Abstract
Purpose
Invasive micropapillary carcinoma (IMPC) of the breast is a rare and associated with high incidence of lymph node metastasis and poor outcome. The aims of this study were to provide a comprehensive analysis of clinicopathologic and immunohistochemical characteristics of IMPC and to elucidate the differences between IMPC and invasive ductal carcinoma (IDC).
Methods
Sixty-one patients of IMPC were identified by retrospective review of database from January 2004 to December 2008. 221 patients were randomly selected among the IDC patients who received operation during the same period. Two groups were compared with uni- and multivariate analysis.
Results
We observed significant differences in mean number of metastatic lymph nodes (6.1 vs. 1.9, p=0.001), positivity of lymph node (70.5% vs. 45.2%, p<0.001), and presence of lymphatic vessel invasion (75.4% vs. 34.8%, p<0.001) between IMPC and IDC patients. Although it has been known that triple negative breast cancer (TNBC) have lymphotropic tendency in their early T stage, 11.8% (26/221) of IDC and 3.3% (2/61) of IMPC patients were TNBC in this study (p=0.050). In multivariate analysis, IMPC histology showed no correlation with disease-free survival (DFS) and the lymphatic vessel invasion was a significant predictor of DFS.
Conclusion
The results of this study confirm that IMPC is unique subtype of breast cancer that is commonly accompanied by axillary lymph node metastasis and shows poor outcome, although it rarely presents the pattern of TNBC. Lymphatic vessel invasion rather than histology of IMPC seems to be more closely related to DFS.
Invasive micropapillary carcinoma (IMPC) of the breast is a rare and distinct subtype of breast cancer.(1) In 1993, Siriaunkgul and Tavassoli(1) defined histologic features of IMPC and it was newly listed in the World Health Organization classification of the breast cancer in 2003. Recently, some papers on IMPC have been published and most authors suggested that IMPC showed more aggressive characteristics than invasive ductal carcinoma (IDC).(2-5) According to these studies, axillary lymph node metastasis, lymphatic vessel invasion, high histologic grade, and overexpression of estrogen receptor (ER) were distinct behavior of IMPC compared with IDC.(3-8)
However, there were some differences in clinicopathologic and immunohistochemical results of IMPC although many agreements have been reached. In particular, lymphotropic feature (lymph node metastasis and lymphatic vessel invasion) was observed in most of the studies, but as for hormonal receptors and biologic marker (e.g., p53 and HER2), there have been some disagreements,(3-8) which may be due to insufficient data to date. It has been reported that triple negative breast cancer (TNBC, ER-/PR-/HER2-) patients have a high rate of lymph node positivity,(9) and therefore we assumed that IMPC would be associated with TNBC.
The objective of this study was to provide a comprehensive analysis of clinicopathologic and immunohistochemical characteristics of IMPC of breast and to recognize the differences between IMPC and IDC. We also attempted to verify the co-relation between IMPC and TNBC.
Sixty-one cases of IMPC of breast were identified by retrospective review of 3,452 patients with IDC who received operation from January 2004 to December 2008 at Samsung Medical Center. To be included in this study, tumors had to have a predominant (>75%) invasive micropapillary pattern; we excluded cases that showed a minor invasive micropapillary pattern. The primary hypothesis of this study is that there is difference in the number of metastatic lymph node between IMPC and IDC patients. Based on the calculation that the standard deviation of the number of metastatic lymph node is 8.22(3) and the size of IMPC is 61 patients, a total of 221 IDC patients would provide the power of 0.9, under the significance level 0.05, to detect the significant difference of at least 4 metastatic lymph node between the two groups with nonparametric method. So, we randomly selected 221 patients with IDC among 3,391 IDC patients as control group using "Rand" and "Int", a functional formula of Microsoft Excel®.
We collected the data from electronic medical records about age, sex, operation type, tumor size, lymph node metastasis, presence of lymphatic vessel invasion, histological grade, nuclear grade, hormonal receptor status, HER2, p53, and recurrence.
The breast cancer stage was adopted from the sixth edition of the AJCC cancer staging.(10) The histologic grade was evaluated using the modified Bloom-Richardson scoring system.(11) Cases were considered positive for ER or PR if nuclear staining was present in at least 10% of the tumor cells tested. Moderate (2+) or strong (3+) membranous staining in at least 50% of the tumor cells was required for a case to be considered positive for HER2. Patients with negative ER, PR, and HER2 were defined triple negative breast cancer (TNBC).
Survival analysis end points included disease-free survival (DFS), defined as time to disease recurrence (local recurrence, recurrence in the opposite breast, or distant organ metastasis), but disease-specific survival was not included because of relative short follow-up duration.
For statistical analysis, SPSS version 17.0 (SPSS Inc., Chicago, USA) was used. Categorical variables and numerical variables were analyzed with chi-squared test (Fisher's exact test when appropriate) and Student's t-test, respectively. Cox proportional hazard model was implemented for univariate and multivariate analysis. p-value of <0.05 was considered statistically significant.
Tumors diagnosed as IMPC comprised 1.7% of the reviewed breast carcinomas. Only one patient was male among IMPC patients. There were no statistical differences in mean age and mean tumor size between IMPC and IDC patients. Four types of operation were performed: modified radical mastectomy (MRM), breast conserving surgery (BCS), partial mastectomy with sentinel lymph node biopsy (PM+SLN), and total mastectomy with sentinel lymph node biopsy (TM+SLN). There were no statistically significant differences among the operations performed (p=0.003). Mean follow up periods of IMPC and IDC patients were 38.6 and 34.9 months, respectively. Recurrence rate during follow-up recurrence was 13.1% and 5.4% for IMPC and IDC patients, respectively (p=0.049). Recurrence occurred sooner in IMPC patients than in IDC patients, but there was no significant difference between them (p=0.667).
Mean number of metastatic lymph node of IMPC and IDC were 6.1 and 1.9, respectively (p=0.001). Forty-three (70.5%) of 61 IMPC and 100 (45.2%) of 221 IDC patients had metastatic lymph node (p<0.001); 46 (75.4%) and 77 (34.8%) patients with IMPC and IDC, respectively, appeared to have lymphatic vessel invasion and it was statistically significant (p<0.001).
When histologic results of IMPC were classified using the modified Bloom-Richardson scoring system, 41.0%, 55.7%, and 3.3% IMPC patients could be classified as poorly differentiated, moderately differentiated, and well differentiated, respectively. When the scoring system was applied to the IDC patients, 20.4%, 46.2%, and 33.5% could be categorized as well differentiated, moderately differentiated, and poorly differentiated IDC, respectively (p=0.007) (Table 1).
In the T stage, there was no statistical difference between IMPC and IDC patients (p=0.831). In the N stage, 52.6% of IDC patients were N0 and only 5.0% were N3, but IMPC patients were quite evenly distributed from N0 to N3 (29.5, 26.2, 23.0, and 21.3%), which was statistically significant (p<0.001). TNM stage between the two groups was also statistically different (p<0.001) (Table 1).
At T1 stage, 60.0 and 73.3% of IMPC patients show lymph node metastasis and lymphatic vessel invasion, but IDC patients show lower percentage of involvement than IMPC (p=0.001 and p<0.001). There was a trend that the higher T stage, the more metastatic lymph node and lymphatic vessel invasion (Table 2).
The percentage of expression of ER, PR, and HER-2 were higher in IMPC than in IDC although there were no statistical differences (p=0.234, 0.229, and 0.105). Only expression of p53 was higher in IDC than in IMPC (p=0.012).
Twenty-six (11.8%) patients of IDC were TNBC, but in IMPC patients, only 2 (3.3%) patients were TNBC (p=0.05) (Table 1).
Factors univariately associated with recurrence are listed in Table 3. The major factors associated with poor outcome in these analyses were IMPC pathology, lymph node metastasis, and lymphatic vessel invasion.
IMPC histology showed no correlation with DFS in multivariate analysis. Only lymphatic vessel invasion was significant predictor of DFS (Table 4).
In our study, axillary lymph node metastasis and lymphatic vessel invasion were more frequently observed in IMPC than in IDC. And percentage of triple negative was higher in IDC than in IMPC, but IMPC showed worse prognosis than IDC. IMPC pathology, lymph node metastasis, and lymphatic vessel invasion were factors significantly associated with disease-free survival in univariate analysis, but IMPC pathology showed no correlation with DFS in multivariate analysis. Invasive papillary carcinoma of the breast is often confused with IMPC pathologically. While invasive papillary carcinoma shows a complex arborescent growth pattern within duct-like spaces,(12) IMPC is composed of small clusters of tumor cells within the clear stromal spaces which are not epithelium lined (Figure 1).
Results of the present study correspond with that of the majority of earlier studies(2,6-8,13-15) which reported that IMPC showed more lymphotropic features (lymph node metastasis and lymphatic vessel invasion) than IDC not only in T2 and T3 but also in T1. These findings are in close association with poor outcome of IMPC and are most distinguishing characteristics of IMPC from IDC. In IMPC patients, much higher percentage of operations included axillary dissection (MRM and BCS) than in IDC. This finding doesn't seem to have been the result of current study design, in which IDC patients have been randomly selected, but to the lymphotropic nature of IMPC.
In previous studies,(2,4,5) estrogen and progesterone receptors were shown to be more overexpressed in IMPC than IDC, but there were no differences between IMPC and IDC in our results. And as for p53, which is a tumor suppressor gene product associated with recurrence and decreased survival in patients with advanced breast cancer,(16) results have been conflicting since in some studies, p53 was shown to be more overexpressed in IDC than in IMPC,(6,8) Further study is needed to clarify this discrepancy.
It is known that so called triple negative breast cancer (TNBC, ER-/PR-/HER2-) is unresponsive to hormonal therapies and results in poor outcome and tends to have lymph node metastasis even in early T stage.(17-19) In contrast to the assumption that TNBC is more common in IMPC than in IDC, TNBC was more frequently found in IDC than in IMPC (11.8% vs. 3.3%, p=0.05) in this study. The reason why IMPC carries worse prognosis than IDC can be explained better by lymphotropic characteristic of IMPC, which proved to be significant predictor of DFS in our study, than by characteristics of TNBC.
In line with the previous study, which reported that IMPC histology was not related to the breast cancer recurrences,(3) IMPC histology was not an independent factor which could predict local recurrence as well as distant organ metastasis in this study. A large-scaled prospective study is warranted to clarify this finding in the future.
The results of this study confirm that IMPC is a unique subtype of breast cancer. Axillary lymph node metastasis and lymphatic vessel invasion is common in IMPC and related to poor outcome although IMPC itself rarely has the pattern of TNBC. Careful consideration is needed when evaluating the axilla of IMPC patients since lymphatic vessel invasion rather than the histology of IMPC seems to be more closely associated with DFS.
Figures and Tables
Figure 1
Invasive micropapillary carcinoma of the breast. Photomicrograph reveals carcinoma composed of small clusters of tumor cells within the clear stromal spaces (H&E stain, ×100).
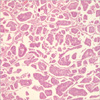
Table 1
Clinicopathologic characteristics of IMPC and IDC patients

IMPC=invasive micropapillary carcinoma, IDC=invasive ductal carcinoma; SD=standard deviation; LN=lymph node; MRM=modified radical mastectomy; BCS=breast conserving surgery; PM+SLN=partial mastectomy with sentinel lymph node biopsy; TM+SLN=total mastectomy with sentinel lymph node biopsy; ER=estrogen receptor; PR=progesterone receptor.
*p<0.05.
References
1. Siriaunkgul S, Tavassoli FA. Invasive micropapillary carcinoma of the breast. Mod Pathol. 1993. 6:660–662.
2. Zekioglu O, Erhan Y, Ciris M, Bayramoglu H, Ozdemir N. Invasive micropapillary carcinoma of the breast: high incidence of lymph node metastasis with extranodal extension and its immunohistochemical profile compared with invasive ductal carcinoma. Histopathology. 2004. 44:18–23.

3. Paterakos M, Watkin WG, Edgerton SM, Moore DH 2nd, Thor AD. Invasive micropapillary carcinoma of the breast: a prognostic study. Hum Pathol. 1999. 30:1459–1463.
4. Nassar H, Wallis T, Andea A, Dey J, Adsay V, Visscher D. Clinicopathologic analysis of invasive micropapillary differentiation in breast carcinoma. Mod Pathol. 2001. 14:836–841.

5. Walsh MM, Bleiweiss IJ. Invasive micropapillary carcinoma of the breast: eighty cases of an underrecognized entity. Hum Pathol. 2001. 32:583–589.

6. Kim MJ, Gong G, Joo HJ, Ahn SH, Ro JY. Immunohistochemical and clinicopathologic characteristics of invasive ductal carcinoma of breast with micropapillary carcinoma component. Arch Pathol Lab Med. 2005. 129:1277–1282.

7. Luna-More S, Casquero S, Perez-Mellado A, Rius F, Weill B, Gornemann I. Importance of estrogen receptors for the behavior of invasive micropapillary carcinoma of the breast. Review of 68 cases with follow-up of 54. Pathol Res Pract. 2000. 196:35–39.

8. Pettinato G, Manivel CJ, Panico L, Sparano L, Petrella G. Invasive micropapillary carcinoma of the breast: clinicopathologic study of 62 cases of a poorly recognized variant with highly aggressive behavior. Am J Clin Pathol. 2004. 121:857–866.
9. Dent R, Trudeau M, Pritchard KI, Hanna WM, Kahn HK, Sawka CA, et al. Triple-negative breast cancer: clinical features and patterns of recurrence. Clin Cancer Res. 2007. 13:4429–4434.

10. Singletary SE, Connolly JL. Breast cancer staging: working with the sixth edition of the AJCC Cancer Staging Manual. CA Cancer J Clin. 2006. 56:37–47.

11. Elston CW, Ellis IO. Pathological prognostic factors in breast cancer. I. The value of histological grade in breast cancer: experience from a large study with long-term follow-up. Histopathology. 1991. 19:403–410.

12. Fisher ER, Palekar AS, Redmond C, Barton B, Fisher B. Pathologic findings from the National Surgical Adjuvant Breast Project (protocol no. 4). VI. Invasive papillary cancer. Am J Clin Pathol. 1980. 73:313–322.

13. Yu JH, Kim SW, Han WS, Kim SW, Park IA, Youn YK, et al. Micropapillary carcinoma of breast. J Korean Breast Cancer Soc. 2004. 7:132–135.

14. Luna-More S, Gonzalez B, Acedo C, Rodrigo I, Luna C. Invasive micropapillary carcinoma of the breast. A new special type of invasive mammary carcinoma. Pathol Res Pract. 1994. 190:668–674.
15. Middleton LP, Tressera F, Sobel ME, Bryant BR, Alburquerque A, Grases P, et al. Infiltrating micropapillary carcinoma of the breast. Mod Pathol. 1999. 12:499–504.
16. Beck T, Weller EE, Weikel W, Brumm C, Wilkens C, Knapstein PG. Usefulness of immunohistochemical staining for p53 in the prognosis of breast carcinomas: correlations with established prognosis parameters and with the proliferation marker, MIB-1. Gynecol Oncol. 1995. 57:96–104.

17. Haffty BG, Yang Q, Reiss M, Kearney T, Higgins SA, Weidhaas J, et al. Locoregional relapse and distant metastasis in conservatively managed triple negative early-stage breast cancer. J Clin Oncol. 2006. 24:5652–5657.





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download