Abstract
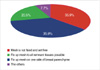
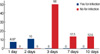
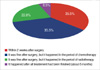
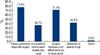
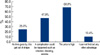
The aim of this study is to investigate the use of absorbable mesh in breast surgery in Korea. We conducted a survey from members of Korea Breast Cancer Society by phone, E-mail, and notice on the website from 6th to 20th April 2009. A total of 54 breast surgeons had responded to the survey. Of these, 40 surgeons (74.1%) had used absorbable mesh during breast surgery, with Vicryl mesh® being the choice of every surgeon and Interceed® having been used by 36 (90%) of the surgeons. In responding to the indications for mesh use, 26 surgeons (65%) indicated that mesh use was effective when a deformity was expected regardless of T stage. Contraindications for mesh use principally included existing patients' comorbidity such as a wound healing problem, diabetes mellitus and immunocompromised condition. Thirty one surgeons (77.5%) had experienced an infection in the mesh insertion site. However, on a case basis, only 39 of 843 cases (4.6%) had resulted in an infection. In the follow up after mesh use, 33 of the 37 responding surgeons (89.2%) used breast ultrasonography. Nineteen of the 38 respondents (50%) replied that the mesh was absorbed in 6 months and it did not confuse diagnostic imaging. The cited merits of mesh included maintenance of breast shape following surgery (n=38/49, 77.6%) and ease of surgical use (n=35/49, 71.4%). However, the high price of mesh was cited as a disadvantage by 33 of the 48 respondents (68.8%). In summary, survey results mentioned above show that surgical mesh use in breast surgery is increasing by times and the procedures greatly varies by surgeons. Thereby, we suggest that a guideline for mesh use should be made in the near future.
Figures and Tables
References
1. The Korean Breast Cancer Society. Nationwide Korean breast cancer data of 2004 using breast cancer registration program. J Breast Cancer. 2006. 9:151–161.
2. Ko SS. Korean Breast Cancer Society. Chronological changing patterns of clinical characteristics of Korean breast cancer patients during 10 years (1996-2006) using nationwide breast cancer registration on-line program: biannual update. J Surg Oncol. 2008. 98:318–323.

3. Fisher B, Bauer M, Margolese R, Poisson R, Redmond C, Fisher E. Five-year results of a randomized clinical trial comparing total mastectomy and segmental mastectomy with or without radiation in the treatment of breast cancer. N Engl J Med. 1985. 312:665–673.

4. Eom TI, Kim BS, Koo BY, Kim JW, Lim YA, Lee HH, et al. The use of a corrective procedure with vicryl mesh for oncoplastic surgery of the breast. J Breast Cancer. 2009. 12:36–40.

5. Clough KB, Lewis JS, Fitoussi A, Faucoult MC. Oncoplastic techniques allow extensive resection for breast-conserving therapy of breast carcinomas. Ann Surg. 2003. 237:26–34.

6. Ohuchi N, Harada Y, Ishida T. Breast conserving surgery for primary breast cancer: immediate volume replace using lateral tissue flap. Breast Cancer. 1997. 4:59–65.
7. Rietjens M, Urban CA, Rey PC, Mazzarol G, Maisonneuve P, Garusi C, et al. Long-term oncological results of breast conservative treatment with oncoplastic surgery. Breast. 2007. 16:387–395.





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download