Abstract
Purpose
To assess the appropriateness of radiotherapy volume for patients receiving breast-conserving treatment (BCT) through analysis of recurrence pattern and factors affecting recurrence.
Methods
From 1991 to 1996, 362 patients who received BCT were retrospectively evaluated. The radiation volume was the involved breast alone in the patients with less than 4 positive axillary lymph nodes (LNs), and breast and supraclavicular fossa in patients with 4 or more positive axillary LNs. The median follow-up period was 123 months (range, 3-169 months).
Results
Ten-year overall, disease-free, local recurrence-free, and regional recurrence-free survival rates were 86.2%, 82.2%, 95.9%, and 95.2%, respectively. Among 310 patients receiving radiotherapy on the breast alone, 15 (4.8%) had regional recurrence. In particular, patients with inner quadrant lesions had high regional recurrence rates (11/98, 11.2%) (p<0.001).
Conclusion
These low local recurrence rates may reveal that the current radiotherapy technique was successful. However, in cases of inner quadrant lesions, there were a considerable number of regional recurrences, even in N0 cases. This may suggest a potential role for irradiation on regional LNs in this group.
Although breast conserving surgery (BCS) and irradiation is now considered as the preferable treatment method for patients with stage I and II breast cancer, some controversial issues regarding patient eligibility, radiotherapy volume, necessity of boost, and optimal combination of chemotherapy have not been solved yet. As for radiotherapy volume, the conventional approach is whole breast irradiation, typically followed by a boost to the primary tumor bed. It is controversial as to whether nodal areas should also be irradiated.
Since 1991, our institution has instituted a team approach for breast conservation treatment and we previously reported our radiation technique and short term follow-up result.(1,2) As we started breast conserving treatment (BCT) after a National Institutes of Health (NIH) consensus conference(3) in 1990, we followed recommended radiotherapy techniques at that time and had consistently applied the treatment during that period to the patients reported in the current study.
As long-term follow-up is warranted for diseases with a long natural history such as breast cancer, we performed a retrospective analysis of long-term results for patients receiving BCT with early breast cancer. We analyzed the patterns of recurrence and the factors affecting recurrences. We also assessed the appropriateness of radiotherapy technique with a special interest in radiotherapy volume.
Between 1991 and 1996, 362 patients with clinical stage I or II breast cancer were treated with conservative surgery and radiation therapy at Yonsei Cancer Center. Patients with synchronous or metachronous breast cancer were excluded. The median follow-up period was 123 months (range, 3-169 months).
Patient characteristics are summarized in Table 1. The age distribution was 23-80 yr with a median age of 44 yr. The 2002 American Joint Committee on Cancer (AJCC) tumor staging system was used for cancer staging. Two hundred five (56.6%) patients had T1 lesions and the others had T2 lesions. Two hundred forty-two (66.8%) patients were N0. Eighty-one patients had 1 to 3 axillary lymph nodes (LNs) involved with the disease while 38 patients had 4 or more LNs involved with the disease.
All patients underwent lumpectomy or quadrantectomy. Axillary LN dissection was performed in 361 (99.7%) patients. The median number of dissected LNs was 15 (range, 3-46). Thirteen (3.6%) cases had positive resection margins.
All patients were treated with radiotherapy using tangential fields directed at the whole breast after conservative surgery. Radiation was administered using 4-10 MV X-ray linear accelerators. Whole breast dose was 50.4 Gy (range, 45-55.8 Gy) with 1.8-2 Gy per fraction. Tumor bed boost was performed with a 9-12 MeV electron beam. The median boost dose was 10 Gy (range, 10-20 Gy). In cases with positive or close resection margins, total radiation dose including boost dose was increased to 65 Gy. Irradiated volume was the involved breast alone with or without supraclavicular (SCL) fossa in most patients. Patients with 4 or more positive axillary LNs received SCL fossa irradiation. In cases of incomplete axillary LN dissection or extracapsular LN extension, we irradiated the axilla using posterior boost beam. Internal mammary nodes (IMNs) were not irradiated.
Systemic therapy was delivered at the discretion of the medical oncologist involved in each case. One hundred sixty-eight (46.4%) patients with positive axillary LNs or poor prognostic factors such as high nuclear or histological grades received chemotherapy. Cyclophosphamide, methotrexate, and 5-fluorouracil (CMF) or 5-fluorouracil, Adriamycin, and cyclophosphamide (FAC) regimens were administered in 168 (46.4%) patients. Most patients started chemotherapy after recovering from surgery, received 1 or 3 cycles of chemotherapy before radiotherapy, and completed chemotherapy after radiotherapy. No patients received chemotherapy concomitantly with radiotherapy.
Patients were followed every 3 months for 2 yr. Post-radiotherapy mammograms were taken at 6 months after radiotherapy and annually thereafter. Local failure was defined as treatment failure that occurred anywhere within treated breast and classified as 1) true recurrence, defined as being within the primary tumor site or the boost volume of the treated breast; 2) marginal miss, defined as being near the boost volume; 3) elsewhere recurrence, defined as being within treated breast except 1) and 2); or 4) skin recurrence, defined as being the skin of the treated breast.(4) Regional failure was defined as failure that occurred in the ipsilateral axillary, SCL, infraclavicular, IMN regions, and/or level III LN of ipsilateral neck. Contralateral breast recurrence was defined as the occurrence of a second, independent primary breast cancer in the ocontralateral breast after the initial diagnosis of breast cancer.
Overall and disease-free survivals were calculated using the Kaplan-Meier method, with the time period beginning at the time of surgery. Factors potentially affecting regional recurrence were evaluated in univariate analysis using log-rank test. Cox proportional hazards model was used for multivariate analysis.
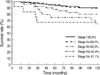
Ten-year overall, cause-specific, disease-free, local recurrence-free, regional recurrence-free, and distant recurrence-free survival rates were 86.2%, 87.3%, 82.2%, 95.9%, 95.2%, and 86.9%, respectively (Figure 1). Ten-year overall survival rates were 90.5%, 89.5%, 80.3%, 64.9%, and 67.1% for stage I, IIa, IIb, IIIa, and IIIc, respectively (Figure 2), while disease-free survival rates were 89.3%, 84.9%, 74.8%, 67.2%, and 38.5%, respectively.
Local failures were noted in 14 (3.8%) patients at 3-106 months (median, 23.5 months) after treatment. Ten patients had local recurrence alone, 1 had local and regional recurrence, and 3 had local and distant recurrence. Among them, there were 4 with true recurrence, 2 with marginal miss, 3 with elsewhere recurrence, and 5 with skin recurrence. All patients with local recurrence only received salvage operation and showed no recurrence thereafter. Any patients with positive resection margin didn't have local recurrence. All local failures, except 1, occurred within 5 yr, and all skin recurrences occurred within 1 yr after treatment. In patients with skin recurrences, the number of involved axillary LNs was 3, 9, 11, 18, and 39. Three of 13 patients with 10 or more positive LNs (23.0%) developed skin recurrences.
Regional failure occurred in 17 (4.6%) patients at 3-90 months (median, 36 months) after treatment. Among them, 11 also had local or distant metastasis. All regional failures occurred within 4 yr after treatment, except 1 SCL LN recurrence found at 90 months. The site of regional recurrence was in the SCL LN in 11 patients, in the IMN in 2 patients, and both in the SCL LN and IMN in 2 patients. There was no axillary LN recurrence. There were 7 cases with contralateral breast recurrence. Distant failures were noted in 40 (11.0%) patients at 3-114 months (median, 36 months) after treatment (Table 2). The most common site was the lung (50.0%). Ten patients with distant metastasis were deceased within 5 yr. Among the 6 patients with only regional recurrence, 2 refused treatment and were deceased in 2 yr while the remaining 4 received systemic chemotherapy and radiotherapy at the site of regional recurrence.
The results of univariate and multivariate analyses using log-rank test for overall and disease-free survival are shown in Table 3. For overall survival, statistically significant differences were observed in pathological T, N, and AJCC stage in univariate analysis. In multivariate analysis, there were no statistically significant factors. For disease-free survival, age; pathological T, N, and AJCC stage; and tumor location were statistically significant in univariate analysis. Patients with inner quadrant tumors showed worse disease-free survival than those with outer quadrant tumors (79.4% vs 86.4%). In multivariate analysis, age and pathological N stage were statistically significant.
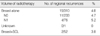
Regional recurrence pattern was analyzed according to radiation volume (Table 4). Among N0 patients who received irradiation to the breast alone, 11 (4.7%) had regional recurrence. Four out of 76 (5.2%) N1 patients who received irradiation to the breast alone experienced regional recurrences. In patients who received SCL irradiation, only 2 showed regional recurrence, 1 of whom had upper neck nodal recurrence while the other had IMN recurrence. Both patients had accompanying distant metastasis and were deceased at 39 and 51 months, respectively. Univariate analyses of factors affecting regional recurrence in the breast alone radiation group were performed. Age and tumor location were found to be significant factors for regional recurrence. In multivariate analysis, only tumor location remained significant for regional recurrence. There were ten recurrences (10/81, 12.3%) in upper inner quadrant and one recurrence (1/17, 6%) in lower inner quadrant. When the tumor location was the inner quadrant, the incidence of regional recurrence was higher than the outer quadrant (11.2% vs 1.9%) (Table 5). The site of regional recurrence in patients with inner quadrant tumor was in the SCL LN in 7 patients, in the IMN in 1 patients, in the neck node in 1 patient, and both in the SCL LN and IMN in 2 patients.
In this study, we report the long-term results of patients with the majority having more than 10-yr of follow-up. Our results are comparable to the long-term results of many other studies.(5-7) Local recurrence rate is low, but we experienced five cases of skin recurrence. As we reported previously,(2) skin recurrences occurred early in patients with extensive axillary LNs metastases. All the skin recurrences occurred within one year after treatment. Twenty three percent of LN>9 cases had skin recurrences. Therefore, application of bolus on intact breast should be considered in case of extensive nodal metastasis.
We evaluated the properness of our radiotherapy technique by analyzing recurrence pattern. We observed a relationship between tumor location and regional recurrence. Regional recurrences were more common in the patients with tumors in the inner location than patients with tumors in the outer location. Ten-year overall survival rate and disease-free survival rate were also worse in the patients with inner location tumors. Most of patients with regional recurrences experienced subsequent distant metastases and in the end succumbed to the cancer. Ten out of seventeen (58.8%) developed distant metastasis and died within five years.
Although there was a lack of consensus concerning the need for irradiation of the regional lymph-node bearing area, there was an agreement for the necessity to avoid axillary irradiation after complete axillary dissection. This was because, not only was the axillary node recurrence rate after axillary dissection negligibly low, but also axillary irradiation also added morbidities such as arm edema, breast edema, and brachial plexopathy.(8) In the National Surgical Adjuvant Breast and Bowel Project (NSABP) B-06 trial and Milan trial in which axillary irradiation was not performed after axillary dissection even in node positive patients, regional recurrence was very low ranging from 2.3% to 4.5%.(9,10) These findings support consider the omission of regional nodal irradiation in patients with positive axillary LNs. In the report from the Joint Center for Radiation Therapy, the incidence of axillary failure for patients undergoing axillary dissection who were irradiated to the breast only was 2.1% for both patient group with negative nodes or positive nodes.(11) In the current study, there was no axillary recurrence. Therefore, we consistently didn't irradiate axilla after proper axillary dissection even in the patient with positive axillary LNs excepting the cases of extracapsular LN extension. However, the role of axillary dissection has more recently been controversial. Several prospective randomized clinical studies have compared results after axillary dissection and regional nodal irradiation.(12,13) These studies show no significant survival difference. Also, the treatment of the axilla in patients with positive sentinel nodes is currently a topic of much debate. For this topic, we need to wait for the results of the large prospective randomized trial (EORTC 10981).(14) Grills et al.(15) reported about risk factors for regional failure after BCT. Although the overall 10-yr regional nodal failure rate was less than 3%, axillary irradiation can significantly reduced the rate of axillary failure in patients with ≥4 positive nodes. The only significant predictor of regional nodal failure was the maximal size of the nodal metastasis. Therefore, a possible benefit to axillary irradiation in some subset of patients cannot be completely excluded.
The current standard of care for patients with negative axillary LNs remains to be whole breast irradiation. Although accelerated partial breast irradiation has been developed and proven feasible with acceptable toxicity in some selective women, it has not yet been demonstrated in randomized trials.(16,17) And SCL fossa irradiation is recommended for patients with more than three positive axillary LNs. However, the data supporting SCL node irradiation in patients with one to three positive axillary LNs is insufficient.(18-20) Therefore, we did not treat SCL fossa irradiation in patients with N0 or N1. And we did not consider IMN irradiation. Since our results showed that a considerable number of regional recurrences occurred in patients with medially located tumors, we began to recognize the necessity of IMN and SCL fossa irradiation. However, we don't have definitive evidence supporting IMN irradiation in breast-conserving treatment at present.
IMN and SCL LN irradiation is still a controversial issue in radiotherapy after BCS and postmastectomy radiation therapy (PMRT). The frequency of IMN involvement in operable breast cancer patients was variable according to the existence or lack of axillary LN metastasis. The rate of IMN metastasis was 6-9% when there was no axillary LN involvement and 28-52% when there was axillary LN involvement.(21) Furthermore, it is known that in case where the tumor is in the inner quadrant, the frequency of IMN involvement was 12-14% even without axillary LN involvement, which is higher than the cases where the tumor was in the outer quadrant. In actuality, it is reported that IMN recurrence was very low, at around 1% clinically.(22) This low incidence might be due to under-reporting. Buchholz (23) explained this discordance as follows. IMNs are not palpable by physical examination and most clinicians do not routinely evaluate IMN regions. Since microscopic IMN involvement has a high risk of developing distant metastases and/or other local recurrences, these recurrences could mask IMN recurrence because regional recurrence is not easily controlled and frequently followed by distant metastasis.(24) Treating IMN metastasis as a subclinical disease would be worthwhile.
There are two ongoing trials which are investigating regional nodal irradiation. The EORTC 10925 trial randomly assigns patients with node-positive or medially or centrally located tumors to irradiation of the upper internal mammary and medial SCL nodes or to no nodal irradiation.(25) The National Cancer Institute of Canada Clinical Trials Group MA.20 trial randomly assigns patients with node-positive or high-risk, node-negative disease following BCS and adjuvant systemic therapy to breast irradiation plus regional nodal irradiation or breast irradiation alone.(26) These trials should address questions regarding efficacy of additional nodal irradiation after breast-conserving surgery or mastectomy and the need to include the internal mammary nodes. Anecdotal experience supporting IMN irradiation was reported by Israel.(27) In the high-dose chemotherapy trial for high risk stage I-II breast cancer, two third of patients received loco-regional radiotherapy including IMN, but one third of the patients did not receive the planned IMN irradiation due to the unavailability of the electron beam. As a result, disease-free survival was significantly prolonged in patients receiving IMN radiation compared to those without IMN irradiation (73% vs 52%).
Predictors of regional recurrence after mastectomy include short tumor-invaded LNs, large tumor size, and higher histological grade.(28-30) Similar findings were observed after breast conservation and young age, lateral hemispheric lesions, positive LNs, histological grade, and hormonal receptor status were predictive factors for regional recurrence.(7,14,24,29) In this study, the regional recurrence rate in N0 patients who received breast alone irradiation was only 1.9% when the lesion was localized to the outer quadrant of the breast. However, the regional recurrence rate was 11.2% when the lesion was in the inner quadrant. This was statistically significant (p=0.006). Although complete pathologic information was not available to determine the many factors responsible for patients such as hormonal receptor status, these findings support internal mammary node irradiation for medially located tumor. This issue should be evaluated in clinical trials which contain current chemotherapy and hormone therapy regimens.
According to our observations, we can conclude that our techniques of radiotherapy for BCT were relevant to positive clinical outcomes based on a low recurrence rate and comparable survival rate. However, in case of inner quadrant lesion, there were a considerable number of regional recurrences even in patients with negative axillary LNs. Based on the findings of this study, it could suggest a potential role for irradiation on regional nodes (IMN and SCL) for the treatment of patients with inner quadrant lesions.
Figures and Tables
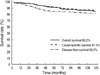 | Figure 1Kaplan-Meier plots of overall, cause-specific, and disease-free survival. Ten-year survival rates were 86.2%, 87.3%, and 82.2%, respectively. |
References
1. Suh CO, Chung EJ, Lee HD, Lee KS, Oh KK, Kim GE. Risk factors for recurrence after conservative treatment in early breast cancer: preliminary report. J Korean Soc Ther Radiol. 1997. 5:331–337.
2. Suh CO, Lee HD, Lee KS, Jung WH, Oh KK, Kim GE. Conservative surgery and primary radiotherapy for early breast cancer: Yonsei Cancer Center experience. J Korean Soc Ther Radiol. 1994. 12:337–348.
3. Dombernowsky P, Andersen JA, Andersen KW, Axelsson CK, Blichert-Toft M, Hansen M, et al. Adjuvant chemotherapy in premenopausal and menopausal high-risk patients with breast cancer. 4. Results of the DBCG (Danish Breast Cancer Cooperative Group) 77B study. Ugeskr Laeger. 1991. 153:2280–2283.
4. Recht A, Silver B, Schnitt S, Connolly J, Hellman S, Harris JR. Breast relapse following primary radiation therapy for early breast cancer. I. Classification, frequency and salvage. Int J Radiat Oncol Biol Phys. 1985. 11:1271–1276.

5. Veronesi U, Banfi A, Salvadori B, Luini A, Saccozzi R, Zucali R, et al. Breast conservation is the treatment of choice in small breast cancer: long-term results of a randomized trial. Eur J Cancer. 1990. 26:668–670.

6. Fisher B, Anderson S, Redmond CK, Wolmark N, Wickerham DL, Cronin WM. Reanalysis and results after 12 years of follow-up in a randomized clinical trial comparing total mastectomy with lumpectomy with or without irradiation in the treatment of breast cancer. N Engl J Med. 1995. 333:1456–1461.

7. Santiago RJ, Wu L, Harris E, Fox K, Schultz D, Glick J, et al. Fifteen-year results of breast-conserving surgery and definitive irradiation for Stage I and II breast carcinoma: the University of Pennsylvania experience. Int J Radiat Oncol Biol Phys. 2004. 58:233–240.

8. Halverson KJ, Taylor ME, Perez CA, Garcia DM, Myerson R, Philpott G, et al. Regional nodal management and patterns of failure following conservative surgery and radiation therapy for stage I and II breast cancer. Int J Radiat Oncol Biol Phys. 1993. 26:593–599.

9. Fisher B, Redmond C, Poisson R, Margolese R, Wolmark N, Wickerham L, et al. Eight-year results of a randomized clinical trial comparing total mastectomy and lumpectomy with or without irradiation in the treatment of breast cancer. N Engl J Med. 1989. 320:822–828.

10. Veronesi U, Zucali R, Del Vecchio M. Conservative treatment of breast cancer with QU.A.R.T. Technique. World J Surg. 1985. 9:676–681.
11. Recht A, Pierce SM, Abner A, Vicini F, Osteen RT, Love SM, et al. Regional nodal failure after conservative surgery and radiotherapy for early-stage breast carcinoma. J Clin Oncol. 1991. 9:988–996.

12. Fisher B, Anderson S, Bryant J, Margolese RG, Deutsch M, Fisher ER, et al. Twenty-year follow-up of a randomized trial comparing total mastectomy, lumpectomy, and lumpectomy plus irradiation for the treatment of invasive breast cancer. N Engl J Med. 2002. 347:1233–1241.

13. Louis-Sylvestre C, Clough K, Asselain B, Vilcoq JR, Salmon RJ, Campana F, et al. Axillary treatment in conservative management of operable breast cancer: dissection or radiotherapy? Results of a randomized study with 15 years of follow-up. J Clin Oncol. 2004. 22:97–101.

14. Rutgers EJ, Meijnen P, Bonnefoi H. Clinical trials update of the European Organization for Research and Treatment of Cancer Breast Cancer Group. Breast Cancer Res. 2004. 6:165–169.

15. Grills IS, Kestin LL, Goldstein N, Mitchell C, Martinez A, Ingold J, et al. Risk factors for regional nodal failure after breast-conserving therapy: regional nodal irradiation reduces rate of axillary failure in patients with four or more positive lymph nodes. Int J Radiat Oncol Biol Phys. 2003. 56:658–670.

16. Arthur DW, Vicini FA. Accelerated partial breast irradiation as a part of breast conservation therapy. J Clin Oncol. 2005. 23:1726–1735.

18. Ragaz J, Jackson SM, Le N, Plenderleith IH, Spinelli JJ, Basco VE, et al. Adjuvant radiotherapy and chemotherapy in node-positive premenopausal women with breast cancer. N Engl J Med. 1997. 337:956–962.

19. Overgaard M, Hansen PS, Overgaard J, Rose C, Andersson M, Bach F, et al. Postoperative radiotherapy in high-risk premenopausal women with breast cancer who receive adjuvant chemotherapy. Danish Breast Cancer Cooperative Group 82b Trial. N Engl J Med. 1997. 337:949–955.

20. Overgaard M, Jensen MB, Overgaard J, Hansen PS, Rose C, Andersson M, et al. Postoperative radiotherapy in high-risk postmenopausal breast-cancer patients given adjuvant tamoxifen: Danish Breast Cancer Cooperative Group DBCG 82c randomised trial. Lancet. 1999. 353:1641–1648.

21. Handley RS. Carcinoma of the breast. Ann R Coll Surg Engl. 1975. 57:59–66.
22. Galper S, Recht A, Silver B, Manola J, Gelman R, Schnitt SJ, et al. Factors associated with regional nodal failure in patients with early stage breast cancer with 0-3 positive axillary nodes following tangential irradiation alone. Int J Radiat Oncol Biol Phys. 1999. 45:1157–1166.

23. Buchholz TA. Internal mammary lymph nodes: to treat or not to treat. Int J Radiat Oncol Biol Phys. 2000. 46:801–803.

24. Harris EE, Hwang WT, Seyednejad F, Solin LJ. Prognosis after regional lymph node recurrence in patients with stage I-II breast carcinoma treated with breast conservation therapy. Cancer. 2003. 98:2144–2151.

25. Poortmans PM, Venselaar JL, Struikmans H, Hurkmans CW, Davis JB, Huyskens D, et al. The potential impact of treatment variations on the results of radiotherapy of the internal mammary lymph node chain: a quality-assurance report on the dummy run of EORTC Phase III randomized trial 22922/10925 in Stage I--III breast cancer (1). Int J Radiat Oncol Biol Phys. 2001. 49:1399–1408.

26. Olivotto IA, Chua B, Elliott EA, Parda DS, Pierce LJ, Shepherd L, et al. A clinical trial of breast radiation therapy versus breast plus regional radiation therapy in early-stage breast cancer: the MA20 trial. Clin Breast Cancer. 2003. 4:361–363.

27. Stemmer SM, Rizel S, Hardan I, Adamo A, Neumann A, Goffman J, et al. The role of irradiation of the internal mammary lymph nodes in high-risk stage II to IIIA breast cancer patients after high-dose chemotherapy: a prospective sequential nonrandomized study. J Clin Oncol. 2003. 21:2713–2718.

28. Andry G, Suciu S, Vico P, Faverly D, Andry-t'Hooft M, Verhest A, et al. Locoregional recurrences after 649 modified radical mastectomies: incidence and significance. Eur J Surg Oncol. 1989. 15:476–485.




 PDF
PDF ePub
ePub Citation
Citation Print
Print







 XML Download
XML Download