine in first-line advanced breast cancer chemotherapy. J Clin Oncol. 1993. 11:1245–1252.

11. Gasparini G, Caffo O, Barni S, Frontini L, Testolin A, Guglielmi RB, et al. Vinorelbine is an active antiproliferative agent in pretreated advanced breast cancer patients: a phase II study. J Clin Oncol. 1994. 12:2094–2101.

12. Ejlertsen B, Mouridsen HT, Langkjer ST, Andersen J, Sjöström J, Kjaer M, et al. Phase III study of intravenous vinorelbine in combination with epirubicin versus epirubicin alone in patients with advanced breast cancer: a Scandinavian Breast Group Trial (SBG9403). J Clin Oncol. 2004. 22:2313–2320.

13. Chua S, Smith IE, A'Hern RP, Coombes GA, Hickish TF, Robinson AC, et al. Neoadjuvant vinorelbine/epirubicin (VE) versus standard adriamycin/cyclophosphamide (AC) in operable breast cancer: analysis of response and tolerability in a randomised phase III trial (TOPIC 2). Ann Oncol. 2005. 16:1435–1441.

14. Weber BL, Vogel C, Jones S, Harvey H, Hutchins L, Bigley J, et al. Intravenous vinorelbine as first-line and second-line therapy in advanced breast cancer. J Clin Oncol. 1995. 13:2722–2730.

15. Elomaa I, Joensuu H, Blomqvist C. Vinorelbine, epirubicin and fluorouracil as first-line therapy in metastatic breast cancer--a phase II trial. Acta Oncol. 2003. 42:309–314.

16. Vici P, Di Lauro L, Sergi D, Foggi P, Viola G, Mottolese M, et al. A phase II trial of docetaxel and vinorelbine in patients with advanced breast cancer previously treated with anthracyclines. Oncology. 2008. 75:175–181.

17. Kerbrat P, Roché H, Bonneterre J, Veyret C, Lortholary A, Monnier A, et al. Epirubicin-vinorelbine vs FEC100 for node-positive, early breast cancer: French Adjuvant Study Group 09 trial. Br J Cancer. 2007. 96:1633–1638.

18. Cho H, Kwak K, Kim J, Sohn SC, Park K, Han S. Feasibility of concurrent adjuvant chemotherapy and radiotherapy after breast-conserving surgery in early breast cancer. J Korean Breast Cancer Soc. 2004. 7:289–293.

19. Fisher B, Brown AM, Dimitrov NV, Poisson R, Redmond C, Margolese RG, et al. Two months of doxorubicin-cyclophosphamide with and without interval reinduction therapy compared with 6 months of cyclophosphamide, methotrexate, and fluorouracil in positive-node breast cancer patients with tamoxifen-nonresponsive tumors: results from the National Surgical Adjuvant Breast and Bowel Project B-15. J Clin Oncol. 1990. 8:1483–1496.

20. Valero V, Holmes FA, Walters RS, Theriault RL, Esparza L, Fraschini G, et al. Phase II trial of docetaxel: a new, highly effective antineoplastic agent in the management of patients with anthracycline-resistant metastatic breast cancer. J Clin Oncol. 1995. 13:2886–2894.

21. Slamon DJ, Press MF. Alterations in the TOP2A and HER2 genes: association with adjuvant anthracycline sensitivity in human breast cancers. J Natl Cancer Inst. 2009. 101:615–618.

22. Levine MN, Pritchard KI, Bramwell VH, Shepherd LE, Tu D, Paul N, et al. Randomized trial comparing cyclophosphamide, epirubicin, and fluorouracil with cyclophosphamide, methotrexate, and fluorouracil in premenopausal women with node-positive breast cancer: update of National Cancer Institute of Canada Clinical Trials Group Trial MA5. J Clin Oncol. 2005. 23:5166–5170.

23. Early Breast Cancer Trialists' Collaborative Group (EBCTCG). Effects of chemotherapy and hormonal therapy for early breast cancer on recurrence and 15-year survival: an overview of the randomised trials. Lancet. 2005. 365:1687–1717.
24. Ardavanis A, Extra JM, Espié M, Cuvier C, Marty M. Phase II trial of a combination of vinorelbine, cyclophosphamide and 5-fluorouracil in the treatment of advanced breast cancer. In Vivo. 1998. 12:559–562.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download