Abstract
Purpose
This study was designed to assess the incidence of pulmonary toxicity (PT) and related risk factors in breast cancer patients treated with postoperative adjuvant radiotherapy (RT) with or without the use of chemotherapy.
Methods
The whole breast or chest wall was irradiated with two tangential photon fields to a total dose of 50.4 Gy in 261 patients. A single anterior oblique photon field for a supraclavicular (SCL) node included if indicated. All patients underwent three-dimensional RT planning (3D RTP), and the calculation of dose volume histogram (DVH) parameters (i.e., ipsilateral lung volume that received ≥15 Gy [V15], V20, V30, and mean lung dose [MLD]). The relationship of symptomatic radiation pneumonitis (SRP) and pulmonary toxicity as discerned by radiographic features (radiographic pulmonary toxicity or RPT) with the clinical and DVH parameters were evaluated. In addition, the relationship of severity of RPT with the DVH parameters was assessed.
Results
SRP and RPT developed in 1.9% (5/261) and 22.6% (59/261) of patients, respectively. Age (p=0.008), inclusion of an SCL field (p<0.0001), use of chemotherapy (p<0.0001), use of taxane (p<0.0001), and all DVH parameters (p<0.0001) were associated with RPT in univariate analysis. Based on the results of multivariate analysis, V30 (p<0.001), age (p=0.001) and use of taxane (p=0.036) were significant risk factors in the development of RPT. None of the DVH parameters was associated with the severity of RPT.
Radiation pneumonitis (RP) is an inflammatory process that affects the lung and usually occurrs 1-6 months after radiotherapy (RT). Although symptomatic radiation pneumonitis (SRP) including cough, dyspnea, and/or low-grade fever, is relatively rare, radiographic pulmonary toxicity (RPT), which is defined as pulmonary toxicity as discerned by the presence of specific radiographic features, is relatively common after RT for breast cancer.
As available data on the histopathological changes in irradiated human lungs is limited, existing findings have mostly obtained from the use of animal models. Findings in animal studies have indicated that increased vascular permeability with alveolar vascular congestion is an early histopathological finding, and the alveoli are filled with inflammatory cells and the alveolar septa are thickened with fibroblast proliferation and increased collagen accumulation, resulting in respiratory symptoms.(1-3)
A prediction of the risk of RP is important to reduce normal tissue complications as well as to maximize tumor control probability. Recently, a three-dimensional RT planning (3D-RTP) system, which is able to provide detailed information about the dose-volume distribution in the target, has been routinely used to improve the therapeutic ratio in clinical practice for various cancers including breast cancer. It is challenging to relate quantitative volumetric parameters to the development of SRP and RPT. Although several studies have reported about the dose-volumetric relationship with pulmonary toxicity in lung cancer, few findings are available concerning lung toxicity after RT in breast cancer.(4-6)
The purpose of this study was to evaluate retrospectively the incidence and potential predictive factors for SRP and RPT after the use of adjuvant RT for breast cancer. The correlation of the severity of RPT with dose volume histogram (DVH) parameters using 3D-RTP were also evaluated.
Between September 2003 and February 2007, a total of 315 patients were treated with adjuvant RT after breast conserving surgery or a mastectomy at Seoul National University Bundang Hospital. Of the 315 patients, 54 patients were excluded from the study due to the following reasons. The use of 3-D RTP was not performed for 33 patients, ten patients were lost at follow-up, five patients had unavailable follow-up chest radiographs, two patients did not complete the RT schedule, two patients had bilateral breast cancer, one patient received double primary lung cancer surgery immediately after RT and one patient had the sternum included in the clinical target volume due to the presence of a suspicious bone metastasis. The median age of patients was 46 yr (range, 16-78 yr). A total of 164 patients received systemic chemotherapy (CTx). Of these patients, a taxane-based chemotherapeutic regimen was used in 89 patients, with paclitaxel and docetaxel used in 62 and 27 patients, respectively. Regional RT to the supraclavicular (SCL) nodal area was indicated in 87 patients. The patient characteristics are summarized in Table 1. A diagnosis of SRP was based on clinical and/or radiographic changes and RPT was reviewed with chest radiographs. The relationship of RPT with the clinical and DVH parameters was evaluated, and the relationship between severity of RPT and the DVH parameters was also assessed.
The post-lumpectomy breast was typically treated with two opposing tangential 6 MV photon fields to a total dose of 50-50.4 Gy (Clinac; Varian, Palo Alto, USA). The tumor bed was generally treated with an additional 9-10 Gy by an en face electron field for patients with invasive carcinoma after lumpectomy. The postmastectomy chest wall was treated in a similar fashion with tangential photon fields to a dose of 50.4 Gy. The SCL fossa was treated with an anterior oblique photon fields to a total dose of 50.4 Gy for patients with a primary tumor size ≥5 cm and/or ≥4 positive axillary nodes. The border between the tangential fields and the SCL field was typically at the level of the inferior aspect of the clavicular head. Routine irradiation of the internal mammary lymph nodes was not applied because of a concern about potential cardiopulmonary toxicity.
To evaluate the relationship with RPT, DVH parameters including the overall percentage of the ipsilateral lung volume that received ≥15 Gy (V15), 20 Gy (V20), 30 Gy (V30) and the mean lung dose (MLD) were calculated based on the cumulative DVH.
All patients received follow-up by a radiation oncologist at one month after completion of RT, then at every three months for the first year and every six months thereafter. A chest radiologist reviewed serial follow-up chest radiographs, with a minimum follow-up of 1 yr. Radiation Therapy Oncology Group (RTOG) toxicity criteria were used for grading SRP and patients with RTOG grade 2 or higher RP were considered to have SRP. A modified WHO grading system based on comprehensive scoring analysis of the RPT area of the ipsilateral lung, the degree of shadowing and the distortion of anatomy was used to evaluate the severity of RPT (Table 2).
Statistical analysis were performed by use of SPSS software (release 12.0.1, SPSS Inc., Chicago, USA). Logistic regression analysis was used to identify potential risk factors for RPT. Pearson's correlation was applied to identify the correlation between the severity of RPT and the DVH parameters.
Of 261 patients, only five patients (1.9%) developed SRP. All patients complained of dry cough and dyspnea and/or low-grade fever that were associated with radiographical evidence of pneumonitis. One patient with grade 3 SRP required hospitalization and the remainder of symptoms were resolved with supportive care with the use of steroid therapy. Two of the patients received regional RT to the SCL nodal area and three of the patients received CTx (two patients underwent taxane-based CTx and one patient underwent non-taxane-based CTx). As a small number of patients developed SRP, we could not identify any clinical variables and DVH parameters that were associated with SRP.
A total of 59 patients (22.6%) developed RPT from a review of the serial chest radiographs. Univariate and multivariate analysis were performed to identify correlations between RPT and various variables, including age, smoking, pre-existing lung disease, inclusion of the SCL field, use of CTx, use of taxane, use of hormonal therapy and all of the DVH parameters. Based on univariate analysis, age (p=0.008), pre-existing lung disease (p=0.044), inclusion of the SCL field (p<0.0001), use of CTx (p<0.0001), the use of taxane (p<0.0001) and all of the DVH parameters (p<0.0001) were associated with RPT. The incidence of RPT was much higher in patients that received regional RT to the SCL nodal area than in patients that did not receive regional RT to the SCL nodal area (49.8% vs 9.2%). Based on multivariate analysis, V30 (p<0.001), age (p=0.001) and the use of taxane (p=0.036) had a significant relationship with RPT. RPT was observed in 27 (17.0%) of 158 patients less than 50 yr-old and in 32 (31.1%) of 103 patients with an age equal or more than 50 yr. RPTs were observed in 41 (46.1%) of 99 patients that had received taxane-based CTx and in 18 (10.5%) of 172 patients that did not receive taxane-based CTx. RPT was observed in four (4.1%) of 98 patients with a V30 of less than 10%, in 12 (15.2%) of 79 patients with a V30 of 10-14.9%, in 7 (29.2%) of 24 patients with a V30 of 15-19.9%, in 19 (59.3%) of 32 patients with a V30 of 20-24.9%, and in 17 (60.7%) of 28 patients with a V30 of equal or more than 25%. The results of univariate and multivariate analysis to assess the relationship between variables and RPT are summarized in Table 3. The distribution of V30 according to development of RPT is shown in Figure 1.
The severity of RPTs were assessed according to a modified WHO grading system and the median RP score was 1.5 (range, 1.5-5.5). None of the DVH parameters was associated with the severity of RPT.
Pulmonary toxicities following radiation therapy for thoracic malignancies are well-known complications, and the incidences of SRP are reported 1% to 34%.(7) Although RP in breast cancer patients treated with RT develops relatively less often than other malignancies such as lung cancer or Hodgkin's disease, this complication should be kept as low as possible since these patients are expected to be long-term survivors. Chest radiographic abnormalities are more common than SRP, with a frequency of 13% to 100%.(7) In our study, the incidence rates of SRP and RPT were 1.9% and 22.6%, respectively.
Factors that increase the risk of damage to lung tissue include age, smoking, the use of an additional SCL field, irradiated lung volume, sequential CTx and concurrent hormonal therapy.(8-13) Actually, it is difficult to estimate the effect of patient-related factors such as age, gender, smoking and performance status on RP as there are many confounding factors for patients who are often treated with different regimens and have diverse comorbidities. In our study, we could not find an association between the development of SRP and any clinical factors or DVH parameters. This result may be due to the low incidence of SRP in our population. However, age, the use of taxane-based CTx and V30 were associated with the presence of radiographic lung abnormalities.
Studies examining the effect of the use of combined CTx and RT on the development of RP have been reported and have demonstrated an increased incidence of RP.(11,12,14) With the increasing use of paclitaxel, several studies have been reported investigations on the role of paclitaxel in the development of RP.(14-17) There have been conflicting results on the relationship of the use of taxane-based CTx with RP, depending on the sequence of CTx-RT (Table 4). In our study, all patients were treated with CTx and sequential RT. The results determined in our study were consistent with the findings of the previous study(17) where taxane-based CTx used sequentially with RT was not associated with the risk of SRP. The incidence of SRP was low (1.9%), but the incidence of RPT was higher in patients that received taxane-based CTx than in patients that did not receive taxane-based CTx (46.1% vs 10.5%). There is a possible explanation for this result. In our study, most of the patients treated with taxane-based CTx, were irradiated on the SCL fossa, which led increased lung volume included in RT ports. The incidence of RPT might be higher in such patients, though inclusion of the SCL field had no statistical significance for the development of RPT. The mechanism that taxane-based CTx tends to increase the risk of RPT is not clear, though the use of taxane is known to increase the cytotoxicity of RT. The association between the risk of RP and RT with the use of taxane-based CTx given either concurrently or sequentially has yet to be resolved with additional clinical studies.
Recently, data obtained from 3D-RTP has made it possible to estimate dose-volume effects on lung injury. Several studies have demonstrated a correlation of dosimetric parameters with the incidence of RP in lung cancer patients treated with adjuvant RT.(4,6,18) However, few studies have analyzed the effect of the dose-volumetric parameters on RP in breast cancer patients, as the risk for SRP after radiation therapy for breast cancer is relatively low. In our study, we could not find any DVH parameters associated with SRP. However, our study showed that V30 was a useful RT parameter to predict RPT. RPT was observed in approximately 30% of patients with a V30 of 15-19.9% and RPT was greater than 50% in patients with a V30 of equal or more than 20%. Considering that RPT would be a detrimental effect on lung function, studies of the clinical importance of RPT should be investigated.
Unlike as described in previous reports, we failed to find an association between other factors including the use of hormonal therapy or smoking and the risk of both SRP and RPT.(10,11) Further studies using conformal RT are needed to analyze the risk factors associated with RPT as well as SRP in order to minimize radiation induced cardiopulmonary toxicities.(19)
The incidence of SRP was acceptable and the risk of SRPs was not affected by any clinical factors and the DVH parameters. Therefore, adjuvant RT using 3D-RTP for breast cancer can be used safely without concerns for SRP. However, the risk of RPT was associated with age, the use of taxane-based CTx and V30.
Figures and Tables
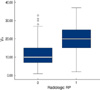 | Figure 1Distribution of V30 according to the development of radiographic pulmonary toxicity.
0=absence of pneumonitis; 1=presence of pneumonitis.
|
Table 3
Univariate and multivariate analysis of clinical and dose volume histogram parameters for the prediction of radiographic pulmonary toxicity

Table 4
Incidence of RP associated with taxane-based CTx as reported in the literature

RP=radiation pneumonitis; CTx-RT=chemotherapy-radiotherapy.
*Score based on modified Radiation Therapy Oncology Group toxicity criteria; †Score based on Radiation Therapy Oncology Group toxicity criteria; ‡Score based on modified Radiation Therapy Oncology Group/European Organization for Research and Treatment of Cancer late radiation morbidity score; §No mention of toxicity criteria or score.
References
1. McDonald S, Rubin P, Phillips TL, Marks LB. Injury to the lung from cancer therapy: clinical syndromes, measurable end point, and potential scoring systems. Int J Radiat Oncol Biol Phys. 1995. 31:1187–1203.

2. Rosai J. Rosai J, editor. acute pulmonary injury and interstitial pneumonia. Ackerman's surgical pathology. 1996. Vol. 1:8th ed. New York: Mosby;358–359.
3. Gross NJ. Experimental radiation pneumonitis. IV. Leakage of circulatory proteins onto the alveolar surface. J Lab Clin Med. 1980. 95:19–31.
4. Hernando ML, Marks LB, Bentel GC, Zhou SM, Hollis D, Das SK, et al. Radiation-induced pulmonary toxicity: a dose-volume histogram analysis in 201 patients with lung cancer. Int J Radiat Oncol Biol Phys. 2001. 51:650–659.

5. Armstrong JG, Zelefsky MJ, Leibel SA, Burman C, Han C, Harrison LB, et al. Strategy for dose escalation using 3-dimensional conformal radiation therapy for lung cancer. Ann Oncol. 1995. 6:693–697.

6. Kim TH, Cho KH, Pyo HR, Lee JS, Zo JI, Lee DH, et al. Dose-volumetric parameters predicting severe radiation pneumonitis after three-dimensional conformal radiation therapy for lung cancer. Radiology. 2005. 235:208–215.

7. Movsas B, Raffin TA, Epstein AH, Link CJ. Pulmonary radiation injury. Chest. 1997. 111:1061–1076.

8. Lingos TI, Recht A, Vicini F, Abner A, Silver B, Harris JR. Radiation pneumonitis in breast cancer treated with conservative surgery and radiation therapy. Int J Radiat Oncol Biol Phys. 1991. 21:355–360.

9. Lind PARM, Gagliardi G, Wennberg B, Fornander T. A descriptive study of pulmonary complications after postoperative radiation therapy in node-positive stage II breast cancer. Acta Oncol. 1997. 36:509–515.

10. Bentzen SM, Skoczylas JZ, Overgaard M, Overgaard J. Radiotherapy-related lung fibrosis enhanced by tamoxifen. J Natl Cancer Inst. 1996. 88:918–922.

11. Theuws JC, Kwa SL, Wagenaar AC, Boersma LJ, Damen EM, Muller SH, et al. Dose-effect relations for early local pulmonary injury after irradiation for malignant lymphoma and breast cancer. Radiother Oncol. 1998. 48:33–43.

12. Lind PA, Marks LB, Jamieson TA, Carter DL, Vredenburgh JJ, Folz RL, et al. Predictors for pneumonitis during locoregional radiotherapy in high-risk patients with breast carcinoma treated with high-dose CTx and stem-cell rescue. Cancer. 2002. 94:2821–2829.

13. Quon H, shepherd FA, Payne DG, Coy P, Murray N, Feld R, et al. The influence of age on delivery, tolerance, and efficacy of thoracic irradiatin in the combined modality treatment of limited stage small cell lung cancer. Int J Radiat Oncol Biol Phys. 1999. 43:39–45.

14. Taghian AG, Assaad SI, Niemierko A, Kuter I, Younger J, Schoenthaler R, et al. Risk of pneumonitis in breast cancer patients treated with radiation therapy and combination chemotherapy with paclitaxel. J Natl Cancer Inst. 2001. 93:1806–1811.

15. Burstein HJ, Bellon JR, Galper S, Lu HM, Kuter I, Taghian AG, et al. Prospective evaluation of concurrent paclitaxel and radiation therapy after adjuvant doxorubicin and cyclophosphamide chemotherapy for stage II or III breast cancer. Int J Radiat Oncol Biol Phys. 2006. 64:496–504.

16. Taghian AG, Assaad SI, Niemierko A, Floyd SR, Powell SN. Is a reduction in radiation lung volume and dose necessary with paclitaxel chemotherapy for node-positive breast cancer? Int J Radiat Oncol Biol Phys. 2005. 62:386–391.

17. Yu TK, Whitman GJ, Thames HD, Buzdar AU, Strom EA, Perkins GH, et al. Clinically relevant pneumonitis after sequential paclitaxel-based chemotherapy and radiation in breast cancer patients. J Natl Cancer Inst. 2004. 96:1676–1681.

18. Graham MV, Purdy JA, Emami B, Harms W, Bosch W, Lockett MA, et al. Clinical dose-volume histogram analysis for pneumonitis after 3D treatment for non-small cell lung cancer (NSCLC). Int J Radiat Oncol Biol Phys. 1999. 45:323–329.

19. Kim KJ, Suh CO. Partial breast cancer (PBI). J Korean Breast Cancer Soc. 2004. 7:65–71.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download