INTRODUCTION
Systemic polyarteritis nodosa usually involves multiple organs including the kidney, heart, skeletal muscle, skin and mesentery, but rarely involves the breast.(1-3) Only 11 cases of systemic or localized polyarteritis involving the breast have been reported in English literature to date. Two cases of localized polyarteritis nodosa of the breast have been reported in Korea.(3, 4) Of the 13 reported cases, 8 were systemic and 5 were localized. Localized polyarteritis nodosa has shown a much better prognosis than systemic ones.(5) We report a case of localized polyarteritis nodosa in a 69-yr-old woman with no systemic symptoms and review previously reported cases of vasculitis of the breast.
CASE
A 69-yr-old woman noticed a gradually increased tenderness of the right breast for 2 months. She had no history of trauma or specific accident. The patient had no symptoms of a generalized disease such as fatigue, fever or weight loss. The patient had no previous medical or familial history.
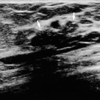
On physical examination, a 2 cm sized mass was identified in the subareolar area of the right breast. No axillary or cervical lymph nodes were palpable. The left breast was unremarkable. Other physical findings were normal with no skin rashes or arthritic changes. Studies for ASO, ANCA or Rheumatoid factor were not performed. Laboratory results showed ESR, Hb/Hct, Wbc count, and hepatitis-associated antigen within the normal limits. An ultrasonogram revealed a 1.8 cm, heterogeneous, and irregular shaped mass-like lesion (Fig 1). Multifocal microcalcifications were identified on mammograhic examination. A presumptive diagnosis of mammary malignancy was made. Surgical excision for the mass was performed. Several tissue sections were prepared from the excised mass.
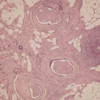
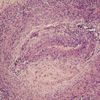
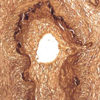
Microscopic findings showed marked vasculitis of the breast parenchyma in a background of mammary duct ectasia (Fig 2). There were several small to medium-sized arteries that were infiltrated by mixed inflammatory cells, including neutrophils, lymphocytes, and eosinophils and some lumens were obliterated by the inflammatory cells and secondary thrombosis (Fig 3). Fragmentation of internal elastic lamina and calcification in vessel were also seen (Fig 4). No giant cell reaction was seen around the vessels or in the breast parenchyma. Adjacent parenchymal ducts were lined by cuboidal or flat epithelium and contained secretory fluid contents. A group of large and coarse microcalcifications were identified in the area of clustered dilated ducts. The stromal tissue was fibrotic with or without an inflammatory reaction. The patient had no symptoms or signs of concurrent vasculitis involving other organs. Biopsy specimens of other tissues were not taken. On the basis of both clinical and histological findings, a diagnosis of localized polyarteritis nodosa with surrounding mammary duct ectasia was made.
In previously reported cases, no patient suffered local recurrence after total excision of the breast lesion. Two months' follow-up revealed no evidence of recurrence or visceral involvement.
DISCUSSION
Breast involvement in polyarteritis nodosa is very rare manifestation.(2) Vasculitis involving the breast has been reported in 13 cases aged between 34 and 78 yr.(2-5) Six of the 13 patients exhibited constitutional symptoms including headache, fatigue, arthralgia, and myalgia.(2) In most cases, patients complained of single or multiple painful breast masses in unilateral or bilateral manifestation. These cases were presumed to be malignant tumors in the context of prevalence of disease and abnormal radiologic findings. Total excision was performed according to systemic or localized manifestations of polyarteritis. If systemic vasculitis is involved, the patient should consider steroid therapy, but localized polyarteritis of the breast has shown a good prognosis following complete excision as a treatment of choice.
Although the present case revealed no systemic symptom and normal limits of erythrocyte sedimentation rate (ESR) level, most of the vasculitis appearing as a tumor-like lesion were associated with constitutional symptoms and elevated ESR.(6) Antineutrophil cytoplasmic antibodies (ANCA) is associated with some of the necrotizing vasculitides, the c-ANCA is highly specific and sensitive to Wegener's granulomatosis, and the p-ANCA is less specific, but has been associated with microscopic polyangiitis, pauci-immune glomerulonephritis, and Churg-Strauss vasculitis.(7) Therefore, constitutional symptoms, positivity for ANCA test, and elevated ESR should alert clinicians to the possible diagnosis of vasculitis rather than a tumor. Poltarteritis nodosa is probably associated with immune complex deposition in the vessel wall in response to infective agents, and has been associated with the state of hepatitis B and C virus carrier and infection with parvovirus B19 rather than with ANCA.(8-11)
The prognosis for systemic and localized polyarteritis are different. Systemic polyarteritis can be fatal, but localized polyarteritis shows an excellent prognosis.(3) Systemic polyarteritis affects the kidney, heart, skeletal muscle, skin, mesentery, spleen, pancreas, lung, liver, nerves, meninges, brain and spinal cord.(1) Localized polyarteritis has been found in the skin, gall bladder and cervix.(12-14)
Histologically, polyarteritis can be divided into acute and advanced stages. In the acute stage, there is fibrinoid deposition in the vessel wall and dense inflammatory infiltrates composed predominantly of neutrophils, eosinophils, and lymphocytes.(15) In the advanced stage, the thickening of the blood vessel wall with microcalcification is seen.(16) Associated findings of the breast are interlobular fibrosis, focal panniculitis, and an inflammatory infiltrate in lobules of breast acini.(15) Mammary duct ectasia is a benign condition of the mammary gland. Although it is accompanied by inflammatory changes in the collecting ducts, it is not clear that polyarteritis nodosa and mammary duct ectasia are associated.(17) There are no previously reported cases of polyarteritis nodosa with mammary duct ectasia.
Other types of vasculitis that may involve the breast parenchyma are giant cell arteritis and Wegener's granulomatosis. In general, giant cell (temporal or cranial) arteritis involves large vessels with giant cells, thrombosis, and phagocytized fragments of the internal elastic lamina.(18) Wegener's granulomatosis involves veins as well as arteries and exhibits extravascular destructive granulomatous foci.(19) An absence of capillary or vein involvment with giant cells and arteriosclerotic changes differentiates other forms of vasculitis from polyarteritis.(16) Polyarteritis affecting breast tissue should not be confused with superficial thrombophlebitis of the chest wall (Mondor's disease), Behcet's disease, and lupus erythematosus.(20)
In the present case of localized polyarteritis nodosa of the breast with mammary duct ectasia, a good prognosis was achieved by surgical excision. Even though constitutional symptoms may be present, a lack of systemic involvement or life-threatening complications indicates that localized polyarteritis is probably benign unlike the systemic form.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download