Abstract
Purpose
To reduce the side effects and improve the effectiveness of standard chemoradiation therapy, many complementary or alternative medicines have been tried. However, little is known about its immunologic effects in breast cancer patients. The aim of this study was to assess the immunologic effects of mistletoe extract (Viscum album L., VAE) in patients with early breast cancer after surgery followed by standard adjuvant chemoradiation therapy.
Methods
A total 20 patients with early breast cancer treated with breast conserving surgery followed conventional chemoradiation therapy. Ten of these patients received subcutaneous injections of VAE for 7 weeks. IL-2, IL-4, IL-6, IL-10, TGF-β, and IFN-γ levels in serum samples were measured in all patients.
Results
The concentrations of IL-2, IL-4, IL-10, and TGF-β were not significantly changed between before and after VAE treatment in both test and control group. The concentration of IL-6 in the test group was increased from 8.19±1.75 pg/mL to 9.86±1.46 pg/mL after treatment (p=0.013). The concentration of IFN-γ in the test group was remarkably increased from 91.76±17.16 pg/mL to 167.42±66.61 pg/mL after treatment (p=0.009).
During treatment of cancer, some side effects of conventional treatment may limit the ability of the patient to receive the full course of therapy. To reduce the side effects and improve the effectiveness of standard therapy, many complementary or alternative medicines (CAM) have been tried in patient with a variety of cancers.
Mistletoe extracts are among commonly prescribed CAM for cancer patients. Mistletoe is a semiparasitic plant that grows on several types of trees, including apple, oak, maple, elm, pine, and birch. Viscum album L. extract (VAE) was introduced as a possible treatment for cancer in 1920 by Steiner and Wegman.(1) Mistletoe extracts have been shown to kill cancer cells in the laboratory and to boost the immune system.(2-4) In animal studies, activation of natural killer (NK) cells, monocytes/macrophages, T cells and cytokine release have been demonstrated.(5) Although there are numerous reports regarding cytokine secretion induced by VAE in vitro or in animals, there is limited information on the immunostimulatory effects of VAE in vivo, especially used in adjuvant setting after conventional treatment in patients with operable breast cancer. The aim of this study was to assess the immunologic effects of VAE after surgery followed by standard adjuvant chemoradiation therapy in patients with early breast cancer. The immunologic parameters such as interleukin-2 (IL-2), IL-4, IL-6, IL-10, transforming growth factor-beta (TGF-β), and interferon-gamma (IFN-γ) were measured in test group with VAE treatment and in control group.
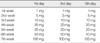
All patients enrolled in this study were diagnosed with stage I or II primary breast cancer and received a standard course of breast conserving surgery, CAF (cyclophosphamide, doxorubicin, and fluorouracil) chemotherapy, and conventional radiation therapy at the department of breast-endocrine surgery of Korea University Medical Center from March 2007 to December 2008. At the time of enrollment, any patient had hematologic abnormality or any other co-morbid condition affecting to immunity was excluded. Total 20 patients were randomly assigned to receive the conventional therapy only (control group, n=10) or the conventional therapy followed by VAE (Helixor®) treatment (test group, n=10). The test group patients started receiving a series of subcutaneous VAE injections two weeks after completion of conventional therapy. VAE was injected three times a week for seven weeks in escalating doses from 1 mg up to 100 mg according to the treatment schedule (Table 1). All patients tolerated the treatment without interruption by the considerable complications such as severe local reaction or fever. Blood samples (5 mL for sera) were collected before and one week after completion of the scheduled VAE injections from test group, and from control group at the corresponding time. The institutional review board of Korea University Anam Hospital approved this study and all patients provided informed consent.
Plasma samples from each patient were collected and stored in a -80℃ freezer until analysis. Measurements of IL-2, IL-4, IL-6, IL-10, TGF-β, and human IFN-γ levels in serum samples from patients were quantified by ELISA (R&D Systems, Abingdon, UK) according to the manufacturer's instructions.
Data were analyzed using the Statistical Package for the Social Sciences (SPSS) program (version 14.0; SPSS Inc., Chicago, USA). Descriptive statistics were calculated to summarize the data. The concentrations in each cytokine between before and after VAE treatment in each group were compared with the Wilcoxon signed-rank test. The differences of concentration in each cytokine between test and control group were analyzed by the Mann-Whitney U test. All comparisons were considered significant at p-value <0.05.
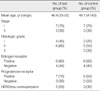
All patients were diagnosed as an invasive ductal carcinoma of breast. One patient of test group had a lobular carcinoma component. The mean age at diagnosis was 46.9 yr, range from 33 to 53 yr in test group and 48.7 yr, range from 41 to 63 yr in control group. Seven patients were stage I and three patients were stage II in each group. Estrogen receptor was positive in six patients in each group (Table 2).
The mean concentrations of IL-2 were changed from 7.80±1.59 pg/mL and 8.50±2.35 pg/mL before treatment to 8.01±1.45 pg/mL and 7.67±1.76 pg/mL after treatment in the test and control group. But there were not significant differences between both groups and between before and after. The mean concentrations of IL-4 were measured from 11.78±4.04 pg/mL and 13.21±3.48 pg/mL before treatment in the test and control group to 13.81±5.13 pg/mL and 12.92±2.93 pg/mL after treatment. They were statistically not different too. In IL-10, there were also not significant changes, from 20.20±0.61 pg/mL and 20.24±0.76 pg/mL before in the test and control group to 20.43±0.70 pg/mL and 20.07±0.56 pg/mL after. The concentration of TFG-β was increased from 28.25µ15.51 pg/mL to 35.08µ13.54 pg/mL after treatment in test group, but similar change was also measured in control group, from 30.26±12.66 pg/mL to 34.65±10.87 pg/mL. The differences between both groups and between before and after were statistically not significant.
The concentration of IL-6 in the test group was significantly increased from 8.19±1.75 pg/mL to 9.86±1.46 pg/mL after treatment (p=0.013) in contrast to slight decrease from 9.44±2.43 pg/mL to 8.76±1.33 pg/mL in control group (Figure 1). The concentration of IFN-γ was remarkably increased after treatment from 91.76±17.16 pg/mL to 167.42±66.61 pg/mL in the test group (p=0.009), compared to no change from 87.58±11.35 pg/mL to 92.83±15.80 pg/mL in the control group (Figure 2). The change in concentration of IFN-γ after treatment was statistically significant between test group and control group (p=0.002) (Table 3).
Impairment in immune function has been demonstrated in cancer patients.(6) In addition, cancer treatment with chemotherapy and radiotherapy generally leads to further immune-suppression. We wondered whether VAE therapy as immunemodulator could lead to improved immunity in immune-compromised patients after chemoradiation. In this study we measured IL-2, IL-6, and IFN-γ as parameters for cell-mediated immunity, IL-4 for humoral immunity, and IL-10 and TGF-β for suppression in immunity.
During the development of the tumor specific immune response, T helper (Th) cells are differentiated in two subsets (Th1 and Th2 cells), depended on cytokines (IL-6, IL-12) secreted by monocytes/dendritic cells. T helper type 1 (Th1) cells are characterized by their hallmark cytokine IFN-γ and are shown to be important for cell-mediated immune responses by their activation of macrophages and the killing of intracellular pathogens. In contrast, Th2 cells produce IL-4 and IL-5, cytokines that they showed are involved in humoral immunity by antibody responses.(7) IL-10 is mainly expressed in monocytes, Th2 cells, and regulatory T cells. It has pleiotropic effects in immunoregulation and inflammation. It down-regulates the expression of Th1 cytokines but enhances B cell survival, proliferation, and antibody production. TGF-β is important in regulation of the immune system by regulatory T cells. It appears to block the activation of monocyte and IL-2 induces the differentiation of cytotoxic T lymphocytes and effects on NK cells. IL-6 also induces the stimulation of cytotoxic T cells and helps in producing lymphokine-activated killer cells. IFN-γ plays a critical role in the immune system. It is produced predominantly by NK cells and natural killer T (NKT) cells as part of the innate immune response.
Several studies have shown the immunological responses to mistletoe extracts in patients with a variety of cancers. Signaling by purified mistletoe lectin induces activation of transcription and secretion of pro-inflammatory cytokines such as IL-1, IL-6, and TNF-α in human peripheral blood mononuclear and endothelial cells.(8) Kovacs(9) showed that treatment with VAE lead an increase in the serum level of IL-12 and an increase of IL-12 and IFN-γ secretion in peripheral blood mononuclear cells. Gardin(10) reported the increases in the number of white blood cells, activated T lymphocytes, complements (C3, C4), immunoglobulins (IgA, IgG, IgM), and delayed hypersensitivity reaction by VAE treatment. The results of this study showed that serum IL-6 and IFN-γ were increased after VAE therapy used in adjuvant setting in patients with breast cancer.
IL-6 is a pleiotropic cytokine that modulates multiple aspects of normal immune and non-immune cell function. Many studies have documented high IL-6 levels in the serum of patients with certain carcinomas (i.e., breast, lung and lymphoma) and have correlated high IL-6 levels with a poor clinical prognosis. In the presence of breast cancer tissue, IL-6 may activate malignant progression of breast cancer cells and enhance metastasis. These data imply an oncogenic role for IL-6. However, the mechanisms involved have not been described.(11-13) By contrast, IL-6 has been reported to induce host immunity involved in the regression of tumors such as melanoma, lung cancer, sarcoma, B lymphoma, and colon cancer.(14-16) The cytolytic activity of NK cells has been reported to be enhanced by IL-6.(17) In immune-compromised animal models, a possible vaccination effect with IL-6 has been reported.(18) VAE stimulates maturation of dendritic cells via secretion of pro-inflammatory cytokines, such as IL-6 and IL-8 in vitro.(19) In this study, because the concentrations of IL-6 in both the test and control groups before VAE treatment were not statistically different and VAE was used after surgical removal of the primary tumor, increased IL-6 concentration appear not to be associated with the tumor, but to be secreted from innate T cells or macrophages under the influence of VAE. This suggests the immunostimulatory effects of VAE.
INF-γ is a cytokine that is involved in promoting both protective immune responses and immune-pathological processes. IFN-γ is produced predominantly by NK cells and NKT cells as part of the innate immune response, and by CD4+ helper and CD8+ cytotoxic T lymphocytes, once antigen specific immunity develops.(20) Lymphocytes and INF-γ have been reported to collaborate in preventing the development of spontaneous intestinal and breast cancers.(21) IFN-γ can exert direct anti-proliferative effects on various tumors. IFN-γ dependent inhibition of cellular proliferation has been observed in human fibrosarcomas and murine fibroblasts.(22) In regard to immunological function, IFN-γ is known as a major macrophage activating factor capable of inducing macrophages to non-specifically kill a variety of tumor cells.(23) In an animal study with mice, production of IFN-γ by activated NKT cells subsequently induced activation of NK cell proliferation and cytolytic activity.(24)
The results of this study showed the increases of IL-6 and IFN-γ levels in peripheral blood by VAE. This suggests that VAE can be used as an immunomodulator in adjuvant setting in patients with breast cancer. However, because this study was carried out on a small numbers of patients, it needs to be confirmed by further studies with a large scale. To more popular use of VAE, further studies for finding out the mechanisms by which VAE increases the immunity will be needed.
Significant increases in the serum concentration of IL-6 and IFN-γ were observed after VAE treatment. These results suggest that VAE can stimulate immune responses, especially cell-mediated immunity, in immune-compromised patients received the conventional chemoradiation for breast cancer.
Figures and Tables
 | Figure 1The changes of IL-6 concentration after Viscum Album treatment in the control and test group. |
References
1. Ernst E, Schmidt K, Steuer-Vogt MK. Mistletoe for cancer? A systematic review of randomised clinical trials. Int J Cancer. 2003. 107:262–267.
2. Bussing A. Immune modulation using mistletoe (Viscum album L.) extracts Iscador. Arzneimittelforschung. 2006. 56:508–515.
3. Kienle GS, Berrino F, Büssing A, Portalupi E, Rosenzweig S, Kiene H. Mistletoe in cancer: a systematic review on controlled clinical trials. Eur J Med Res. 2003. 8:109–119.
4. Kienle GS, Kiene H. Complementary cancer therapy: a systematic review of prospective clinical trials on anthroposophic mistletoe extracts. Eur J Med Res. 2007. 12:103–119.
5. Lyu SY, Park WB. Mistletoe lectin (Viscum album coloratum) modulates proliferation and cytokine expressions in murine splenocytes. J Biochem Mol Biol. 2006. 39:662–670.

6. Sulizeanu D. Immunosuppressive factors in human cancer. Adv Cancer Res. 1993. 60:247–267.
7. Mosmann TR, Coffman RL. TH1 and TH2 cells: different patterns of lymphokine secretion lead to different functional properties. Annu Rev Immunol. 1989. 7:145–173.

8. Hajto T, Hostanska K, Gabius HJ. Modulatory potency of the beta-galactoside-specific lectin from Mistletoe Extract (Iscador) on the host defense system in vivo in rabbits and patients. Cancer Res. 1989. 49:4803–4808.
9. Kovacs E. Serum levels of IL-12 and the production of IFN-gamma, IL-2 and IL-4 by peripheral blood mononuclear cells (PBMC) in cancer patients treated with Viscum album extract. Biomed Pharmacother. 2000. 54:305–310.

10. Gardin NE. Immunological response to mistletoe (Viscum album L.) in cancer patients: a four-case series. Phytother Res. 2009. 23:407–411.

11. Yokoe T, Iino Y, Morishita Y. Trends of IL-6 and IL-8 levels in patients with recurrent breast cancer: preliminary report. Breast Cancer. 2000. 7:187–190.

12. Knüpfer H, Preiss R. Significance of interleukin-6 in breast cancer (review). Breast Cancer Res Treat. 2007. 102:129–135.

13. Kurebayashi J. Regulation of interleukin-6 secretion from breast cancer cells and its clinical implications. Breast Cancer. 2000. 7:124–129.

14. Mullen CA, Coale MM, Levy AT, Stetler-Stevenson WG, Liotta LA, Blaese RM. Fibrosarcoma cells transduced with the IL-6 gene exhibited reduced tumorigenicity, increased immunogenicity, and decreased metastatic potential. Cancer Res. 1992. 52:6020–6024.
15. Sun WH, Kreisle RA, Phillips AW, Ershler WB. In vivo and in vitro characteristics of interleukin 6-transfected B16 melanoma cells. Cancer Res. 1992. 52:5412–5415.
16. Xiao B, Jing B, Zhang YL, Zhou DY, Zhang WD. Tumor growth inhibition effect of hIL-6 on colon cancer cells transfected with the target gene by retroviral vector. World J Gastroenterol. 2000. 6:89–92.

17. Luger TA, Krutmann J, Kirnbauer R, Urbanski A, Schwarz T, Klappacher G, et al. IFN-beta 2/IL-6 augments the activity of human natural killer cells. J Immunol. 1989. 143:1206–1209.
18. Ishiguro H, Kishimoto T, Furuya M, Nagai Y, Watanabe T, Ishikura H. Tumor-derived interleukin (IL)-6 induced anti-tumor effect in immune-compromised hosts. Cancer Immunol Immunother. 2005. 54:1191–1199.

19. Elluru SR, van Huyen JP, Delignat S, Kazatchkine MD, Friboulet A, Kaveri SV, et al. Induction of maturation and activation of human dendritic cells: a mechanism underlying the beneficial effect of Viscum album as complimentary therapy in cancer. BMC Cancer. 2008. 8:161.
20. Schoenborn JR, Wilson CB. Regulation of interferon-gamma during innate and adaptive immune responses. Adv Immunol. 2007. 96:41–101.
21. Shankaran V, Ikeda H, Bruce AT, White JM, Swanson PE, Old LJ, et al. IFNgamma and lymphocytes prevent primary tumour development and shape tumour immunogenicity. Nature. 2001. 410:1107–1111.

22. Bromberg JF, Horvath CM, Wen Z, Schreiber RD, Darnell JE Jr. Transcriptionally active Stat1 is required for the antiproliferative effects of both interferon alpha and interferon gamma. Proc Natl Acad Sci U S A. 1996. 93:7673–7678.





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download