Abstract
Purpose
The negative sentinel lymph node (SLN) biopsy avoids conventional axillary dissection in patients with breast cancer with clinically negative axilla. Despite negative SLN, there is a risk of leaving involved non-SLN behind in the axilla. We investigated the predictive power of tumor characteristics for non-SLN metastasis.
Methods
Lymphatic mapping with blue dye method for SLN biopsy and level 1-2 axillary dissections were performed to establish axillary status in 59 patients with T1 and T2 breast cancer and clinically negative axilla. Tumor's characteristics were histopathologically established to assess their association with non-SLN metastasis.
Results
The axilla was malignant in 23 (39%) patients. The SLN alone was metastatic in 10, both SLN and non-SLN in 9, and non-SLN alone in 4 (7%) patients. The false negative rate for SLN biopsy was 10% in our series. The rate of positive non-SLN was found as 0% in T1a-b, 19% in T1c, and 40% in T2 tumors (p=0.035). Lymphovascular invasion was positive in 14 (61%) patients with axillary metastasis (p<0.001), and in 10 (77%) patients with non-SLN involvement (p<0.001).
The axillary status is the most important prognostic marker in patients with invasive breast cancer. Modern screening methods have increased the possibility of early detection of malignant tumor in the breast. Early diagnosis of smaller carcinoma has gradually decreased the rate of axillary involvement. Sentinel lymph node (SLN) biopsy is an accepted method for defining pathologic axillary status in early cancer cases with clinically negative axilla. The negative SLN is generally accepted as the representative of the negative axilla [1-3]. On the other hand, a risk for non-SLN involvement is always present despite negative SLN biopsy. Non-SLN metastasis increases the risk of axillary (loco-regional) recurrence in the non-dissected axillary tissue. Thus, meaningful markers for predicting SLN and non-SLN involvement in patients with early breast cancer are needed. The presence of tumor emboli within the peritumoral endothelial lined spaces is defined as lymphovascular invasion (LVI). LVI is easily established by histopathological examination. The pathological report of the presence of LVI may help determine whether patients with cancer are at increased risk for regional and systemic spread. LVI may indicate the invasiveness power of breast cancer as indicator of high biological aggressiveness [4-6].
In this study, we investigated the relationship between tumor characteristics and axillary status in patients with early breast cancer. The study was conducted to establish the effect of LVI for predicting lymphatic metastasis, especially beyond SLN.
We analyzed 59 surgically treated patients with early breast cancer (invasive ductal cancer) in the years 2007 and 2008. Patients had T1 and T2 primary tumor and clinically negative axilla. T1 tumors were detected by physical examination and/or by mammography and/or ultrasonography for non-palpable lesions. The diagnosis was established by core biopsy, fine needle aspiration or stereotactic biopsy. The SLN was identified by subareolar injection of blue dye (isosulphan blue), the SLN was excised via an axillary incision for pathological analysis. The mean number of removed SLNs was 1.8 (range, 1-4). Patients were surgically treated by total mastectomy or by wide local excision. Level 1 and 2 axillary dissection was then performed to determine non-SLN involvement. Lymph nodes were identified and stained with hematoxylin and eosin (H&E) and examined for tumor metastasis. Tumor and peritumoral breast tissue were examined for LVI. The presence of tumor emboli within peritumoral endothelial lined spaces, stained with H&E is defined as positive LVI. We compared the presence of LVI and other prognostic markers with the results of pathological analyses regarding axillary status (SLN and non-SLNs involvement) in order to establish the predictive value for prognostic markers and LVI for lymphatic metastasis.
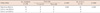
The mean age was 52 years (range, 29-78 years). Twenty one (36%) patients were premenopausal. Thirty-nine (66%) patients had T1 tumors. The LVI was detected in 19 (32%) patients, and 23 (39%) patients had axillary lymphatic metastasis (Table 1).
The SLN was metastatic in 19 patients and negative in 40. The SLN was the only metastatic node in 10 patients. Four patients had non-SLN metastasis despite negative SLN. Therefore, the false negative rate (FNR) was 10% (4/40) in our series. The menopausal feature of the patients, and grade and hormone receptor status of the primary tumors had no significant influence on non-SLN metastasis, but tumor size and LVI had an influence according to univariate and multivariate analyses (Table 1).
The LVI was negative in 86% of breast cancer cases with negative axilla, and the LVI was positive in 61% (p<0.001) of cases with involved axilla. The presence of peritumoral LVI increased according to SLN and non-SLN status (Table 2). Non-SLN invasion was absent (0/12) in T1a and b, and was 28% (13/47) in T1c and T2 tumors (p=0.035) (Table 3). Malignant cells have involved non-SLN in 0% of patients with T1a-b, in 19% (5/27) of patients with T1c and 40% (8/20) of with T2 tumors (p=0.022). Positive LVI was found in 77% (10/13) of patients with non-SLN metastasis (p<0.001) (Table 4).
Screening methods permit us to diagnose early breast cancer cases with clinically negative lymph nodes. The concept of SLN biopsy was developed in patients with early cancer in order to define axillary status before formal dissection of the axilla. After histopathological examination, axillary dissection may be avoided in patients with negative SLN biopsy [1,3,7]. On the other hand, a small but important risk of non-SLN involvement exists despite negative SLN. These skip metastases increase the risk of axillary recurrence in the non-dissected tissue after pathological report of negative SLN biopsy. The concept of non-SLN involvement includes both skip (SLN negative, non-SLN positive) and other (SLN positive, non-SLN positive) lymph nodes metastases beyond SLNs. Although SLN biopsy is highly accurate for predicting axillary nodal status, it has been shown that the procedure has been associated with a several false negative results [8]. We need some indicator of non-SLN involvement for determining the subgroup of patients at risk, and prevention of loco-regional recurrence due to leaving metastatic nodes behind in the non-dissected axilla when the SLN biopsy is negative.
Our rate (39%) of axillary involvement was slightly higher than that of similar series in the literature. The rate of positive nodes has been reported between 12% and 29% in previous studies of early breast cancer cases with SLN biopsy [9-12]. On the other hand, there are also some series with positive SLN biopsy rates as between 32% and 40% [13-15]. Our rate of lymphatic metastasis and our findings about tumor characteristics indicate that tumor size is an important factor for axillary involvement. Relatively high rate of T2 tumors in our series increased the risk of axillary metastasis. Okamoto et al. [8] reported that axillary metastasis was observed in 6% of T1a and b and 25% of T1c tumors.
The completion axillary dissection has been omitted in patients with negative SLN biopsy. The rate of negative SLN was 68% (40/59) in our series. The rate of SLN free of tumor has been reported as 60-88% in recent series [9-15]. The FNR of SLN biopsy is defined as non-SLN (skip) metastases despite negative SLN. Our FNR of 10% (4/40) was comparable with those of previous series. Our higher FNR mainly resulted from the relatively high number of T2 cases. Some series have had a FNRs of 0-0.5% [9,16], and some others between 2.7% and 17% [8,14,17-20]. The higher FNR in our T2 cases emphasizes the importance of tumor size. Okamoto et al. [8] have estimated the probability of FNR as 1% for T1a-b, 6% for T1c and 8% for T2 tumors. In some series, the risk of clinically important axillary recurrence has been reported as 0.5% in early cancer cases in whom axillary status was assessed by SLN biopsy [9,12,16,21].
The prevention of loco-regional recurrence is only possible by detecting false negative cases and negative SLN with skip (non-SLN) metastases. Carcoforo et al. [9] have reported three false negative cases that all three patients presented as an axillary recurrence in 24 months. This result has also been confirmed by others [12,16,21]. How can we detect the false negative cases? Which patients have higher risk for non-SLN involvement? Although the SLN biopsy was negative, the completion axillary lymph node dissection (ALND) must be performed in patients with higher risk of non-SLN involvement in order to eliminate the risk of leaving metastatic nodes behind in the axilla. In our study, the rate of non-SLN metastasis in T1c and in T2 tumors revealed has showed the importance of tumor size for lymphatic metastasis beyond SLN. The higher FNR in T2 cases also confirms the role of larger tumors on positive non-SLN, despite negative SLN. Therefore, a primary tumor size near 2 cm or more significantly increased the risk for non-SLN involvement. Tan et al. [10] also reported that tumor size greater than 15 mm was significantly associated with SLN macro metastasis which had a higher risk of tumor involvement in non-SLN. Cao et al. [15] also pointed out the strong metastatic ability of worse malignant lesions. Tumor size greater than 2 cm was an independently significant prognostic marker for loco-regional recurrence, and was associated with a higher risk for developing lymphatic metastasis [22-25].
Another important marker of lymphatic spread is peritumoral LVI. We observed that the rate of LVI increased gradually according to tumor size and axillary metastasis. The diagnosis of early cancer cases decreased the risk of lymphatic spread in approximately half (10/23; 43%) of our metastatic cases with SLN involvement alone. The importance of micro and macro metastasis in SLN has been previously established [10,13,24]. The macrometastasis has been well documented factor for increasing the risk of non-SLN involvement. Tan et al. [10] reported that LVI was significantly associated with SLN macro metastasis. The NSABP B2 trial demonstrated that LVI increases the risk of lymph node involvement in 70-year-old patients with T1 or T2 breast cancer from 10% to 45% [26]. Our rate of positive LVI (10/13; 77%) in our patients with non-SLN metastasis suggested that LVI was a strong positive predictor of the non-SLN involvement. The results of recent studies have also confirmed that LVI was significantly associated with lymph node status and non-SLN metastasis in breast cancer cases [24,27-29]. Previous studies have recently shown that LVI and larger (T2) primary tumors are predictors of the risk of non-SLN metastasis [25,30]. Based on ours and other findings, although SLN was negative, completion ALND might be considered for patients with T2 tumors and with LVI in order to eliminate the risk of leaving positive nodes behind and to prevent locoregional recurrence. This does not mean that SLN biopsy is not suitable for patients with cT2N0 breast cancer. It means that surgeons must be more alert for non-SLN involvement in case of patients with larger tumor.
One of the most important factors for patient's survival is false negative cases in which non-SLN harbors malignant cells despite negative SLN biopsy. Despite a small number of patients, our LVI results in metastatic non-SLN and false negative cases indicated the adverse effect of LVI, which has promoted non-SLN metastasis. It was generally accepted that negative SLN biopsy cases have a better prognosis, as well as disease-free and overall survival. On the other hand, breast cancer cases with LVI have poorer prognoses among node-negative cases [22,23]. Node-negative patients with LVI are at higher risk for locoregional recurrence, relapse, disease free and overall survival [22,23,30]. The results of LVI and tumor size in our patients revealed that the presence of peritumoral LVI and larger tumor (>2 cm) were strong indicators of non-SLN metastasis.
There is a small but important risk of false negative SLN biopsy when non-SLN is involved with malignant cells despite negative SLN. Greater tumor size and positive LVI were adverse markers for axillary metastasis. Tumor size (>2 cm) was significantly associated with non-SLN metastasis. Peritumoral LVI was a positive predictor of the metastatic involvement of non-SLN. Despite negative SLN, completion ALND may be considered in patients with larger tumor and positive LVI in order to avoid leaving metastatic non-SLNs behind in the axilla.
Figures and Tables
References
1. Brennan M, Wilcken N, French J, Ung O, Boyages J. Management of early breast cancer--the current approach. Aust Fam Physician. 2005. 34:755–760.
2. Gurleyik G, Aker F, Sekmen U, Saglam A. Accuracy of sentinel lymph node biopsy for the assessment of axillary status in patients with early (T1) breast carcinoma. J Coll Physicians Surg Pak. 2005. 15:697–700.
3. Nitz U, Grosse R, Thomssen C. Breast cancer surgery: oncological aspects. Breast Care. 2006. 1:229–233.
4. Shen J, Hunt KK, Mirza NQ, Buchholz TA, Babiera GV, Kuerer HM, et al. Predictors of systemic recurrence and disease-specific survival after ipsilateral breast tumor recurrence. Cancer. 2005. 104:479–490.

5. Gurleyik G, Gurleyik E, Aker F, Aktekin A, Emir S, Gungor O, et al. Lymphovascular invasion, as a prognostic marker in patients with invasive breast cancer. Acta Chir Belg. 2007. 107:284–287.

6. Schoppmann SF, Bayer G, Aumayr K, Taucher S, Geleff S, Rudas M, et al. Prognostic value of lymphangiogenesis and lymphovascular invasion in invasive breast cancer. Ann Surg. 2004. 240:306–312.

7. Houssami N, French J, Brennan M, Ahern V, Ung O. Breast cancer--new and emerging technologies for diagnosis and management. Aust Fam Physician. 2005. 34:657–661.
8. Okamoto T, Yamazaki K, Kanbe M, Kodama H, Omi Y, Kawamata A, et al. Probability of axillary lymph node metastasis when sentinel lymph node biopsy is negative in women with clinically node negative breast cancer: a Bayesian approach. Breast Cancer. 2005. 12:203–210.

9. Carcoforo P, Sortini D, Soliani G, Basaglia E, Feggi L, Liboni A. Accuracy and reliability of sentinel node biopsy in patients with breast cancer. Single centre study with long term follow-up. Breast Cancer Res Treat. 2006. 95:111–116.

10. Tan YY, Wu CT, Fan YG, Hwang S, Ewing C, Lane K, et al. Primary tumor characteristics predict sentinel lymph node macrometastasis in breast cancer. Breast J. 2005. 11:338–343.

11. Soni NK, Carmalt HL, Gillett DJ, Spillane AJ. Evaluation of a breast cancer nomogram for prediction of non-sentinel lymph node positivity. Eur J Surg Oncol. 2005. 31:958–964.

12. Jeruss JS, Winchester DJ, Sener SF, Brinkmann EM, Bilimoria MM, Barrera E Jr, et al. Axillary recurrence after sentinel node biopsy. Ann Surg Oncol. 2005. 12:34–40.

13. Soni NK, Spillane AJ. Experience of sentinel node biopsy alone in early breast cancer without further axillary dissection in patients with negative sentinel node. ANZ J Surg. 2005. 75:292–299.

14. Hung WK, Chan MC, Mak KL, Chong SF, Lau Y, Ho CM, et al. Non-sentinel lymph node metastases in breast cancer patients with metastatic sentinel nodes. ANZ J Surg. 2005. 75:27–31.

15. Cao Y, Paner GP, Rajan PB. Sentinel node status and tumor characteristics: a study of 234 invasive breast carcinomas. Arch Pathol Lab Med. 2005. 129:82–84.

16. Smidt ML, Janssen CM, Kuster DM, Bruggink ED, Strobbe LJ. Axillary recurrence after a negative sentinel node biopsy for breast cancer: incidence and clinical significance. Ann Surg Oncol. 2005. 12:29–33.

17. Gui GP, Joubert DJ, Reichert R, Ward A, Lakhani S, Osin P, et al. Continued axillary sampling is unnecessary and provides no further information to sentinel node biopsy in staging breast cancer. Eur J Surg Oncol. 2005. 31:707–714.

18. Degnim AC, Reynolds C, Pantvaidya G, Zakaria S, Hoskin T, Barnes S, et al. Nonsentinel node metastasis in breast cancer patients: assessment of an existing and a new predictive nomogram. Am J Surg. 2005. 190:543–550.

19. Bergkvist L, Frisell J. Swedish Breast Cancer Group. Swedish Society of Breast Surgeons. Multicentre validation study of sentinel node biopsy for staging in breast cancer. Br J Surg. 2005. 92:1221–1224.

20. Martin RC 2nd, Chagpar A, Scoggins CR, Edwards MJ, Hagendoorn L, Stromberg AJ, et al. Clinicopathologic factors associated with false-negative sentinel lymph-node biopsy in breast cancer. Ann Surg. 2005. 241:1005–1012.

21. Veronesi U, Galimberti V, Mariani L, Gatti G, Paganelli G, Viale G, et al. Sentinel node biopsy in breast cancer: early results in 953 patients with negative sentinel node biopsy and no axillary dissection. Eur J Cancer. 2005. 41:231–237.

22. Jagsi R, Raad RA, Goldberg S, Sullivan T, Michaelson J, Powell SN, et al. Locoregional recurrence rates and prognostic factors for failure in node-negative patients treated with mastectomy: implications for postmastectomy radiation. Int J Radiat Oncol Biol Phys. 2005. 62:1035–1039.

23. Truong PT, Yong CM, Abnousi F, Lee J, Kader HA, Hayashi A, et al. Lymphovascular invasion is associated with reduced locoregional control and survival in women with node-negative breast cancer treated with mastectomy and systemic therapy. J Am Coll Surg. 2005. 200:912–921.

24. Houvenaeghel G, Nos C, Mignotte H, Classe JM, Giard S, Rouanet P, et al. Micrometastases in sentinel lymph node in a multicentric study: predictive factors of nonsentinel lymph node involvement--Groupe des Chirurgiens de la Federation des Centres de Lutte Contre le Cancer. J Clin Oncol. 2006. 24:1814–1822.

25. Rivers AK, Griffith KA, Hunt KK, Degnim AC, Sabel MS, Diehl KM, et al. Clinicopathologic features associated with having four or more metastatic axillary nodes in breast cancer patients with a positive sentinel lymph node. Ann Surg Oncol. 2006. 13:36–44.

26. Fitzal F, Riedl O, Jakesz R. Local therapy of early breast cancer. Breast Care. 2007. 2:143–148.

27. Gur AS, Unal B, Ozbek U, Ozmen V, Aydogan F, Gokgoz S, et al. Validation of breast cancer nomograms for predicting the non-sentinel lymph node metastases after a positive sentinel lymph node biopsy in a multi-center study. Eur J Surg Oncol. 2010. 36:30–35.

28. Gwak G, Park K, Shin E, Han S, Kim JY, Kim H, et al. Lymphovascular invasion and HER2/neu amplification as predictive factors for axillary lymph node metastasis in early breast cancer patients. J Breast Cancer. 2010. 13:250–256.





 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download