Abstract
Purpose
The final purpose of post mastectomy reconstruction is a balanced, symmetrical, pleasing appearance for both breasts. However, in cases where women have an unattractive breast, which may be small, ptotic or huge, remodeling of the contralateral breast may be desirable. Surgical options available for the contralateral breast included breast augmentation using implants, mastopexy, and reduction mammoplasty.
Methods
All patients who underwent unilateral breast reconstruction at Kyungpook National University Hospital from September of 2006 to February of 2008 were included in this study. The methods of reconstruction included transverse rectus abdominis musculocutaneous flap, latissimus dorsi flap, and the use of implants. Contralateral procedures to achieve symmetry included augmentation, mastopexy, and reduction.
Results
A total of 57 patients were evaluated, including 45 immediate, and 12 delayed reconstructions. Twenty-six of these patients underwent contralateral breast management (augmentation [12], mastopexy [11], and reduction [3]). The average age was 44.9 years and the mean follow up interval was 13 months. Most of the patients were satisfied with the symmetry, clothed appearance, nude appearance, aesthetics, and consistency. Sixty-six percent (8 of 12) of delayed reconstruction patients had a symmetry procedure performed on the opposite breast, compared with 40 percent (18 of 45) of the immediate-reconstruction patients. No complications were observed on the contralateral breasts undergoing symmetrization.
Conclusion
Contralateral management in breast reconstruction can provide symmetry with the reconstructed breast contour and aesthetically satisfactory results in a safe manner. Immediate symmetrization procedure also can avoid secondary operations and offer psychological benefits without delaying adjuvant therapy.
A balanced, symmetrical, pleasing appearance for both breasts has been the final objective of post-mastectomy reconstruction. When reconstruction has been considered, an equal level of importance should be placed on the contralateral breast. If the contralateral breast was not appropriately sized or shaped, remodeling of the contralateral breast to achieve optimal results has been indicated. The need for a symmetry procedure on the opposite breast often depends on the patient's premastectomy characteristics, surgeon's preference, post-reconstruction desires, type of mastectomy, and reconstruction method used. Numerous options may be available to the patient depending upon the individual anatomic and oncologic status for symmetrical shape. Surgical options available for the contralateral breast has included breast augmentation with implant, mastopexy, and reduction mammoplasty.(1-14)
On consultation with a plastic surgeon, options for the contralateral breast should be presented to the patient. After ruling out any associated pathology and completing a diagnosis regarding the outline of the concerned breast, the patient and the physician should together to decide on whether to pursue augmentation, mastopexy, or reduction.
The purpose of this study was to provide information on contralateral breast management in Korean females by presenting the experience at Kyungpook National University Hospital in this field and to compare breast reconstruction in combination with contralateral breast mammoplasty with breast reconstruction alone. The results suggest that contralateral management in breast reconstruction can provide symmetry with the reconstructed breast contour and aesthetically satisfactory result in a safe manner.
All patients who underwent unilateral breast reconstruction at Kyungpook National University Hospital from September of 2006 to February of 2008 were included in the study. The patients were stratified by reconstruction timing, method of reconstruction, and type of contralateral breast procedure. The various methods of reconstruction included pedicled transverse rectus abdominis musculocutaneous (TRAM) flap, latissimus dorsi (LD) flap, and the use of implants. The contralateral lateral breast procedures to achieve symmetry included augmentation, mastopexy, and reduction. Augmentation was performed using smooth type saline or cohesive gel implants. Implants were routinely placed in the submuscular area by transaxillary or periareolar incision. Vertical mastopexy was mainly used for ptotic breasts, and periareolar mastopexy was performed in selected cases. In order to obtain a better long term outcome, the inferior thoracic based flap was elevated and fixed to the pectoralis fascia for maintenance of upper pole fullness (Figure 1).(15) Wise pattern reduction mammoplasty or vertical mammaplasty was done for large breast.
To compare the breast symmetry procedure with breast reconstruction alone, we assessed patients'satisfaction through the use of a questionnaire including symmetry, clothed appearance, nude appearance, aesthetic, and consistency. Scoring systems were used for each item and assessments of patients were categorized based on the following: "Good" (6-7), "Fair" (3-5), and "Poor" (0-2).(16)
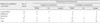
A total of 57 patients underwent unilateral breast reconstruction at Kyungpook National University Hospital from September of 2006 to February of 2008. Twenty-six of these patients underwent contralateral breast management. Contralateral procedures included augmentation (12), mastopexy (11) (vertical [8] and periareola [3]) and reduction (3) (wise pattern [2], vertical [1]) of the contralateral breast (Table 1). The average age was 44.9 yr and the mean follow up interval was 13 months. The relation between breast reconstruction and contralateral breast procedure were as follows.
Of 57 patients, 40 underwent total mastectomy with or without axillary lymph node dissection (Stage 0, n=4; Stage I, n=9; Stage II, n=23; Stage III, n=4), 13 underwent skin sparing mastectomy (phyllodes tumor, n=1; Stage I, n=8; Stage II, n=3; Stage III, n=1) and 4 underwent nipple sparing mastectomy (giant fibroadenoma, n=4). In this study, immediate breast reconstruction did not lead to a delay in the delivery of adjuvant chemotherapy and did not adversely affect breast cancer outcome.
The 57 patients were divided into 45 immediate reconstructions and 12 delayed reconstructions. Sixty-six percent (8 of 12) of delayed reconstruction patients had a symmetry procedure performed on the opposite breast, compared with 40 percent (18 of 45) of the immediatere-construction patients. The most likely symmetry procedure performed in delayed reconstructions was augmentation mammoplasty (3 of 8 or 38 percent) and that of immediate reconstructions was mastopexy (8 of 18 or 44 percent).
The 57 patients were stratified into three groups with respect to the methods of reconstruction: TRAM, LD, and implant. TRAM flap reconstruction accounted for 54 percent (31 of 57), LD flap reconstruction occupied 12 percent (7 of 57), and 33 percent (19 of 57) underwent implant reconstruction.
Symmetry procedures stratified by method of reconstruction have been depicted. Results indicate that TRAM flap reconstruction required a symmetry procedure in 52 percent of patients (16 of 31), with augmentation being the most common (8 of 16 or 50 percent). Further, LD flap reconstruction required a symmetry procedure in only 29 percent (2 of 7) and all procedures were augmentation. Reconstructions involving an implant required a symmetry procedure in 42 percent of the patients (8 of 19), with mastopexy being the most common procedure (4 of 8 or 50 percent).
The type of symmetry procedure was most likely to involve augmentation in the TRAM reconstruction group for both delayed (3 of 6 or 50 percent) and immediate (5 of 10 or 50 percent) reconstruction.
To assess patients'satisfaction, the 57 patients were divided into two groups: breast reconstruction and a contralateral procedure, and breast reconstruction only. Each group completed a questionnaire which consisted of five parameters: symmetry, clothed appearance, nude appearance, aesthetic appearance and consistency. The contralateral procedure group was assessed as having a more "Good" satisfaction outcome compared with the breast reconstruction only group (Figure 2).
There were four cases of fat necrosis characterized by subcutaneous firmness larger than 2 cm in diameter, one partial flap loss, one hernia in the TRAM reconstructions and one seroma in the LD flap reconstructions. Further, two capsular contractures and one skin necrosis at the junction of the inverted 'T' closure flaps were observed in the implant reconstructions. However, these complications were treated by simple revisions or conservative therapy and did not influence for additional treatment of cancer. No complications were observed on the contralateral breasts that had been subjected to symmetrization (Table 2).
The goals of unilateral breast reconstruction are: 1) to restore a comfortable, pleasing breast contour, 2) to restore a natural looking nipple-areola complex, and 3) to provide symmetry between the reconstructed breast and remaining normal breast. The third goal forms the basis for the decisions that need to be made with regard to contralateral breast management. The objective for management of the contralateral breast in post mastectomy reconstruction has been to provide symmetry with the reconstructed breast contours. Therefore, evaluation and treatment of the contralateral breast has been a very important component of the reconstructive process.
In cases when the unaffected breast has been aesthetically pleasing and there has been low risk of breast cancer in the contralateral breast, matching to the remaining breast has been selected as the best choice. This is also important if the patient prefers the healthy breast to be untouched. Breast augmentation may be necessary on the opposite breast to correct either pure hypoplasia or slight ptosis. Breast reconstruction to duplicate very small hypoplastic breast is somewhat challenging. In this study, contralateral breast augmentation was most commonly required when the breast had been reconstructed by using a distant flap such as a TRAM flap (Figure 3).
In cases when the remaining breast has been ptotic, symmetry has been accomplished either by breast augmentation in the case of mild ptosis, or by mastopexy for moderate to severe ptosis. If patient, with a ptotic breast, chooses implant reconstruction, it can be difficult to achieve ptosis using an implant and it has been more likely to achieve the desired symmetry using mastopexy of contralateral breast (Figure 4).
Both periareolar mastopexy and vertical mastopexy have been used for correction of mild to modrate ptosis. In cases of less projected original breast or large areola, periareolar mastopexy has been appropriate and in cases of short inframammary fold to nipple distance, vertical mastectomy have been suitable. Inverted T type mastopexy has been preferable for patients who need nipple areolar complex elevation more than 6 cm due to severe ptosis,. In this study, vertical mastopexy was mainly used for ptotic breast whereas periareolar mastopexy was performed in selected cases when patients had mild ptosis or wanted to conceal a scar. If the contralateral breast was larger than the resultant reconstructed breast, reduction mammoplasty can be performed on the remaining natural breast (Figure 5).
The breast size and shape are not the only factors that must be considered. In this study, contralateral breast surgery was performed in just 66 percent of delayed reconstruction patients and in 40 percent of immediate reconstruction patients. These percentages are influenced by a patients' decision as to whether or not a heathy breast should undergo surgery for aesthetic reasons. Additionally, the consideration to operate on the contralateral breast in unilateral breast reconstruction is complex and multifactorial. The patient's concept and image of her breast, a surgeon's preference and skill, and social conceptual background about the breast inevitably influences whether a symmetry procedure is needed and all must be considered preoperatively. There are several reports which have provided information about the contralateral breast management. Dinner and Dowden(2) reported that an operative procedure to improve the appearance of the opposite breast has been indicated in as many as 80 percent of unilateral breast reconstruction patients. In a large series, which was reported by Losken et al.,(3) involving 1,394 patients who underwent postmastectomy breast reconstruction with TRAM flaps, LD flaps, and implants, 67 percent of delayed reconstruction patients and 22 percent of immediate reconstruction patients were reported to require a symmetry procedure on the opposite breast. Prosthetic reconstruction resulted in a higher incidence of contralateral operation, breast reduction was the most common procedure after autologous reconstruction and augmentation mammoplasty was most common after prosthetic reconstruction in this series.
Recently, Nahabedian described a study involving 665 patients who underwent unilateral breast reconstructions. Among them, a contralateral operation was performed in 17% (n=111) and occurred with greater frequency in the delayed reconstruction group. The most common contralateral procedure was reduction mammaplasty.(4) In one oriental group, however, contralateral breast augmentation was most commonly performed as a symmetry procedure because of thin and slender body habitus of the patients.(5) Similarly, Korean women are thin with a slender body habitus. Therefore, in this study, contralateral breast augmentation was the procedure most commonly applied for hypoplastic breasts (46 percent). The advantage of implant replacement as the contralateral breast procedure in Korean women include: 1) perioperatively, the contralateral breast can serve as a model for adjusting the shape and volume of the breast that needs reconstruction, 2) it does not interfere with adjuvant therapy, and 3) it can provide not only symmetrical breasts but also aesthetically improved breasts.
A procedure on the opposite breast can be performed at the same time as breast reconstruction or can be delayed for several months. The ideal time at which to perform the symmetry procedure remains controversial; however, several studies postulated that superior aesthetic results can be achieved when the symmetry procedure is carried out during the initial reconstruction, because the corrected opposite side can be used as a standard for breast reconstruction. Furthermore, it has been advocated that the primary symmetrization procedure offers an opportunity for glandular exploration for occult carcinomas in the contralateral breast.(6) In contrast, some authors prefer to adjust the contralateral breast at a later stage, after completion of any adjuvant therapy. This may be due to the fact that alterations in the shape, size, and consistency of the reconstructed mound occur within the first 3-6 months postoperatively.
For this reason, a more accurate assessment of the rearrangement of the contralateral breast can be performed after these changes have occurred. When the contralateral procedure is delayed, is allows for it to be performed together with the reconstruction of the nipple-areola complex and with whatever alterations are required on the reconstructed mound.
There are advantages to simultaneous breast reconstruction and contralateral breast management. When these operations are performed together, the patient experiences less recuperative time and duration of discomfort. Additionally, a one-stage procedure may be more cost-effective and may positively affect a patient's well-being. Also, simultaneous correction of body contouring offers significant psychological benefits to the patient and improved aesthetic results without delaying adjuvant therapy or negatively impacting patient's outcome.
Contralateral management in breast reconstruction can provide symmetry with the reconstructed breast contour and aesthetically satisfactory results in a safe manner. Additionally, immediate symmetrization procedures can avoid secondary operations and offer psychological benefits without delaying adjuvant therapy.
Figures and Tables
 | Figure 1A vertical mastopexy for ptotic breast. (A) After deepithelization. (B) Pillars pulled together with inverted sutures. (C) Immediate postoperative view. (D) When both correction of ptosis and projection were needed, the inferior thoracic-based flap of the breast was transposed underneath and fixed to the pectoralis fascia for added projection. |
 | Figure 2Satisfaction rate. The subjective analysis of results by patients indicated satisfaction with the combined procedure. Contralateral procedure group (A). Ipsilateral breast reconstruction only group (B). |
 | Figure 3(A, B) A 36-year-old woman with cancer of the left breast. (C, D) The same patient after skin sparing mastectomy. Immediate TRAM flap reconstruction and augmentation on contralateral breast were performed. Results 12 months postoperatively. |
 | Figure 4(A, B) A 36-year-old woman with cancer of the right breast. (C, D) The same patient after skin sparing mastectomy. Immediate breast reconstruction with a silicone implant and periareolar mastopexy on the contralateral breast were performed. Results 14 months postoperatively. |
 | Figure 5(A, B) A 47-year-old woman with cancer of the left breast. (C, D) The same patient after delayed TRAM flap reconstruction and vertical reduction on the contralateral breast. Results 13 months postoperatively. |
References
1. Hartrampf CR, Scheflan M, Black PW. Breast reconstruction with a transverse abdominal island flap. Plast Reconstr Surg. 1982. 69:216–225.

2. Dinner MI, Dowden RV. Gant TD, Vasconez LO, editors. Management of the contralateral breast. Postmastectomy Reconstruction. 1988. 2nd ed. Baltimore: Williams & Wilkins;205–217.
3. Losken A, Carlson GW, Bostwick J 3rd, Jones GE, Culbertson JH, Schoemann M. Trends in unilateral breast reconstruction and management of the contralateral breast: The Emory experience. Plast Reconstr Surg. 2002. 110:89–97.

4. Nahabedian MY. Managing the opposite breast: contralateral symmetry procedures. Cancer J. 2008. 14:258–263.

5. Ulusal BG, Cheng MH, Wei FC. Simultaneous endoscopic-assisted contralateral breast augmentation with implants in patients undergoing postmastectomy breast reconstruction with abdominal flaps. Plast Reconstr Surg. 2006. 118:1293–1302.

6. Petit JY, Rietjens M, Contesso G, Bertin F, Gilles R. Contralateral mastoplasty for breast reconstruction: a good opportunity for glandular exploration and occult carcinomas diagnosis. Ann Surg Oncol. 1997. 4:511–515.

7. Miller MJ, Rock CS, Robb GL. Aesthetic breast reconstruction using a combination of free transverse rectus abdominis musculocutaneous flaps and breast implants. Ann Plast Surg. 1996. 37:258–264.

8. Serletti JM, Moran SL. The combined use of the TRAM and expanders/implants in breast reconstruction. Ann Plast Surg. 1998. 40:510–514.

9. Stevenson TR, Goldstein JA. TRAM flap breast reconstruction and contralateral reduction of mastopexy. Plast Reconstr Surg. 1993. 92:228–233.

10. Lejour M, Jabri M, Deraemaecker R. Analysis of long-term results of 326 breast reconstructions. Clin Plast Surg. 1988. 15:689–701.

11. Restifo RJ. TRAM revisions and contralateral mammaplasties: the role of "mirror image" skin patterns. Semin Plast Surg. 2004. 18:245–253.

12. Chen JS. Simultaneous TRAM flaps with contralateral augmentation mammaplasty in breast reconstruction. ANZ J Surg. 2003. 73:A238.
13. VanderKam VM, Achauer BM. Breast reconstruction: the contralateral breast. Plast Surg Nurs. 1996. 16:197–198. 196
14. Murillo WL. Contralateral breast management in breast reconstruction. Semin Plast Surg. 2002. 16:77–91.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download