Abstract
Purpose
False negative results obtained with the use of a sentinel lymph node biopsy (SLNB) can result in down staging of tumors, whereas the use of a more elaborated pathological examination of sentinel lymph nodes might lead to upstaging of tumors. The purpose of this study was to compare results after performing only an SLNB as compared with performing conventional axillary lymph node dissection (ALND) without an SLNB in pathologically node negative (pN0) breast cancer patients.
Methods
From April 2004 to June 2007, SLNBs were performed for patients with primary breast cancer who had no clinical evidence of a lymph node metastasis. A total of 272 patients were treated with only an SLNB. During the same period, 278 patients were confirmed as pN0 after conventional ALND without an SLNB. A prospectively collected database and medical records of these patients were reviewed.
Results
For patients that had undergone only an SLNB, there was no local or regional recurrence. A distant metastasis developed in four patients (1.5%). In patients that had undergone ALND without an SLNB, a recurrence was found in 13 patients (4.7%). Patients that had undergone only an SLNB showed significantly better disease-free survival as compared to patients that had undergone ALND without an SLNB (p=0.032).
Conclusion
pN0 patients treated with only an SLNB showed a significantly better outcome as compared to patients treated with conventional ALND without an SLNB. These results suggest that performing an SLNB might result in the upstaging of a subset of patients who would have been understaged by the use of conventional ALND.
Evaluating for the possible presence of axillary lymph node metastasis is critical to predict the prognosis and to determine the treatment strategy for those patients suffering with breast cancer.(1) The use of axillary lymph node dissection (ALND), which has long been performed to assess the axillary stage, can cause acute or chronic arm edema and long-term morbidities such as a limitation of shoulder motion, paresthesia of the arm, loss of sensation or pain.(2-4)
About ten years ago, the use of a sentinel lymph node biopsy (SLNB) was introduced into the field of breast cancer treatment and this has rapidly became one of the standard methods for axillary staging in many institutions.(5-8) However, several questions have been raised about the use of only SLNB for axillary staging. A false negative rate of 2-10% has continuously been reported for SLNB.(8-11) A false negative result after performing SLNB might result in the down-staging of a tumor and so deprive the patient of a chance for proper management, such as chemotherapy. On the other hand, there is also the possibility of up-staging of a tumor due to a more elaborated examination of the sentinel lymph nodes (SLNs) with using multiple node sections and immunohistochemical methods.(12-14) There currently are insufficient answers about what would happen with the sum of these opposite effects of SLNB, that is, down-staging versus up-staging.
We have proposed that if down-staging of a tumor after performing SLNB was more common, then the prognosis of the pathologically node negative (pN0) patients treated with only SLNB would be worse than that for the patients who were treated with conventional ALND. In contrast, if up staging of a tumor that's due to the more elaborated examination of the SLNs were more common than a finding of a false negative result, then the patients who undergo SLNB only would show a better prognosis than that of the patients who undergo ALND without SLNB.
At our institution, performing SLNB only has been done since April 2004 (and after the learning curve period) to treat those patients with negative SLNs on the serial frozen sections. In this study, we compared the outcomes of pN0 patients who were treated either with SLNB only or with conventional ALND without SLNB during the same time period.
From April 2004 to June 2007, the patients who had a primary invasive breast cancer smaller than 5 cm and pN0 stage disease and who were treated with SLNB only or with conventional ALND at Korea Cancer Center Hospital were considered for the study. The patients who received SLNB followed by ALND and the patients who were treated with neoadjuvant chemotherapy prior to surgery were excluded from the study. The patients with lymph node metastases larger than 0.2 mm (micrometastases) were classified as N1mic and they were excluded from this study. The sixth edition of the AJCC Cancer Staging Manual was used for staging.(15) The prospectively collected database and medical records of the patients were reviewed for the following clinical and pathological variables: the age at the initial diagnosis, the pathological tumor size, the hormonal receptor status, the expression of c-erb-B2 and the method of treatment. On immunohistochemistry, strong nuclear staining for estrogen receptor or progesterone receptor in more than 10% of tumor nuclei was regarded as positive. Strong and complete cell membrane staining for c-erb-B2 was interpreted as 3+.
The patients were divided into two groups. The SLNB only group was defined as those patients with negative SLNs and they did not undergo further ALND. A total of 272 patients were included in this group. The ALND without SLNB group was defined as the patients who were treated by conventional level I and II ALND without SLNB. Among these patients, the patients who had less than ten harvested lymph nodes were excluded from this study to avoid the effect of misclassification due to a small number of harvested lymph nodes.(16-18) A total of 278 patients were included in the ALND without SLNB group.
As both SLNB and ALND have been considered as standard procedures for axillary staging, the patients were treated with SLNB or ALND without SLNB at the discretion of the individual breast surgeons and the patients. For the SLNB, 2-2.5 mCi of 99Tc-Tin colloid was injected at the upper outer subareolar area on the day of surgery or in the afternoon of the day before surgery.(19) A lymphatic scintigram was obtained for each patient. In the operating room, a hand-held gamma detector (World of Medicine, Berlin, Germany) was used to locate the SLNs. For the ALND without SLNB, conventional level I and II axillary lymph node dissection was performed without SLNB.
The harvested SLNs were submitted to the pathology department for immediate frozen section diagnosis. For the intraoperative evaluation, SLNs with diameters ≤5 mm were bisected, whereas the nodes that measured >5 mm were sectioned every 2 mm. For each sample, two frozen sections that were made at 50 µm intervals were stained with hematoxylin and eosin (H&E staining). For the definite histology, four sections at 50 µm intervals were cut from a paraffin block. Three sections were stained with hematoxylin and eosin and the remaining section was immunostained with a monoclonal antibody against cytokeratin. According to the sixth edition of the TNM Staging System, when a micrometastasis (≥0.2 mm and ≤2 mm) was found, then the cases were classified as N1mic and they were excluded from this study, while tumors with isolated tumor cells (<0.2 mm; ITCs) were classified as pN0.
The axillary lymph nodes harvested by ALND were bisected along the longest diameter and a section was taken from each halve. H&E staining and cytokeratin immunostaining were routinely performed for all sections.
For the patients treated with a lumpectomy, the ipsilateral breast was treated with a total dose of 50-50.4 Gy of radiation. The axillary and supraclavicular areas were not included in the irradiation field. Adjuvant chemotherapy was administered to most of the patients. The patients who did not receive chemotherapy were those patients who were considered to have a minimal risk of recurrence (a tumor size <1 cm, a histological grade of I, a hormone receptor positive status and they were postmenopausal). All the patients with a hormone receptor positive tumor received adjuvant tamoxifen or aromatase inhibitors after completion of chemotherapy.
The probabilities of disease free survival were calculated by using the Kaplan-Meier method and these values were compared by means of the log-rank test. Comparison of the patient characteristics for the SLNB only group and the ALND without SLNB group was done with the use of the chi-square test. A p-value <0.05 was regarded as statistically significant.
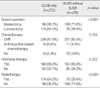
The study population was comprised of 550 patients, including 272 patients in the SLNB only group and 278 patients in the ALND without SLNB group. The mean patient age at diagnosis was 49.6 yr (age range, 26-83 yr). There were no differences for the age of the 2 groups at the time of diagnosis, the TNM classification, the histological grade, the hormone receptor status or the expression of HER2 between patients in the SLNB only group and the patients in the ALND without SLNB group (Table 1). In the SLNB only group, seven patients were identified who had a lymph node metastasis of smaller than 0.2 mm (ITC). In the ALND without SLNB group, no patient were reported as having ITC.
The proportion of patients who were treated with a lumpectomy was higher in the SLNB only group. Radiotherapy was performed more often in the SLNB only group, but none of the patients had received radiotherapy for an axillary lymph node (Table 2). The incidence of administering chemotherapy and hormonal therapy were well balanced between the patients of both groups.
During the mean follow-up period of 27.4 months, a recurrence developed in 17 patients (3.1%). In the SLNB only group, there was no local or regional recurrence. Distant metastasis was found in four patients (1.5%). In the ALND without SLNB group, there were 13 cases (4.7%) of disease recurrence, one case of regional recurrence and 12 cases of systemic relapse. The disease-free survival of the SLNB only group was significantly better than that for the ALND without SLNB group (p=0.032) (Figure 1). Age at diagnosis, T stage, hormonal receptor status, c-erb-B2 status and radiation therapy does not have any significant relation with disease recurrence (Table 3).
Although the use of SLNB has become the standard approach for axillary staging in many medical centers, some critical questions still remain unanswered.(20-24) The biggest concern with utilizing SLNB is its false-negative rate, which is about 2-10% as reported in most studies.(8-11) The prognostic consequences of such false-negative findings are still unclear. Theoretically, a false-negative SLNB might have a negative impact on the prognosis of patients for two reasons. First, undetected metastatic tumor in an axillary lymph node may cause locoregional recurrence or it might be a source of distant metastasis. Second, false-negative findings on SLNB might result in the down-staging of tumors, and systemic adjuvant therapy might be unjustly omitted for a subset of patients. In contrast, SLNB can result in the up-staging of a tumor due to the elaborated pathological evaluation of the SLNs such as characterization of the serial sections and immunohistochemical analysis that is practically just not possible to do for the conventional ALND specimens.
A couple of prospective randomized trials have been conducted to compare the use of SLNB with ALND. In the Milan trials, the disease-free survival and the overall survival of the patients who underwent SLNB were at least equivalent to the DFS and OS of the patients who underwent ALND.(25) In contrast, the Gruppo Interdisciplinare Veneto di Oncologia Mammria (GIVOM) trial group recently reported that both the disease-free survival and the overall survival were slightly worse for the patients who underwent only SLNB as compared to the patients who that underwent SLNB followed by ALND. However, in this study, the false negative rate after SLNB was significantly higher than that of the other previous series (16.4%).(26) Therefore, the definitive comparison between SLNB and ALND would be possible by evaluating the long-term results from a large randomized trial such as the National Surgical Adjuvant Breast and Bowel Project (NSAB) B-32 study.(27)
Although performing SLNB has reduced the morbidity associated with ALND and it has increased the quality of life of breast cancer patients, we do not believe that the use of SLNB can improve the individual patient's prognosis as compared with ALND because SLNB is considered to be one of the staging procedures rather than being a treatment modality. Thus, if there is a difference in the prognosis of the patients with the same stage disease between the patients who undergo SLNB and the patients who undergo ALND, this is most likely due to stage migration. It has been reported that SLNB might cause up-staging. Vanderveen et al.(14) have demonstrated an approximate 5% shift of patients from N0 to N1 disease after the start of performing SLNB, and this suggests that SLNB is more sensitive than ALND for the detection of an early nodal metastasis. Maaskant et al.(12) also reported a significant increase in the proportion of patients with positive nodes after the introduction of SLNB, and this suggests that SLNB has led to up-staging of tumors. However, the results of these studies might be confounded by other time-dependent variables as comparisons were made between patients who were treated in different time periods, that is, before and after the implementation of SLNB. Few studies have compared the outcomes of patients with the same pathological stage and who were treated with SLNB only versus the patients who were treated with conventional ALND during the same period.
In our institution, after confirmation of the low false-negative rate after performing SLNBs through a learning-curve period, ALND has not been done for the patients with negative SLNs, as determined by the serial frozen section diagnosis. During the same period, a similar number of patients were treated with conventional ALND based on the preference of the individual breast surgeon and the patient's preference because ALND still remains one of the standard treatments for breast cancer patients. In this study, we compared the disease-free survival of pN0 patients and we found that the prognosis of the pN0 patients who were treated with SLNB only was significantly better than that of the patients who were treated with ALND without SLNB. This is not a randomized study, but the clinical and pathological characteristics were not different between the two groups and other treatments such as chemotherapy and hormone therapy were applied to patients under the same conditions, and this made it possible to compare between the two groups. Of note, after a median follow-up of 27.4 months, none of the patients in the SLNB only group developed axillary recurrence. The possible explanation for the absence of regional recurrence in the SLNB only group is the low incidence of false negative cases, and this validates the results of a previous study.(28) In addition, it has been suggested that most occult metastases in axillary nodes would not progress to clinically overt axillary recurrence. In the Milan trial, only one out of 167 SLN negative patients developed an axillary recurrence, even though approximately eight patients were estimated to have occult axillary involvement.(25) Hwang et al.(24) have recently reported that for 196 patients with positive SLNs and who did not undergo complete ALND, none of the patient had an axillary recurrence, as seen over a median follow-up period of 29.5 months.
This study has some limitation because it was retrospective surgery. First, mastectomy was more frequently performed in the ALND group. However, It is already well known that the survival is not different between the mastectomy and breast conserving therapy. All patient received lumpectomy in this study were treated by radiation therapy. Therefore, we considered this difference between two groups would not affect the result of this study. Second, the mass size of the SLNB only group had tendency to be smaller than that of the ALND group. Even though the difference was little, it could have influence on this result as selection bias. CONCLUSION In the present study we found that the prognosis of the pN0 patients treated with SLNB only was significantly better than the prognosis of the patients treated with ALND without SLNB. This finding strongly suggests that the use of SLNB leads to up-staging of tumors, and the effect of this up-staging might surpass the possible negative impact on the prognosis of patients that is due to a false-negative result after SLNB. However, because it is only a short-term follow-up results, a long term followup results are needed to make a definitive conclusion.
In the present study we found that the prognosis of the pN0 patients treated with SLNB only was significantly better than the prognosis of the patients treated with ALND without SLNB. This finding strongly suggests that the use of SLNB leads to up-staging of tumors, and the effect of this up-staging might surpass the possible negative impact on the prognosis of patients that is due to a false-negative result after SLNB. However, because it is only a short-term follow-up results, a long term follow-up results are needed to make a definitive conclusion.
Figures and Tables
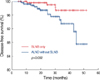 | Figure 1Actuarial curves showing disease-free survival. The disease-free survival of the sentinel lymph node biopsy (SLNB) only group was significantly better than that for the axillary lymph node dissection (ALND) without SLNB group. |
References
1. Goldhirsch A, Wood WC, Gelber RD, Coates AS, Thurlimann B, Senn HJ, et al. Progress and promise: highlights of the international expert consensus on the primary therapy of early breast cancer 2007. Ann Oncol. 2007. 18:1133–1144.

2. Ernst MF, Voogd AC, Balder W, Klinkenbijl JH, Roukema JA. Early and late morbidity associated with axillary levels I-III dissection in breast cancer. J Surg Oncol. 2002. 79:151–155.

3. Lauridsen MC, Overgaard M, Overgaard J, Hessov IB, Cristiansen P. Shoulder disability and late symptoms following surgery for early breast cancer. Acta Oncol. 2008. 47:569–575.

4. Kwan W, Jackson J, Weir LM, Dingee C, McGregor G, Olivotto IA. Chronic arm morbidity after curative breast cancer treatment: prevalence and impact on quality of life. J Clin Oncol. 2002. 20:4242–4248.

5. Crane-Okada R, Wascher RA, Elashoff D, Giuliano AE. Long-term morbidity of sentinel node biopsy versus complete axillary dissection for unilateral breast cancer. Ann Surg Oncol. 2008. 15:1996–2005.

6. Kim HJ, Lee JS, Park EH, Choi SL, Lim WS, Chang MA, et al. Sentinel node biopsy in patients with multiple breast cancer. Breast Cancer Res Treat. 2008. 109:503–506.

7. Kinoshita T. Sentinel lymph node biopsy is feasible for breast cancer patients after neoadjuvant chemotherapy. Breast Cancer. 2007. 14:10–15.

8. Veronesi U, Paganelli G, Viale G, Luini A, Zurrida S, Galimberti V, et al. A randomized comparison of sentinel-node biopsy with routine axillary dissection in breast cancer. N Engl J Med. 2003. 349:546–553.

9. Giuliano AE, Dale PS, Turner RR, Morton DL, Evans SW, Krasne DL. Improved axillary staging of breast cancer with sentinel lymphadenectomy. Ann Surg. 1995. 222:394–399.

10. Chao C, Wong SL, Tuttle TM, Noyes RD, Carlson DJ, Ley P, et al. Sentinel lymph node biopsy for breast cancer: improvement in results over time. Breast J. 2004. 10:337–344.

11. McMasters KM, Wong SL, Chao C, Woo C, Tuttle TM, Noyes RD, et al. Defining the optimal surgeon experience for breast cancer sentinel lymph node biopsy: a model for implementation of new surgical techniques. Ann Surg. 2001. 234:292–299.

12. Maaskant AJ, van de Poll-Franse LV, Voogd AC, Coebergh JW, Tutein Nolthenius-Puylaert MC, Nieuwenhuijzen GA. Stage migration due to introduction of the sentinel node procedure: a populationbased study. Breast Cancer Res Treat. 2009. 113:173–179.

13. van der Heiden-van der, Bezemer PD, Hennipman A, Siesling S, van Diest PJ, Bongers V, et al. Introduction of sentinel node biopsy and stage migration of breast cancer. Eur J Surg Oncol. 2006. 32:710–714.

14. Vanderveen KA, Schneider PD, Khatri VP, Goodnight JE, Bold RJ. Upstaging and improved survival of early breast cancer patients after implementation of sentinel node biopsy for axillary staging. Ann Surg Oncol. 2006. 13:1450–1456.

15. Greene FL, Compton CC, Fritz AG, Shah JP, Winchester DP. AJCC cancer staging manual. 2002. 6th ed. New York: Springer.
16. Axelsson CK, Mouridsen HT, During M, Moller S. Axillary staging during surgery for breast cancer. Br J Surg. 2007. 94:304–309.

17. Axelsson CK, Mouridsen HT, Zedeler K. Axillary dissection of level I and II lymph nodes is important in breast cancer classification. the danish breast cancer cooperative group (DBCG). Eur J Cancer. 1992. 28A:1415–1418.
18. Kiricuta CI, Tausch J. A mathematical model of axillary lymph node involvement based on 1446 complete axillary dissections in patients with breast carcinoma. Cancer. 1992. 69:2496–2501.

19. Kim KS, Kim YH, Paik NS, Kim MS, Choi CW, Moon NM, et al. Utiliy of breast sentinel lymph node biopsy using the day-before or the same-day subareolar injection of 99mTc-tin colloid. J Breast Cancer. 2006. 9:121–126.

20. Naik AM, Fey J, Gemignani M, Heerdt A, Montgomery L, Petrek J, et al. The risk of axillary relapse after sentinel lymph node biopsy for breast cancer is comparable with that of axillary lymph node dissection: a follow-up study of 4008 procedures. Ann Surg. 2004. 240:462–468.
21. Jeruss JS, Winchester DJ, Sener SF, Brinkmann EM, Bilimoria MM, Barrera E Jr, et al. Axillary recurrence after sentinel node biopsy. Ann Surg Oncol. 2005. 12:34–40.

22. Kim HJ, Son BH, Park EW, Lim WS, Seo JY, Jang MA, et al. Axillary recurrence after negative sentinel lymph node biopsy. Breast Cancer Res Treat. 2009. 114:301–305.

23. Guenther JM, Hansen NM, DiFronzo LA, Giuliano AE, Collins JC, Grube BL, et al. Axillary dissection is not required for all patients with breast cancer and positive sentinel nodes. Arch Surg. 2003. 138:52–56.

24. Hwang RF, Gonzalez-Angulo AM, Yi M, Buchholz TA, Meric-Bernstam F, Kuerer HM, et al. Low locoregional failure rates in selected breast cancer patients with tumor-positive sentinel lymph nodes who do not undergo completion axillary dissection. Cancer. 2007. 110:723–730.

25. Veronesi U, Paganelli G, Viale G, Luini A, Zurrida S, Galimberti V, et al. Sentinel-lymph-node biopsy as a staging procedure in breast cancer: Update of a randomised controlled study. Lancet Oncol. 2006. 7:983–990.

26. Zavagno G, De Salvo GL, Scalco G, Bozza F, Barutta L, Del Bianco P, et al. A randomized clinical trial on sentinel lymph node biopsy versus axillary lymph node dissection in breast cancer: results of the Sentinella/GIVOM trial. Ann Surg. 2008. 247:207–213.





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download