Abstract
Purpose
Isosulfan blue has been traditionally used as a tracer to map the lymphatic system during identification of
the sentinel lymph node (SLN). However, this vital dye is difficult to obtain in Korea. Radioisotopes such as technetium-labeled sulfur colloid or albumin colloid are also expensive and complex to use. The purpose of this study is to evaluate usefulness of a sentinel lymph node biopsy (SLNB) using methylene blue dye in breast cancer patients.
Methods
We evaluated the sentinel node mapping experience using methylene blue dye from July 2003 to January 2007. Fifty-eight patients with clinical T1-T2 breast cancer without palpable axillary lymph nodes were enrolled. All SLNs were submitted for intraoperative frozen section and hematoxyline and eosin (H & E) stain analysis. For the negative SLNs, serial sections of each SLN specimen were examined by permanent H & E staining and by immunohistochemical techniques (IHC) using cytokeratin. Regardless of the results of a frozen section for the SLNs, a backup level II or III axillary lymph node dissections (ALND) was performed.
Results
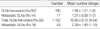
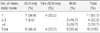
Of the 58 patients that underwent a SLNB using methylene blue dye, an SLN was identified in 56 patients (96.6%), and metastatic SLNs were detected in 14 cases. Axillary lymph node metastasis found in 18 out of 58 patients. Thus, the false negative rate for a SLNB was 22.2% (4/18). Two patients had a micrometastasis (pN1mi) and two patients had clusters of isolated tumor cells (pN0[i+]) that were identified in the SLNs by IHC with the additional use of cytoketatin. The sensitivity, specificity, and accuracy of the SLNBs were 77.8%, 100%, and 92.9%, respectively. The false negative rate improved with the accumulation of experience for performing a SLNB (12.5% vs 30.0%). The sensitivity, specificity, positive predictive value, and accuracy of preoperative ultrasonography (USG) for an axillary lymph node metastsis were 50.0%, 95.5%, 81.8% and 81.0% respectively.
Conclusion
Based on our initial experience, methylene blue dye is safe, inexpensive, and a readily available tracer for the SLN mapping, and it could be an effective alternative to the use of isosulfan blue dye for accurately identifying SLNs in early breast caner patients. We expected that the findings of preoperative USG could serve as useful adjuncts to a SLNB.
Figures and Tables
 | Fig 2Ultrasonographic findings of metastatic axillary lymph node. This lymph node was not palpable. But, this round lymph node had increased vascular flow at perinodal area and cortex on doppler examination and did not display hilar structures. |
 | Fig 3Cytokeratin immunohistochemical staining of sentinel lymph nodes. (A) isolated tumor cells (pN0[i+]) (×400) and (B)1.5 mm sized micrometastasis (pN1mi) (×100). |
Table 3
Sentinel and axillary lymph node status on permanent sections (N=56)
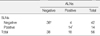
ALNs=axillary lymph nodes; SLNs=sentinel lymph nodes.
*Included 2 cases with clusters of isolated tumor cells (pN0[i+]) in SLN on cytokeratin immunohistochemical stain (IHC); †Include 2 cases with micrometastasis(pN1mi) in SLN on IHC.
Sensitivity=14/18 (77.8%); Specificity=38/38 (100%); Positive predictive value=14/14 (100%); Negative predictive value=38/42 (90.5%); False negative rate=4/18 (22.2%); Accuracy=92.9% (52/56).
References
1. Cunningham DK, Mancino AT, Edwards MJ. Singletary SE, Robb GL, Hortobagyi GN, editors. Axillary staging. Advanced Therapy of Breast Disease. 2004. 2nd ed. Hamilton: BC Decker Inc;349–360.
2. Whitworth P, McMasters KM, Tafra L, Edwards MJ. Stage-of-the-art lymph node staging for breast cancer in the year 2000. Am J Surg. 2000. 180:262–267.
3. The Korean Breast Cancer Society. Nationwide korean breast cancer data of 2004 using breast cancer registration program. J Breast Cancer. 2006. 9:151–161.
4. Simmons R, Thevarajah S, Brennan MB, Christos P, Osborne M. Methylene blue dye as an alternative to isosulfan blue dye for sentinel lymph node localization. Ann Surg Oncol. 2003. 10:242–247.

5. Eldrageely K, Vargas MP, Khalkhali I, Venegas R, Burla M, Gonzalez KD, et al. Sentinel lymph node mapping of breast cancer: a case-control study of methylene blue racer compared to isosulfan blue. Am Surg. 2004. 70:872–875.
6. Masannat Y, Shenoy H, Speirs V, Hanby A, Horgan K. Properties and characteristics of the dyes injected to assist axillary sentinel node localization in breast surgery. Eur J Surg Oncol. 2006. 32:381–384.

7. Tuttle TM. Technical advances in sentinel lymph node biopsy for breast cancer. Am Surg. 2004. 70:407–413.
8. Yang WT, Chang J, Metreweli C. Patients with breast cancer: Differences in color Doppler flow and gray-scale US features of benign and malignancy axillary lymph nodes. Radiology. 2000. 215:568–573.

9. Lee CS, Bong JG, Park JH, Lee YS, Paik SM, Shin MJ, et al. The accuracy of the physical examination, mammography, and ultrasonography in the assessment of tumor size and axillary lymph node metastasis in breast cancer patient. J Korean Breast Cancer Soc. 2003. 6:87–94.

10. Giuliano AE, Male PS, Turner RR, Morton DL, Evans SW, Krasne DL. Improved axillary staging of breast cancer with sentinel lymphadenectomy. Ann Surg. 1995. 222:394–401.

11. Wong JH, Cagle LA, Morton DL. Lymphatic drainage of skin to a sentinel lymph node in a feline model. Ann Surg. 1991. 214:637–641.

12. Tsopelas C, Sutton R. Why certain dyes are useful for localizing the sentinel lymph node. J Nucl Med. 2002. 43:1377–1382.
13. Giulliano AE, Kirgan DM, Guenther JM, Morton DL. Lymphatic mapping and sentinel lymphadenectomy for breast cancer. Ann Surg. 1994. 220:391–401.

14. O'Hea BJ, Hill AD, El-Shirbiny AM, Yeh SD, Rosen PP, Coit DG, et al. Sentinel lymph biopsy in breast cancer: initial experience of Memorial Sloan-Kettering Cancer Center. J Am Coll Surg. 1998. 186:423–427.
15. Derossis AM, Fey J, Yeung H, Yeh SD, Heerdt AS, Petrek J, et al. A trend analysis on the relative value of blue dye and isotope localization in 2,000 consecutive cases of sentinel node biopsy for breast cancer. J Am Coll Surg. 2001. 193:473–478.

16. Hill AD, Mann GB, Borgen PI, Cody HS. Sentinel lymph node mapping in breast cancer. J Am Cancer Soc. 1999. 188:545–549.
17. Simmons RM, Smith SM, Osborne MP. Methylene blue dye as an alternative to isosulfan blue dye for sentinel lymph node localization. Breast J. 2001. 7:181–183.

18. Cimmino VM, Brown AC, Szocik JF, Pass HA, Moline S, De SK, et al. Allegic reactions to isosulfan blue during sentinel node biopsy-a common event. Surgery. 2001. 130:439–442.

19. Thevarajah S, Huston TL, Simmons RM. A comparison of the adverse reactions associated with isosulfan blue versus methylene blue dye in sentinel lymph node biopsy for breast cancer. Am J Surg. 2005. 189:236–239.

20. Montgomery LL, Thorne AC, Van Zee KJ, Fey J, Heerdt AS, Gemignani M, et al. Isosulfan blue dye reactions during sentinel lymph node mapping for breast cancer. Anesth Analg. 2002. 95:385–388.

21. Stradling B, Aranha G, Gabram S. Adverse skin lesion after methylene blue injections for sentinel lymph node localization. Am J Surg. 2002. 184:350–352.

22. BIT Druginfo. accessed Jul 5, 2007. http://www.druginfo.co.kr.
23. Tafra L, McMasters KM, Whitworth P, Edwards MJ. Credentialing issues with sentinel lymph node staging for breast cancer. Am J Surg. 2000. 180:268–273.





 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download