Abstract
Purpose
We wanted to assess the clinical efficacy of breast-specific gamma imaging (BSGI) as compared with that of conventional imaging modalities (mammography, ultrasonography and magnetic resonance imaging) as a preoperative examination for patients with breast cancer.
Methods
From April to May 2009, a retrospective review was performed for the prospectively collected 143 patients who were diagnosed with breast cancer. All the patients received a conventional imaging examination and BSGI before definitive surgery. The patients underwent BSGI with intravenous injection of 30 mCi of 99mTc-sestamibi through the contralateral antecubital vein. After 10 minutes, the craniocaudal and mediolateral oblique images were obtained. All the imaging findings were correlated with the final pathologic examination.
Results
The mean age of the patients was 49.7±9.4 years (range, 27-77). In 143 patients, 166 malignant lesions were identified by pathologic examination (invasive cancer: 96 (67.1%), ductal carcinoma in situ 14 (9.8%) and invasive cancer with carcinoma in situ 33 (23.1%). The conventional imaging modalities found 166 malignant lesions and BSGI found 156 malignant lesions. The rate of correspondence was 94.0% between the conventional imaging modalities and BSGI for malignant lesions. For BSGI, there were 4 false positive findings and 10 false negative findings. BSGI found no occult cancers that were missed by conventional imaging modality. For making the diagnosis of axillary lymph node metastasis, the sensitivity, specificity and accuracy were 33.3%, 92.1%, and 69.9% for BSGI, and 55.6%, 77.5%, and 69.2%, for ultrasonography, respectively.
Figures and Tables
 | Figure 1Malignant lesion on imaging study. (A) Breast-specific gamma imaging in left craniocaudal and left mediolateral oblique view. (B) Mammography in left craniocaudal and left mediolateral oblique view. (C) Ultrasonography. (D) Magnetic resonance imaging. Pathologic examination demonstrated 1.6 cm-sized invasive ductal carcinoma. |
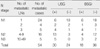
Table 3
Analysis of 10 BSGI detection-failed cases and the final pathologic results

BSGI=breast-specific gamma imaging; LVI=lymphovascular invasion; ER=estrogen receptor; PR=progesterone recepter; HER2=human epidermal growth factor receptor-2; CK=cytokeratin; EGFR=epidermal growth factor receptor; IDC=invasive ductal carcinoma; DCIS=ductal carcinoma in situ; Micropapil ca=micropapillary carcinoma.
*One metastatic lymph node; †Six metastatic lymph nodes.
References
1. Teifke A, Hlawatsch A, Beier T, Werner Vomweg T, Schadmand S, Schmidt M, et al. Undetected malignancies of the breast: dynamic contrast-enhanced MR imaging at 1.0 T. Radiology. 2002. 224:881–888.

2. Potterton AJ, Peakman DJ, Young JR. Ultrasound demonstration of small breast cancers detected by mammographic screening. Clin Radiol. 1994. 49:808–813.

3. Rosenberg RD, Hunt WC, Williamson MR, Gilliland FD, Wiest PW, Kelsey CA, et al. Effects of age, breast density, ethnicity, and estrogen replacement therapy on screening mammographic sensitivity and cancer stage at diagnosis: review of 183,134 screening mammograms in Albuquerque, New Mexico. Radiology. 1998. 209:511–518.

4. Kolb TM, Lichy J, Newhouse JH. Comparison of the performance of screening mammography, physical examination, and breast US and evaluation of factors that influence them: an analysis of 27,825 patient evaluations. Radiology. 2002. 225:165–175.

5. Berg WA, Gutierrez L, NessAiver MS, Carter WB, Bhargavan M, Lewis RS, et al. Diagnostic accuracy of mammography, clinical examination, US, and MR imaging in preoperative assessment of breast cancer. Radiology. 2004. 233:830–849.

6. Yang WT, Ahuja A, Tang A, Suen M, King W, Metreweli C. High resolution sonographic detection of axillary lymph node metastases in breast cancer. J Ultrasound Med. 1996. 15:241–246.

7. Rajesh YS, Ellenbogen S, Banerjee B. Preoperative axillary ultrasound scan: its accuracy in assessing the axillary nodal status in carcinoma breast. Breast. 2002. 11:49–52.

8. Cowher MS, Erb KM, Poller W, Julian TB. Correlation of the use of axillary ultrasound and lymph node needle biopsy with surgical lymph node pathology in patients with invasive breast cancer. Am J Surg. 2008. 196:756–759.

9. Khalkhali I, Mena I, Jouanne E, Diggles L, Venegas R, Block J, et al. Prone scintimammography in patients with suspicion of carcinoma of the breast. J Am Coll Surg. 1994. 178:491–497.
10. Sharma S, Sharma MC, Sarkar C. Morphology of angiogenesis in human cancer: a conceptual overview, histoprognostic perspective and significance of neoangiogenesis. Histopathology. 2005. 46:481–489.

11. Delmon-Moingeon LI, Piwnica-Worms D, Van den Abbeele AD, Holman BL, Davison A, Jones AG. Uptake of the cation hexakis(2-methoxyisobutylisonitrile)-technetium-99m by human carcinoma cell lines in vitro. Cancer Res. 1990. 50:2198–2202.
12. Brem RF, Petrovitch I, Rapelyea JA, Young H, Teal C, Kelly T. Breast-specific gamma imaging with 99mTc-Sestamibi and magnetic resonance imaging in the diagnosis of breast cancer--a comparative study. Breast J. 2007. 13:465–469.

13. Brem RF, Floerke AC, Rapelyea JA, Teal C, Kelly T, Mathur V. Breast-specific gamma imaging as an adjunct imaging modality for the diagnosis of breast cancer. Radiology. 2008. 247:651–657.

14. Tolmos J, Khalkhali I, Vargas H, Stuntz M, Cutrone J, Mishkin F, et al. Detection of axillary lymph node metastasis of breast carcinoma with technetium-99m sestamibi scintimammography. Am Surg. 1997. 63:850–853.
15. Taillefer R, Robidoux A, Turpin S, Lambert R, Cantin J, Leveille J. Metastatic axillary lymph node technetium-99m-MIBI imaging in primary breast cancer. J Nucl Med. 1998. 39:459–464.
16. Danielsson R, Bone B, Perbeck L, Aspelin P. Evaluation of planar scintimammography with 99mTc-MIBI in the detection of axillary lymph node metastases of breast carcinoma. Acta Radiol. 1999. 40:491–495.

17. Lumachi F, Tregnaghi A, Ferretti G, Povolato M, Marzola MC, Zucchetta P, et al. Accuracy of ultrasonography and 99mTc-sestamibi scintimammography for assessing axillary lymph node status in breast cancer patients. A prospective study. Eur J Surg Oncol. 2006. 32:933–936.

18. Lumachi F, Ferretti G, Povolato M, Bui F, Cecchin D, Marzola MC, et al. Axillary lymph node metastases detection with 99mTc-sestamibi scintimammography in patients with breast cancer undergoing curative surgery. Anticancer Res. 2007. 27:2949–2952.
19. Massardo T, Alonso O, Llamas-Ollier A, Kabasakal L, Ravishankar U, Morales R, et al. Planar Tc99m-sestamibi scintimammography should be considered cautiously in the axillary evaluation of breast cancer protocols: results of an international multicenter trial. BMC Nucl Med. 2005. 5:4.

20. Maublant J, de Latour M, Mestas D, Clemenson A, Charrier S, Feillel V, et al. Technetium-99m-sestamibi uptake in breast tumor and associated lymph nodes. J Nucl Med. 1996. 37:922–925.
21. Brem RF, Rapelyea JA, Zisman G, Mohtashemi K, Raub J, Teal CB, et al. Occult breast cancer: scintimammography with high-resolution breast-specific gamma camera in women at high risk for breast cancer. Radiology. 2005. 237:274–280.

22. Arslan N, Ozturk E, Ilgan S, Urhan M, Karacalioglu O, Pekcan M, et al. 99Tcm-MIBI scintimammography in the evaluation of breast lesions and axillary involvement: a comparison with mammography and histopathological diagnosis. Nucl Med Commun. 1999. 20:317–325.
23. Tillman GF, Orel SG, Schnall MD, Schultz DJ, Tan JE, Solin LJ. Effect of breast magnetic resonance imaging on the clinical management of women with early-stage breast carcinoma. J Clin Oncol. 2002. 20:3413–3423.

24. Lehman CD, Gatsonis C, Kuhl CK, Hendrick RE, Pisano ED, Hanna L, et al. MRI evaluation of the contralateral breast in women with recently diagnosed breast cancer. N Engl J Med. 2007. 356:1295–1303.

25. Bilimoria KY, Cambic A, Hansen NM, Bethke KP. Evaluating the impact of preoperative breast magnetic resonance imaging on the surgical management of newly diagnosed breast cancers. Arch Surg. 2007. 142:441–445.





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download