Abstract
Purpose
A CXCR4/stroma derived factor-1α (SDF-1α, CXCL12) interaction is involved in many metastatic cancer mechanisms, including breast cancer. The primary objectives of this study were to investigate the correlation between CXCR4 and axillary lymph node metastasis and to clarify the interaction between CXCR4 in primary tumor cells and SDF-1α in metastatic lymph nodes. An analysis of the correlation between CXCR4, SDF-1α and clinicopathologic features was also performed.
Methods
Representative areas from 44 invasive ductal carcinomas were selected for construction of tissue microarrays using a 5 mm punch. Breast cancers (n=44), metastatic axillary lymph nodes (n=18) and non-metastatic axillary lymph nodes (n=26) were immunohistochemically stained for CXCR4, SDF-1α, estrogen receptor (ER), progesterone receptor (PR) and HER2. The parameters of age, tumor size, nuclear grade, histologic grade, lymph node status and pathologic node (pN) stage pN0 to pN3 were evaluated.
Results
CXCR4 expression was negatively correlated with increased age (p=0.005) and positively correlated with a large tumor size (p=0.043) and PR expression (p=0.027). CXCR4 expression was not correlated with metastatic lymph nodes (p=0.079) and SDF-1α expression in metastatic lymph nodes (p=0.062). However, CXCR4 nuclear positivity is correlated with lymph node metastasis (p=0.044). SDF-1α was not correlated with any clinicopathologic feature in a statistically significant manner.
Breast cancer, the most common malignancy in women, is characterized by a distinct pattern of metastases involving regional lymph nodes, lung, bone, and liver. Even though early stage breast cancers are not life threatening, metastatic breast cancer is responsible for the majority of cancer-related deaths. Metastasis is the result of several sequential steps and represents a highly organized, nonrandom, and organ-selective process.(1) Chemokines and their respective receptors regulate chemotaxis and the transendothelial migration of leukocytes during immune and inflammatory reactions.(2) Although different kinds of cancer cells express different chemokine receptors, the most common expressed on human cancer cells is the CXC chemokine receptor CXCR4, which has been found in at least 23 different types of human cancer, including those of epithelial, mesenchymal, and hematopoietic origin.(3) Expression of CXCR4 has been demonstrated in breast cancer, melanoma, some leukemias,(4) prostate and ovarian cancers,(5) B-cell lymphomas,(6) primary pancreatic cancer cell lines,(7) renal cell carcinoma(8) and bladder cancer.(9) CXCR4 is activated by its only known ligand, stromal cell-derived factor-1α (SDF-1α). Activation of CXCR4 induces signal transduction pathways in cancer cells that are important in the cancer metastasis procedure with involvement in cytoskeletal rearrangement, actin polymerization,(4) pseudopodia formation, firm adhesion to endothelial cells, directional migration and proliferation.(10) Dewan et al.(11) found that the SDF-1 receptor CXCR4 was over-expressed in human breast cancer tissues and was linked to the nodal spread of breast cancer. Also, CXCR4-expressing breast cancer cells aggressively metastasized in secondary organs. Sun et al.(12) found that SDF-1α was expressed in all lymph cells in lymph nodes, including metastatic and non-metastatic, suggesting that the expression of SDF-1α in lymph nodes probably participates in CXCR4 signal-directed migration of breast cancer cells into the lymph system. SDF-1 was specifically expressed in malignant cell types including breast cancers, pancreatic cancers, glioblastomas and oral squamous cell carcinoma.(6,13) Neutralization of SDF-1/CXCR4 interaction significantly inhibits the metastasis of breast cancer cells to distant organs.(11) Helbig et al.(14) found that studies using mouse models of breast cancer and specimens from human tumors had emphasized the importance of the tumor microenvironment in controlling the SDF-1/CXCR4 signaling pathway.
The primary objectives of this study were to investigate the correlation between CXCR4 and axillary lymph node metastasis and to clarify the interaction of CXCR4 in primary tumor cells and SDF-1α in metastatic lymph nodes. An analysis of the correlation between CXCR4, SDF-1α, and clinicopathologic features was also performed.
Forty-four invasive ductal carcinomas, which were surgically resected in the Department of Surgery and diagnosed in the Department of Pathology at the Catholic University Daejeon St. Mary's Hospital from January 2000 through January 2009, were obtained. Ipsilateral axillary lymph node dissection was performed in all cases.
Clinicopathologic parameters were evaluated, including age at initial diagnosis, tumor size, nuclear grade, histologic grade, lymph node metastasis and pathologic node (pN) stage pN0 to pN3. The histologic grade was assessed according to a modified Bloom-Richardson-Scarff grading system.
Hematoxylin-eosin stained slides were reviewed for each case and areas of interest were marked on each slide. The arrays were constructed using a 5 mm punch on a Bee-Cher arrayer. Corresponding regions were circled on the "donor" paraffin block using a marker pen. Samples were then arrayed on a "recipient" blank block. A total of 19 samples were available for 1 array.
Immunohistochemical staining for CXCR4 (Abcam, Cambridge, UK), SDF-1α (Abcam, Cambridge, UK), estrogen receptor (ER) (Immunotech, Paris, France), progesterone receptor (PR) (Immunotech, Paris, France) and HER2 (DAKO, Copenhagen, Denmark) were performed on TMA sections. Briefly, 4 µm thick sections were cut from paraffin blocks. The wax was removed from the paraffin sections using xylen, followed by rehydration through a series of graded alcohols, placement in 10 mL of citrate buffer, and submitted for heat retrieval using a vapor lock for 30 min. After heating, the slides were allowed to cool to room temperature then briefly washed with tris-buffered saline (DAKO, Copenhagen, Denmark). Then the slides were immersed in a 3% H2O2 solution to block endogenous peroxidase activity, and incubated for 1 hr with primary antibodies for ER, PR and HER2. Primary antibodies for CXCR4 and SDF-1α were incubated overnight at 4℃. After incubation, slides were stained with peroxidase-labeled streptavidin-biotin complex (Zymed, San Francisco, USA) and counterstained with Mayer's hematoxylin.
CXCR4 was considered to be positive when breast cancer cells showed the cytoplasm, the nucleus, and/or the complete membrane as a brown color. The staining pattern of tumors for CXCR4 was defined as cytoplasmic expression, nuclear expression or membranous expression using the criteria in Table 1.(15,16)
SDF-1α was considered to be positive if more than moderate cytoplasmic staining of malignant cells, but not nuclei, was observed. If the sum of the proportion score and the intensity score(17) was more than 3, ER and PR were considered to be positive. Only cells with a membranous staining score 3 were considered positive for HER2.
We performed immunohistochemical staining for both ER and PR three times because of a low percentage for positivity.
The SPSS for Window 12 software package (SPSS Inc., Chicago, USA) was used for statistical analysis.
The tumor size, nuclear grade, histologic grade, and pathology of lymph nodes (pN) of the clinicopathologic features were analyzed using the chi-square test. Fisher's exact test was evaluated used for the remaining clinicopathologic features. The intergroup difference in CXCR4 and tumor size was evaluated by Student's t-test. Pearson's r correlation was also used to estimate correlation coefficients between hormone receptors and histologic or nuclear grade, between ER expression and HER2 expression, and between age and CXCR4 expression. p-values of less than 0.05 were considered statistically significant.
In total, 44 invasive ductal carcinomas were analyzed (Figure 1A). Patient age ranged from 28-77 yr with a mean age of 52 yr. CXCR4 expression in breast cancer was negatively correlated with increased age (≥52 yr) (p=0.005), and positively correlated with a larger tumor size (p=0.043 analyzed using the Fisher's exact test and p=0.020 evaluated by Student's t-test) and PR expression (p=0.027). CXCR4 expression in breast cancer was not correlated with metastatic lymph nodes (p=0.079) nor SDF-1α expression in metastatic lymph nodes (p=0.062) (Tables 2, 3).
The staining patterns of CXCR4 in breast cancer varied as follows: no staining (19 cases), nuclear expression (15 cases, Figure 1B), cytoplasmic expression (9 cases, Figure 1C) and membranous expression (1 case, Figure 1D).
CXCR4 nuclear expression in breast cancer appeared more frequently in lymph node-positive tumors (55.6%, p=0.023) than in lymph node-negative tumors (19.2%). CXCR4 cytoplasmic expression in breast cancer was not correlated with lymph node metastasis (Table 4). CXCR4 expression was absent or minor in normal breast epithelia.
Breast cancer cells were stained by SDF-1α in primary breast cancers (Figure 1E) and in the lymph nodes (Figure 1F). Lymphoid cells were also stained by SDF-1α in primary breast cancers and in the lymph nodes. SDF-1α expression was negative in normal ductal and lobular cells. SDF-1α in breast cancer was not correlated with any clinicopathologic features (Table 2).
Coexpression of ER and PR was present in 10 breast cancers. ER positivity (Figure 2A) was not correlated with the expression of CXCR4 and SDF-1α in breast cancers. PR positivity (Figure 2B) was correlated with CXCR4 positivity in primary breast cancers (p=0.027) and not correlated with SDF-1α in metastatic lymph nodes (Table 2).
ER or PR expression was negatively correlated with histologic grade (p=0.017, r=0.428 and p=0.017, r=0.391). ER or PR expression was negatively correlated with nuclear grade (p=0.029, r=0.397 and p=0.014, r=0.392). ER expression trended toward a negative correlation with HER2 expression (p=0.61, r=0.282).
The mechanism of metastasis to lymph nodes is not well understood. Recent studies have shown that CXCR4, CCR7, and c-MET are involved in directing tumor cells to lymph nodes.(7) Activation of SDF-1α/CXCR4 increases secretion of MMP2 and MMP9. These signaling events result in changes in cellular motility and invasive and adhesive properties in breast cancer cells. Collectively, these events may lead tumor cells to metastasize to lymph nodes. Experimental studies have suggested that several tumor types metastasize to distant organs, such as the lungs and bones, via the CXCR4-mediated signaling pathway.(3)
Sun et al.(12) found that SDF-1α is involved in CXCR4-stimulated directed metastasis of cancer cells. CXCR4 protein expression increases with tumor aggressiveness, and levels of SDF-1 are higher in metastatic lesions than in primary tumor sites. Tumor invasion and metastasis involve complex procedures in which the invasion of tumor cells and passage through the basement membrane, fibroblast monolayers and endothelial cells are regarded as key processes before the tumor cells migrate to target organs. Directed migration of tumor cells stimulated by activation of CXCR4 is dependent on an SDF-1α gradient.(9) It has been reported that 100-1,000 ng/mL of SDF-1α is an optimal concentration to stimulate the migration of monocytes, lymphocytes, endothelial cells, and tumor cells. By using time-lapse monitoring of the locomotion of individual cells, it was shown that SDF-1α accelerates the motility of several different kinds of human tumor cells, including breast cancer, rhabdomyosarcoma and small lung cancer cell lines.(10) The mechanisms by which SDF-1α effects tumor cell motility include changes/rearrangement of the cytoskeletal proteins, augmentation of the number and thickness of F-actin bundles, and calcium flux.(11) Based on a Matrigel invasion model, SDF-1α is probably also involved in cancer cell growth and survival, in addition to stimulating cancer cell migration. Because cancer cells experience little growth when deprived of a blood supply during metastasis to distant sites, SDF-1α probably helps in the survival and spread of cancer cells by stimulating their proliferation. CXCR4/SDF-1α participates in vivo and directs migration in vitro.
Tumor cell metastasis may be correlated with attraction of SDF-1α to the metastatic organ. Our results showed that CXCR4 expression in breast cancers tended toward a positive correlation with SDF-1α expression in lymph nodes-positive tumors, even though the correlation was not statistically significant (p=0.062).
A high level of cytoplasmic CXCR4 expression occurs more commonly, but not significantly, in lymph node-positive tumors.(15,18) The results of Woo et al.(19) showed that expression of CXCR4 in the cytoplasm is not associated with axillary lymphatic metastasis. CXCR4 is a membrane-bound G-protein-coupled receptor that can be internalized together with its ligand SDF-1 upon activation. Therefore, cytoplasmic reactivity, especially when co-expressed together with SDF-1, may reflect receptor internalization and, thus, a state of activation of CXCR4.(20) Predominantly nuclear CXCR4 staining was more likely to be statistically significant in lymph node-negative tumors.(15,18) Su et al.(21) reported that a high level of CXCR4 nuclear expression was not associated with lymph node involvement. Spano et al.(22) pointed out that in non-small cell lung carcinoma, CXCR4-positive nuclear staining might be associated with survival. They opined that the nuclear retention of CXCR4 decreases cell proliferation and metastasis by inhibiting the interaction with SDF-1α. Shim et al.(23) stated that SDF-1 induces both down-regulation of membranous CXCR4 expression and degradation of the internalized CXCR4 receptors via the lysosome pathway. These results suggest that a reduction in CXCR4 membrane staining in metastatic lymph nodes is associated with progression of breast cancer metastasis.
Our results showed that CXCR4 nuclear positivity is correlated with lymph node metastasis and that CXCR4 expression trended toward a positive correlation with metastatic lymph nodes (p=0.079). These results indicate that different patterns of CXCR4 expression in cells probably lead to differences in the biological behavior of the respective tumor cells. Evaluation of the expression patterns will help predict lymph node metastasis and clinical outcomes.
Woo et al.(19) found that neither cytoplasmic nor nuclear CXCR4 expression shows a significant correlation with other characteristics including age, tumor stage, node stage, tumor-node-metastasis (TNM) stage, histological grade, ER, PR, or HER2 status.
We found that the positivity of CXCR4 in breast cancer is negatively correlated with increased age (≥52 yr). Assuming a normal age distribution in breast cancer occurrance, the sample mean (52 yr) of observed ages is considered to be an estimate of the population mean. The p-value and the correlation coefficient (Pearson's r) for increased age (≥52 yr) and CXCR4 positivity were 0.005 and -0.445, respectively. These show an inverse relationship between increased age (≥52 yr) and CXCR4 positivity.
High-intensity immunohistochemical staining for CXCR4 was associated with large tumors in papillary thyroid carcinomas (p=0.02)(24) and CXCR4 was also expressed strongly in large tumors of non-small cell lung cancers (>3 cm, p=0.042).(25)
Woo et al.(19) found that among 105 breast cancers, 26 cases (24.8%) were classified as T1, 63 cases (60%) as T2 and 16 cases (15.2%) as T3. Nuclear and cytoplasmic CXCR4 were not correlated with tumor size. However, our results showed that a larger tumor size was correlated with CXCR4 expression.
Salvucci et al.(26) found an inverse correlation between cytoplasmic CXCR4 staining and ER positivity, and no correlation between either cytoplasmic or nuclear CXCR4 staining and PR positivity. A negative estrogen and a progesterone receptor status were significantly correlated with a high level of nuclear CXCR4 expression and with lymph node metastasis. Furthermore, there was a significant correlation between a high level of nuclear CXCR4 expression and lymph node metastasis and receptor negative estrogen and the progesterone status.(19) We found that CXCR4 was positively correlated with PR expression but wasn't with ER positivity.
Recently, the Breast Pathology Study Group of the Korean Society of Pathologist collected 1,198 breast carcinoma samples from seven university hospitals and performed ER staining with the three antibodies, 1D5, 6F11 and SP1. The ER positivity rates were 68.6% for SP1, 59.5% for 1D5 and 54.8% for 6F11.(27) In our study, the ER expression rate in breast cancers was 36.4% with the 1D5 estrogen receptor clone. Also, among the other 72 excised breast cancers without lymph node dissection, the ER expression rate was 35 cases (48.6%). In our study, negative ER or PR expression was correlated with a high histologic grade or high nuclear grade. These ER expression rates may be attributable to high histologic grade cancers, high nuclear grade cancers, different kinds of antibodies used, differences between the products of manufacturing companies, the duration of fixation, the buffer solutions used, tumor heterogeneity, or a small number of cases.
An evaluation of young age, large tumor size and PR expression helps predict lymph node metastasis and poor prognosis. Expression of CXCR4 nuclear positivity is correlated with a poor prognosis. A larger study is needed to verify these results and further study is needed to determine the clinical significance of SDF-1α/CXCR4 expression.
Figures and Tables
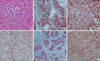 | Figure 1H&E and immunohistochemical staining in invasive ductal carcinoma. Small irregular shaped glands and nests infiltrate the stroma (H&E stain, ×200) (A). Immunohistochemical staining for CXCR4 is positive in cytoplasm and nucleus (B, ×400), cytoplasm (C, ×200), and membrane (D, ×400). SDF-1α is positive in the cytoplasm in primary breast carcinoma (E, ×200) and metastatic lymph node (F, ×200). |
 | Figure 2Immunohistochemical staining in invasive ductal carcinoma. Immunohistochemical staining for estrogen receptor (A, ×200) and progesterone receptor (B, ×400) are positive in the nucleus. HER2 is positive in the membrane (C, ×200). |
References
1. Nicolson GL. Paracrine and autocrine growth mechanisms in tumor metastasis to specific sites with particular emphasis on brain and lung metastasis. Cancer Metastasis Rev. 1993. 12:325–343.

2. Möhle R, Schittenhelm M, Failenschmid C, Bauts F, Kratz-Albers K, Serve H, et al. Functional response of leukaemic blasts to stromal cell-derived factor-1 correlates with preferential expression of the chemokine receptor CXCR4 in acute myelomonocytic and lymphoblastic leukaemia. Br J Haematol. 2000. 110:563–572.

3. Kang H, Watkins G, Douglas-Jones A, Mansel RE, Jiang WG. The elevated level of CXCR4 is correlated with nodal metastasis of human breast cancer. Breast. 2005. 14:360–367.

4. Kijima T, Maulik G, Ma PC, Tibaldi EV, Turner RE, Rollins B, et al. Regulation of cellular proliferation, cytoskeletal function, and signal transduction through CXCR4 and c-Kit in small cell lung cancer cells. Cancer Res. 2002. 62:6304–6311.
5. Balkwill F. The significance of cancer cell expression of the chemokine receptor CXCR4. Semin Cancer Biol. 2004. 14:171–179.

6. Uchida D, Begum NM, Almofti A, Nakashiro K, Kawamata H, Tateishi Y, et al. Possible role of stromal-cell-derived factor-1/CXCR4 signaling on lymph node metastasis of oral squamous cell carcinoma. Exp Cell Res. 2003. 290:289–302.

7. Fernandis AZ, Prasad A, Band H, Klosel R, Ganju RK. Regulation of CXCR4 mediated chemotaxis and chemoinvasion of breast cancer cells. Oncogene. 2004. 23:157–167.

8. Pan J, Mestas J, Burdick MD, Phillips RJ, Thomas GV, Reckamp K, et al. Stromal derived factor-1 (SDF-1/CXCL12) and CXCR4 in renal cell carcinoma metastasis. Mol Cancer. 2006. 5:56.

9. Scotton CJ, Wilson JL, Milliken D, Stamp G, Balkwill FR. Epithelial cancer cell migration: a role for chemokine receptors? Cancer Res. 2001. 61:4961–4965.
10. Adams GB, Chabner KT, Foxall RB, Weibrecht KW, Rodrigues NP, Dombkowski D, et al. Heterologous cells cooperate to augment stem cell migration, homing, and engraftment. Blood. 2003. 101:45–51.

11. Dewan MZ, Ahmed S, Iwasaki Y, Ohba K, Toi M, Yamamoto N. Stromal cell-derived factor-1 and CXCR4 receptor interaction in tumor growth and metastasis of breast cancer. Biomed Pharmacother. 2006. 60:273–276.

12. Sun YX, Wang J, Shelburne CE, Lopatin DE, Chinnaiyan AM, Rubin MA, et al. Expression of CXCR4 and CXCL12 (SDF-1) in human prostate cancers (PCa) in vivo. J Cell Biochem. 2003. 89:462–473.

13. Geminder H, Sagi-Assif O, Goldberg L, Meshel T, Rechavi G, Witz IP, et al. A possible role for CXCR4 and its ligand, the CXC chemokine stromal cell-derived factor-1, in the development of bone marrow metastases in neuroblastoma. J Immunol. 2001. 167:4747–4757.

14. Helbig G, Christopherson KW 2nd, Bhat-Nakshatri P, Kumar S, Kishimoto H, Miller KD, et al. NF-kappaB promotes breast cancer cell migration and metastasis by inducing the expression of the chemokine receptor CXCR4. J Biol Chem. 2003. 278:21631–21638.

15. Cabioglu N, Yazici MS, Arun B, Broglio KR, Hortobagyi GN, Price JE, et al. CCR7 and CXCR4 as novel biomarkers predicting axillary lymph node metastasis in T1 breast cancer. Clin Cancer Res. 2005. 11:5686–5693.

16. Tsoli E, Tsantoulis PK, Papalambros A, Perunovic B, England D, Rawlands DA, et al. Simultaneous evaluation of maspin and CXCR4 in patients with breast cancer. J Clin Pathol. 2007. 60:261–266.

17. Harvey JM, Clark GM, Osborne CK, Allred DC. Estrogen receptor status by immunohistochemistry is superior to the ligand-binding assay for predicting response to adjuvant endocrine therapy in breast cancer. J Clin Oncol. 1999. 17:1474–1481.

18. Cabioglu N, Sahin A, Doucet M, Yavuz E, Igci A, Yildirim OE, et al. Chemokine receptor CXCR4 expression in breast cancer as a potential predictive marker of isolated tumor cells in bone marrow. Clin Exp Metastasis. 2005. 22:39–46.

19. Woo SU, Bae JW, Kim CH, Lee JB, Koo BW. Significant correlation between nuclear CXCR4 expression and axillary lymph node metastasis in hormonal receptor negative breast cancer. Ann Surg Oncol. 2008. 15:281–285.

20. Liu F, Lang R, Wei J, Fan Y, Cui L, Gu F, et al. Increased expression of SDF-1/CXCR4 is associated with lymph node metastasis of invasive micropapillary carcinoma of the breast. Histopathology. 2009. 54:741–750.

21. Su YC, Wu MT, Huang CJ, Hou MF, Yang SF, Chai CY. Expression of CXCR4 is associated with axillary lymph node status in patients with early breast cancer. Breast. 2006. 15:533–539.

22. Spano JP, Andre F, Morat L, Sabatier L, Besse B, Combadiere C, et al. Chemokine receptor CXCR4 and early stage non-small cell lung cancer: pattern of expression and correlation with outcome. Ann Oncol. 2004. 15:613–617.

23. Shim HS, Lau SK, Devi S, Yoon Y, Cho HT, Liang Z. Lower expression of CXCR4 in lymph node metastases than in primary breast cancers: Potential regulation by ligand-dependent degradation and HIF-1a. Biochem Biophys Res Commun. 2006. 346:252–258.

24. Wagner PL, Moo TA, Arora N, Liu YF, Zarnegar R, Scognamiglio T, et al. The chemokine receptors CXCR4 and CCR7 are associated with tumor size and pathologic indicators of tumor aggressiveness in papillary thyroid. Ann Surg Oncol. 2008. 15:2833–2841.

25. Song JS, Jung JK, Park JC, Kim DK, Jang SJ. Association of CXCR4 expression with metastasis and survival among patients with non-small cell lung cancer. Korean J Pathol. 2008. 42:358–364.
26. Salvucci O, Bouchard A, Baccarelli A, Deschênes J, Sauter G, Simon R, et al. The role of CXCR4 receptor expression in breast cancer: a large tissue microarray study. Breast Cancer Res Treat. 2006. 97:275–283.

27. Bae YK, Gong GY, Kang J, Lee AW, Cho EY, Lee JS, et al. Estrogen receptor expression in Korean breast carcinoma and comparison of three anti-ER antibodies. 2009. In : 61th fall annual meeting of Korean Society of Pathologists; –43. abstract #4.




 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download