Abstract
Hidradenoma papilliferum (HP) is a benign neoplasm arising from mammary-like glands which typically involves the dermal layer of the female anogenital area. The prognosis for HP is good. Recurrence is unusual and is typically attributed to incomplete excision of the primary tumor. Malignant transformation is rare and HP of the breast has not yet been reported. Ectopic HP is usually solitary, small, and asymptomatic. It appears as a well-circumscribed, complex cystic mass in the dermis on ultrasound. We present a case of HP arising from the axillary tail of the breast.
Hidradenoma papilliferum (HP) is a benign neoplasm involving anogenital mammary-like glands (MLG) and occurs most commonly in the vulva or perianal region of adult white women [1,2]. It is histopathologically similar to intraductal papilloma of the breast. The lesions are usually solitary, well-demarcated papules or nodules covered with normal skin, and are generally less than 10 mm in diameter [3]. When these tumors are not located in the anogenital area, they are termed ectopic HP [4].
MLG have been documented in ectopic areas of the skin such as the ear, face, chest, and scalp. Ectopic HP can arise from anywhere which MLG are located. Most of all are excised without suspicious. As a result, its imaging findings are not well known. Then, the purpose of our report was to provide imaging findings of ectopic HP in axillary tail of the breast as rare location.
A 46-year-old woman presented with a 5-year history of a slowly growing, palpable mass on the left breast. Physical examination revealed a 4 cm, soft and movable, brown colored mass at the 2 o'clock location in the axillary tail region of the left breast. She had no remarkable medical or family history.
An ultrasound (iU22 unit; Philips Medical Systems, Bothell, USA) of the left breast revealed grouped, 1-2 cm, well-circumscribed, round solid masses with internal cystic components in the dermis that abutted the subcutaneous layer of the left breast (Figure 1) and were located in the axillary tail. Radiologically, these lesions were considered to be Breast Imaging Reporting and Data System (BI-RADS) Category 3 [5]. Provisional diagnosis of atypical dermoid cysts had been postulated. She underwent surgical excision.
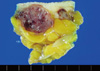
Grossly, Part of the nodules was well encapsulated, lobular masses with purple-brown cut surface that abutted but didn't penetrate the skin (Figure 2). Hematoxylin and eosin (H&E) sections, ×1 (Figure 3A) and ×200 (Figure 3B) revealed dermally based nodules with complex architecture and uninvolved epidermis. The nodules consisted of a cyst with large arborizing papillae which had fibrovascular core. The non-neoplastic breast tissue underneath the tumor showed focal apocrine metaplasia. Microscopically, the lesions are cystic papillary tumors and are composed of proliferation of papillary fronds made of loose fibrous connective tissue lined by pseudostratified bland-looking epithelial cells. Histologic examination of the lesion revealed findings consistent with HP. The immunohistochemical staining for estrogen receptor (ER) or progesterone receptor (PR) were all positive and HER2 protein was negative.
HP is a skin appendage tumor that is most commonly reported on the anogenital region of women, particularly the vulva. HP has been considered to be derived from apocrine glands. However, the observed similarities of HP with intraductal papillomas of the breast indicate that MLG is the true origin of HP. HP primarily affects Caucasian females, typically during the third to fifth decades of life. Ectopic HPs occur on non-anogenital sites in older patients, with an equal incidence in males and females [4].
MLG are normal finding in the anogenital region of males and especially females. MLG are located in the subepidermal stroma, larger than apocrine or eccrine glands, frequently branched and sometimes truly lobulated, lined by basophilic rather than eosinophilic cells and are ER or PR positive. MLG have been documented in ectopic areas of the skin such as the ear, face, chest, and scalp [4]. Therefore, the ectopic HP could occur in these regions and 19 cases of ectopic HPs have been reported in the English language literature (Table 1). Most common site of ectopic HPs was on head and neck.
The classification of cutaneous sweat gland lesions is very complex, as these lesions have a wide histological spectrum, and the pathogenesis and exact origin of many of these lesions is still under investigation and is unclear. Many different terms are often used to describe the same tumor. Eccrine sweat glands are widely distributed almost everywhere in the skin, but apocrine lesions of the skin are rare and are found mainly in body folds including the axillary, groin, and anogenital regions.
HP is usually solitary, small, and asymptomatic. Occasionally, the tumors can be large and elevated, forming a reddish-brown mass with an ulcerated and bleeding surface. The incidence of multiple lesions is reported as 5% and all multiple lesions have been described as unilateral [6]. Histologically, it is a well-circumscribed, solid or cystic, dermal nodular lesion, not connected to the epidermis. The prognosis for both anogenital and ectopic HP is good. Regardless of the site, the treatment of choice is local excision. Recurrence of anogenital and ectopic HP is unusual and is typically attributed to incomplete excision of the primary tumor. Malignant transformation is rare.
In women, anogenital and ectopic HP tumors have only been reported after the onset of puberty. Hence it is possible that estrogen stimulation may play a role in the pathogenesis of HP in women. Whether estrogens are involved in ectopic HP in men remains to be evaluated. Typical eccrine and apocrine sweat glands were devoid of both ER and PR. Thus, ER and PR seem to be reliable markers for distinguishing female anogenital glands from conventional sweat glands [7]. Our case was also positive for ER and PR on immunohistochemical staining. However, our case arose from the breast dermis. It is important to remember that ER and PR positivity has been described in a subset of breast cancers, including papillary neoplasms. Accordingly, ER and PR immunohistochemical staining should not be used to distinguish breast tumors from HP.
HER2 protein is also useful immunostain to distinguish breast adenocarcinoma from skin adnexal tumors. Less than 0.5% of cutaneous eccrine and apocrine neoplasms are associated with positive HER2 immunohistochemical staining [8], whereas 20% of invasive breast adenocarcinomas are HER2 positive.
Ultrasound is used to identify and characterize such masses. Complex cystic breast masses demonstrate both anechoic (cystic) and echogenic (solid) components on ultrasound. Common benign findings include fibrocystic changes and intraductal or intracystic papillomas. Moreover, HP has features analogous to an intraductal papilloma of the breast which can lead to misdiagnosis. But, most papillomas are located in breast parenchyma and are related to ducts, although some peripheral type of papilloma looks like only solid mass.
Adnexal tumor appears as a fairly well-demarcated cystic-solid mass in the dermis and HPs have similar findings. Due to the rarity of this tumor, and its common removal without imaging studies because of small size, typical radiological findings have not yet been well established.
In conclusion, skin adnexal tumors, specifically HP, should be kept in the differential diagnosis when evaluating a subcutaneous breast tumor. To our knowledge, this is the first case report of HP developed in the breast skin of middle-aged woman.
Figures and Tables
 | Figure 1Ultrasound shows three, round complex masses in the dermis which abutted the subcutaneous fat layer of the left breast. |
 | Figure 3Microscopic findings of the lesions (A, H&E stain, ×1; B, H&E stain, ×200). The lesions are composed of proliferation of papillary fronds made of loose fibrous connective tissue lined by pseudostratified bland-looking epithelial cells. These findings are consistent with the cystic papillary tumors. |
References
1. Cunningham JA, Hardy J. Hidradenomas of the vulva: report of four cases with an evaluation of them in the light of analogous breast lesions. South Surg. 1947. 13:831–838.

2. van der Putte SC. Mammary-like glands of the vulva and their disorders. Int J Gynecol Pathol. 1994. 13:150–160.

3. James WD, Berger T, Elston D. Andrews' Diseases of the Skin: Clinical Dermatology. 2006. 10th ed. Philadelphia: W.B. Saunders;667–668.
4. Vang R, Cohen PR. Ectopic hidradenoma papilliferum: a case report and review of the literature. J Am Acad Dermatol. 1999. 41:115–118.

5. American College of Radiology. BI-RADS®-Ultrasound. Breast Imaging Reporting and Data System Atlas (BI-RADS® Atlas). 2003. 1st ed. Reston: American College of Radiology.
6. Woodworth H Jr, Dockerty MB, Wilson RB, Pratt JH. Papillary hidradenoma of the vulva: a clinicopathologic study of 69 cases. Am J Obstet Gynecol. 1971. 110:501–508.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download