Abstract
Purpose
Human epidermal growth factor receptor-2 (HER-2)/neu amplification affects the cell proliferation through the modulation of multiple G1 cell cycle regulators in breast tumor cells. We performed this study to investigate whether retinoblastoma protein (pRB) and p27Kip1 were differently expressed according to the HER2 amplification status in human breast cancer.
Methods
HER2 amplification was assayed by fluorescence in situ hybridization and the expression of cell cycle regulators were assayed by immunohistochemistry on 153 consecutive invasive breast cancers. The proliferative activity of breast cancer was analyzed according to the HER2 amplification and cell cycle protein expression status.
Results
HER2 amplification was observed in 39 (25.5%) of 153 breast cancers. In the HER2 amplified breast cancers, the pRB expression was significantly increased (p=0.011) whereas there was no significant relationship between HER2 amplification and p27Kip1 expression. There was an inverse correlation between pRB expression and Ki-67 labeling index in the HER2 amplified breast cancers (p=0.036). In contrast, Ki67 labeling index was significantly decreased as p27Kip1 expression increased in HER2 non-amplified breast cancers (p=0.028). In HER2 non-amplified breast cancers, we could not observe any association between the pRB expression and Ki67 labeling index.
Conclusion
The proliferation of the breast cancers was associated with pRB expression in HER2 amplified tumors whereas it was associated with p27Kip1 expression in HER2 non-amplified tumors. The results of the current study indicate that the cell proliferative activity of the breast cancer is under different growth signal pathways according to HER2 amplification status.
Human epidermal growth factor receptor-2 (HER2) overexpression resulting from HER2 gene amplification has been shown in 20-30% of human breast cancers and is associated with poor clinical outcome even with systemic chemotherapy.(1) HER2 gene amplification results in the overexpression of HER2 receptor and the activation of HER2 receptor results in the activation of a complex network of signal pathways that mediate enhanced cell proliferation.(2) Better understanding of the mechanism by which HER2 regulates cell signal pathways may help to determine the biologic role of HER2 in the breast cancer.
A series of in vitro studies have indicated that the effects of HER2 on the cell proliferation involve the modulation of G1 cell cycle regulators such as cyclin D1 and p27Kip1 through multiple signaling pathways.(3,4) SKBR3 cells accumulate in G1 upon down-regulation of HER2 and HER2 controls G1 to S transition via phosphorylation of retinoblastoma protein (pRB). Inactivating phosphorylation of pRB seems to be mediated by the interactions between cyclin D1/E and p27Kip1 proteins in the study.(3)
The p27Kip1 was originally discovered as a cyclin-dependent kinase (cdk) inhibitor induced by extracellular antimitogenic signals.(5,6) Rapid elimination of p27Kip1 is probably a prerequisite for the activation of cyclin/cdk complex through cell cycle progression. In vitro data indicated that sequestration of p27Kip1 via ternary complex of cyclin D-cdk4/6-p27Kip1 precedes sequential activation of cyclin E-cdk2 complex in G1-S transition of the cell cycle.(7,8) Overexpression of HER2 increases the turnover of p27Kip1 in HER2 transfected MCF-7 cells whereas inhibition of HER2 increases nuclear levels of p27Kip1 and its association with nuclear cdk2.(4) The p27Kip1 modulation seems to be a part of growth signaling pathway driven by HER2.
In this study, we analyzed the expression profiles of pRB and p27Kip1 according to HER2 amplification status on tissue microarray (TMA) of 153 consecutive breast cancers. Changes of cell proliferation index according to the expression of the studied cell cycle regulators were also analyzed.
Tissue from 153 consecutive breast cancer patients who underwent curative surgical treatment and adjuvant treatment between January 1994 and December 1996 were collected. The representative tumor blocks were selected and transplanted to the tissue array blocks.
Recipient blocks were made with purified agar in 3.8×2.2 frames. Holes with 2 mm in each size were made on the recipient blocks by core needle and agar core was discarded. Donor blocks were prepared after thorough evaluation of H & E slides. Representative cancer portions retrieved from matching donor blocks were transplanted to the recipient blocks using 2 mm core needle. Recipient blocks were framed in the mold which is used to frame conventional paraffin block, and then paraffin was added to the frame. Three µm sections were cut from the recipient blocks using an adhesive coated slide system (Instrumedics Inc., Hackensack, USA) supporting the cohesion of the 2 mm array elements on the glass.(9)
Two-color FISH was done on a 3 µm-thick consecutive microarray sections. Before hybridization, the sections were deparaffinized, air dried, and dehydrated in 100% ethanol after incubation at 56℃ for 24 hr. Microarray slides were treated in wash buffer (Vysis Inc., Downers Grove, USA) for 3 min after treatment with 0.2N HCl for 20 min. Pretreatment solution (Vysis Inc., Downers Grove, USA) at 80℃ was applied for 30 min and the slides were washed with purified water. Slides were treated were treated with wash buffer twice for 5 min serially. Immersed slides in Protease solution (Vysis Inc., Downers Grove, USA) at 37℃ was applied for 10 min and the slides were washed with wash buffer at 45-50℃ and air dried. Slides were fixed in 10% buffered formalin for 10 min and then washed with wash buffer at 45-50℃. For denaturation, slides were immersed in denaturation solution (Vysis Inc., Downers Grove, USA) for 5 min at 72℃ followed by dehydration with 70%, 85% and 100% ethanol serially at 45-50℃. For hybridization, 20 µL LSI HER-2/CEP17 probe (PathVision™, Vysis Inc., Downers Grove, USA) was applied and a coverslip was applied over the probe. After overnight hybridization at 37℃ in a humidified chamber, the slides were washed with 72℃ post-hybridization wash buffer (PHWB, Vysis Inc., Downers Grove, USA) for 2 min. Nuclei were counterstained with 20 µL 4,6-diamino-2-phenylindole (DAPI, Vysis Inc., Downers Grove, USA). The centromere 17 (CEP) and HER2 copy numbers were counted in the predominant tumor cell population.
Hybridization signals were enumerated by the ratio of orange signals for HER2 to green signals for CEP17 in morphologically intact and non-overlapping nuclei. At least two times more HER2 signals than CEP17 signals in the tumor cells were considered as criteria for HER2 amplification.
After deparaffinization and dehydration of the slides, heat induced epitope retrieval was done at 95℃ for 15 min. TMA slides were stained with specific antibodies to p27Kip1 and pRB; mouse monoclonal antibody DCS-72. F6 for p27Kip1 protein (Santa Cruz Biotechnology, Santa Cruz, USA), mouse monoclonal antibody to pRB (Neo-Markers, Fremont, USA) using the avidin-biotin complex- immunoperoxidase method. Scoring was performed by microscopically reviewing the slides to estimate the percent of cancer cells with nuclear staining. The interpretation for pRB expression was made as negative if no cell or less than 10% of cells were stained in nuclei, intermediate category if stained in 10-50% of the observed cancer cells, and high category if stained in more than 50% of the cancer cells. The statistical significance was maintained when we dichotomized the expression status of pRB, thus the cases of intermediate category were merged with those of high category in data analyses. p27kip1 expression was assessed by dichotomizing at 50% as a cutoff value because this cutoff level has been widely used in most studies evaluating p27Kip1 expression in breast carcinoma and median value from the current study was also 50%. The histologic grading of all carcinomas followed the Nottingham modification of the Scarff-Bloom-Richardson scoring system.(10) Review of original pathology reports yielded tumor size and axillary lymph node status, but not in all cases.
4. Statistics
Results of IHC for molecular markers were merged and analyzed. The chi-square test and Fisher's exact test were used for data analyses, and the correlation between molecular markers was estimated by Spearman's correlation coefficient. Calculations were performed with the use of SPSS statistical software, version 11.5. The differences were considered significant when p-values were 0.05.
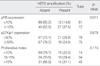
HER2 amplification was observed in 39 (25.5%) of 153 breast cancers. We analyzed the HER2 amplification according to the various clinical and biologic characteristics of the studied patients. The frequency of HER2 amplification was significantly increased in high grade tumors (p=0.023), but there was no statistically significant association between HER2 amplification and other variables such as the status of estrogen receptor (ER) expression and lymph node metastasis (Table 1).
The expression of p27Kip1 and pRB was assessed on the consecutive sections of TMA blocks. pRB was expressed in 72 tumors (47.1%). pRB was expressed in 45 (39.5%) of 114 tumors without HER2 amplification whereas it was expressed in 27 (69.2%) of 39 tumors with HER2 amplification (Table 2). The frequency of pRB expression was significantly increased in HER2 amplified breast cancers. Assay for p27Kip1 expression was performed on the consecutive sections of same array blocks. p27Kip1 expression was preserved in 75 (49%) of 153 tumors. p27Kip1 expression was preserved in 57 (50%) of 114 tumors without HER2 amplification whereas its expression was preserved in 18 (46.2%) of 39 HER2-amplified tumors. There was no significant relationship between HER2 amplification and p27 expression.
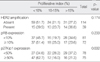
The PI of the individual tumor was assessed by Ki67 labeling index and the change of PI was analyzed according to the expression of the studied cell cycle regulators. The distribution of PI was less than 10% in 74 tumors (49.0%), between 10-15% in 34 tumors (21.2 %), and more than 15% in 45 tumors (29.8%). We divided the PI into 3 categories as low (<10%), intermediate (10-15%), and high (>15%). When the change of PI was analyzed according to HER2 amplification status, PI was labeled more than 15% in 31 (27.2%) of 114 tumors without HER2 amplification, whereas it was increased in 14 (36.8%) of 39 tumors with HER2 amplification. There was a trend that PI was increased in HER2-amplified tumors and the finding was similar when the PI was analyzed as 3 categories, but the difference was not significant statistically (Table 3).
PI change was analyzed according to the pRB expression. PI was increased in 16 (19.7%) at the intermediate category and was increased in 28 (34.6%) at the highcategory of 81 tumors without the pRB-expression. In contrast, PI was increased in 18 (25.0%) at the intermediate category and was increased in 17 (23.6%) at the high category of 72 pRB-expressing tumors.
Of 78 tumors with decreased p27Kip1 expression, PI was increased in 22 (28.2%) at the intermediate category and was increased in 29 (37.2%) at the high category. Of 75 tumors in which the p27Kip1 expression was well preserved, PI was increased in 12 (16.0%) at the intermediate category and was increased in 16 (21.3%) at the high category. PI of the breast cancer was significantly decreased in the p27Kip1-expressing tumors (p=0.032).
We analyzed the change of PI according to the HER2 amplification status. In 39 HER2-amplified tumors, PI was increased in 1 (8.3%) at intermediate category and 8 (66.7%) at high category in 12 pRB negative tumors. In contrast, PI was increased in 9 (33.3%) at intermediate category and 6 (22.3%) at high category in 27 pRB expressing tumors (Table 4). Degree and frequency of PI increase was significantly decreased in the pRB expressing tumors (p=0.036). The change of PI was also analyzed according to the p27Kip1 expression, but the association between PI and p27Kip1 was not observed in the HER2 amplified tumors (Table 4).
In 114 HER2 non-amplified tumors, PI was increased in 16 tumors (28.1%) at intermediate category and 21 tumors (36.8%) at high category in the p27Kip1 repressed tumors. In contrast, PI was increased in 8 tumors (14.1%) at intermediate category and 10 tumors (17.5%) at high category in the 57 tumors with p27Kip1 preservation (Table 5). The PI was significantly decreased in the tumors with p27kip1 expression. The association between pRB expression and PI was not observed in these tumors.
pRB was significantly increased in the HER2-amplified tumors in this study, whereas there was no significant association between the HER2 amplification and the expression of p27. HER2 activation results in the activation of signal pathways that mediate the enhanced proliferation of the cells.(2,11) HER2 amplification coupled with the abnormal expression of cell cycle regulators results in the subversion of cell cycle checkpoints and dysregulates the cell proliferation in tumor cells.(12,13) pRB plays a key role as a negative regulator of the G1-S transition in the normal cell cycle and prevents the activation of the transcription of genes required for the S phase by binding with the transcriptional factor such as E2F family.(14) In this study, the pRB expression was positively associated with the HER2 amplification and PI of the breast cancer was significantly decreased with pRB expression in the HER2 amplified tumors. The finding was unexpected one when we consider that pRB expression is known to be down-regulated by HER2 overexpression in vitro study.(3,4) Furthermore, Inactivation of pRB seems to be mediated by the interactions between cyclin D1/E and p27Kip1 proteins in vitro.(3,4) However, the association between pRB expression and the PI was lost in HER2 non-amplified tumors in which the PI was significantly decreased with p27Kip1 expression. The discrepancy between our study and in vitro data can be partially explained by the hypothesis that pRB expression could be increased reciprocally in response to HER2 overexpression. In other words, increased growth signal driven by HER2 overexpression might lead to the increased expression of pRB to counterbalance the excessive growth stimuli. This hypothesis can be supported by our finding that the PI was significantly decreased with increased pRB expression in the HER2 amplified tumors. Our results suggest that the expression profiles of cell cycle regulators in clinical breast cancer are quite different from the in vitro findings. Exact biologic explanation on this discrepancy seems to need more exquisite molecular dissection study.
A number of reports have suggested that HER2 regulates early cell cycle progression by a process that involves p27Kip1 in breast cancer cell lines.(3,14) The overexpression of HER2 increases the turnover of p27Kip1 and inhibition of HER2 increases nuclear level of p27Kip1 and it's the association with nuclear cdk2 in breast cancer cell line SKBR-3.(4) In this cell line, HER2 controls G1 to S transition via cdk2-dependent phosphorylation of pRB and cyclin E/cdk2 activity is mediated by the association with p27Kip1.(3) In our study, p27Kip1 expression was not associated with HER2 amplification and PI was significantly associated with pRB expression but not with p27Kip1 expression in the HER2 amplified tumors. In contrast, no molecules other than p27Kip1 were associated with PI of the breast cancers when analyzed regardless of HER2 amplification. Relatively the low frequency of HER2 amplification might contribute to the result. The finding of this study was an unexpected one considering the aforementioned evidence from the experimental system. In vitro experiment on BT-474 cells, it appeared that additional HER2 driven signals other than destabilization of p27Kip1 were required for transition into S-phase.(4) It is hard to conclude that cell cycle regulators are differently expressed by HER2 status based on our study, since we did not performed the expression assay for all the downstream molecules. However, it is clear that the expression profiles of cell cycle regulators in clinical breast cancer are quite different from in vitro data produced under the well controlled environment. The different associations between HER2 overexpression and downstream regulators such as pRB and p27Kip1 indicate that growth signal transduction pathways in clinical breast cancer might be under more complex controls than in vitro system.
HER2 amplification was significantly associated with the histologic grade of the tumors but not with other clinical or biologic properties in the consecutive 153 breast cancers such as estrogen receptor expression and PI. The PI of the breast cancers was associated with pRB expression in HER2 amplified tumors whereas it was associated with p27Kip1 expression in HER2 non-amplified tumors. The results of this study indicate that the cell proliferative activity of the breast cancer is under different signal pathways according to HER2 amplification status.
Figures and Tables
References
1. Slamon DJ, Clark GM, Wong SG, Levin WJ, Ullrich A, McGuire WJ. Human breast cancer: correlation of relapse and survival with amplification of the HER-2/neu oncogene. Science. 1987. 235:177–182.

2. Riese DJ, Stern DF. Specificity within the EGF family/ErbB receptor family signaling network. Bioessays. 1998. 20:41–48.

3. Neve RM, Sutterluty H, Pullen N, Lane HA, Daly JM, Krek W, et al. Effects of oncogenic ErbB2 on G1 cell cycle regulators in breast tumour cells. Oncogene. 2000. 19:1647–1656.

4. Lenferink AE, Busse D, Flanagan WM, Yakes FM, Arteaga CL. ErbB2/neu kinase modulates cellular p27Kip1 and cyclin D1 through multiple signaling pathways. Cancer Res. 2001. 61:6583–6591.
5. Polyak K, Lee MH, Erdjument-Bromage H, Koff A, Roberts JM, Tempst P, et al. Cloning of p27, a cyclin-dependent kinase inhibitor and a potential mediator of extracellular antimitogenic signals. Cell. 1994. 78:59–66.

6. Toyoshima H, Hunter T. p27, a novel inhibitor of G1 cyclin/cdk protein kinase activity, is related to p21. Cell. 1994. 78:67–74.

7. Perez-Roger I, Kim SH, Griffiths B, Sewing A, Land H. Cyclins D1 and D2 mediate Myc-induced proliferation via sequestration of p27Kip1 and p21Cip1. EMBO J. 1999. 18:5310–5320.

8. Bouchard C, Thieke K, Maier A, Saffrich R, Hanley-Hyde J, Ansorge W, et al. Direct induction of cyclin D2 by Myc contributes to cell cycle progression and sequestration of p27. EMBO J. 1999. 18:5321–5333.

9. Bok SH, Gwag G, Yang KH, Bae BN, Kim KH, Kim HJ, et al. Proliferative markers of breast cancer. J Breast Cancer. 2005. 8:165–171.

10. Elston CW, Ellis IO. Pathological prognostic factors in breast cancer. I. The value of histologic grade in breast cancer: experience from a large study with long-term follow-up. Histopathology. 1991. 19:403–410.

11. Yarden Y, Sliwkowski MX. Untangling the ErbB signaling network. Nat Rev Mol Cell Biol. 2001. 2:127–137.
12. Elledge SJ. Cell cycle checkpoints: preventing an identity crisis. Science. 1996. 274:1664–1672.





 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download