Abstract
Objective
To identify the technical considerations in implementing a barcode-based medication system and propose practical solutions for successful implementation of the system. In order to reduce medical errors related to medication and blood transfusion, we analyze various factors that hinder the successful implementation of the barcode-based medication system and discuss issues involved in the effective adoption of such a system.
Methods
The barcode-based medication system of this research uses one-dimensional, barcode bands on patients' wrists and two-dimensional barcodes attached to drug bags and blood bags. PDAs with barcode reading capability and wireless networking function are used, which enables Point of Care. The business process for applying the developed system and the current status of the system usage are analyzed.
Results
The factors causing a variety of system failures in the demonstration and pilot periods were identified and categorized as including PDA malfunction, PDA battery discharge due to users' carelessness, confusion in reading barcodes and so on.
Conclusions
It is expected that the analyzed obstructive factors and the proposed technical considerations addressed in this paper can help other hospitals implement similar barcode-based medication systems successfully. Ultimately, this research will contribute to reducing medical errors and improving quality of patient care.
As is well-known, human is prone to err1). It is a common phenomenon that medication errors take place in hospitals2). However, the results of the medication errors occurring everyday in the world are so harmful and fatal to patients that sometimes they may lead the patients to death3). Although the researches on medication errors have been performed by pharmacists for about 40 years and it has been reported that the effects of medication errors are much more serious than we realize, it do not draw sufficient attention4).
In 1984, Harvard Medical Practice Study (MPS) addressed that 3.7 of every 100 inpatients were suffered from iatrogenic mishaps. These injuries were most commonly related to medication use (19.4%). Although these results were reported in early 1990s and additional researches were performed in Colorado and Utah, the importance of medication errors did not draw much attention until Institute of Medicine (IOM) published that iatrogenic events resulted in 44,000-98,000 deaths and 13 millions injuries every year in United States5). It is estimated that the costs of treating healthcare errors would be about 3 billion per year in United States. However, hospitals were not actively adopting Information Technology (IT) for patient safety. Therefore, the leading groups like Joint Commission on Accreditation of Hospital Organization (JCAHO) or Hospital Information Management System Society (HIMSS) began to emphasize the importance of patient safety and assign high priority on medical errors in their recent conferences on the issue6).
A medication error indicates any medicine-related mistake made by healthcare professionals. It is recommended that they have to keep five rights principles (right patient, right drug, right dose, right route, and right time) in order to reduce medication errors7)8).
In a survey on nurses' recognition and experience of medication errors in Korea, it was also revealed that most medical errors were related to medication administration. The other errors include giving wrong drugs to patients, over-dosage and wrong medication route to the prescription, and administrating drugs over the term of validity9). In the survey, nurses proposed methods for reducing medication errors such as adopting efficient and effective communication tools (99.0%), providing standardized guidelines (98.3%), rapidly presenting drug information (98.3%), storing similar drugs apart (98.1%), and enforcing five right principles (97.8%)10).
According to JCAHO, the most remarkable method for patient safety is to exactly identify patients to administrate medications. Therefore, it is no wonder that adopting IT like barcode or RFID to identify patients, drug bags, and blood bags for transfusion is prevalent in healthcare sector. Castle et al. also suggested such auto-ID technologies should be applied to nursing activities because IT can help prevent misusing drugs1). Actually, Concord Hospital in New Hampshire revealed that a barcode-based medication system reduced administration error up to 80%5).
Dzik suggested that advanced technologies should be used to improve patient safety and healthcare professionals such as physician and nurses who utilize the systems for reducing errors should devote themselves to reducing errors6).
There have been 3 types of previous studies related to medication errors including transfusion. They are illustrated in Figure 1. The first type is a research on methods for reducing errors occurring during the dispensing process at the pharmacy, which was performed by Poon et al.15). The second type is a research on methods for reducing medication errors by checking identification of patients and drug bags at the bed-side, which was performed by Sun, Wang, and Wu8). The third type performed by Dzik is a research on methods for reducing errors in transfusion processes.
Poon et al. studied the effect of adopting a barcode-based medication system at the pharmacy of a tertiary university hospital having 735 beds, which is issuing about 6 million prescriptions every year. They analyzed the results after adopting the system and compared them with the previous outputs before adopting it. They tried to improve the accuracy of medication during the dispensing process by setting up a new barcode-based dispensing system in 2003. Consequently, the system enabled the hospital to reduce medication errors. For example, the error rate was 0.37% before implementing the system, which improved up to 0.06% after using the system. This indicates 85% reduction of errors. Therefore, Poon et al. suggested that barcode-based medication systems would be very prominent tools for improving medical errors at the hospital pharmacy2).
Fan Wu recommended that nurses should observe 'five rights' principles in administrating medication for patient safety. He suggested that in order to facilitate the observation of these principles a POC environment should be established. IT like barcode or RFID enables the establishment of the POC environment. When nurses administrate medications to patients, in order to check right patients and right drugs they scan drug package and patients' wrist band using PDAs equipped with the capability of reading barcodes and RFID. And then, after nurses check the formulation, dose and time of drugs, and patients' records with their eyes, they provide drugs to the patients. Fan Wu performed a survey on users' satisfaction in order to assess the usefulness of the system. The survey results showed that degree of users' satisfaction was high and the evaluation values about quality and information were very satisfactory8).
Dzik addressed that barcode technology is adopted by lots of hospitals to reduce errors of transfusion and improve patient safety, because adoption costs of barcode-based systems are much lower than RFID systems6). After the University Hospital of Iowa installed a barcode-based medication system connected with Hospital Information System (HIS) using wireless LAN, the system could capture errors up to 10 times more than previously used manual processes. The research pointed out that despite the apparent advantages of barcode or RFID technologies designed to enhance patient safety, the low rate of application of those technologies can be ascribed to the following reasons. First of all, nurses and physicians may feel uncomfortable using those machines or technologies. Furthermore, medical information managers cannot be convinced of the satisfaction level of technological quality and easiness of application of such technologies.
Recently, as the importance of medication errors are recognized significantly, researches on barcode-based or RFID-based systems have been performed. However, those researches are focusing on the clinical results of adopting those systems for reducing medication errors. Few published studies have analyzed technical obstacles of introducing IT and proposed practical solutions for successful implementation of such a system in healthcare area. The objective of this research is to identify technical barriers in implementing a barcode-based medication system and propose practical solutions to overcome those barriers. Various factors hindering the successful application of the barcode-based medication are identified and a successful business model is discussed.
To improve patient safety, a barcode-based medication system using handheld devices equipped with wireless LAN and barcode reader capability have been implemented at a large-sized tertiary general hospital located at Seoul, Korea. The application program was developed and deployed from late 2008. We identified, assessed and analyzed all failures, and settled major technical failures which occurred during the demonstration period from mid February to March 2009 (demonstration period: about 1.5 month). After that period, the system was deployed to the 14 wards and pilot-tested. We gathered and analyzed all failure cases which took place from April to July 2009 (pilot period: 4 months).
The barcode-based medication system can be divided into two sections: the ward side or bed-side where patients are located and the server room where server machines are placed (Refer to Fig. 2). In the wards, patients are wearing a wristband containing their identification information, and drug bags and blood bags are labeled with barcodes. When nurses scan barcode information using a PDA, it sends the information acquired from the barcode to the server located at the server room through a wireless Access Point (AP). Then the server checks the legacy database containing the information prescribed by a physician, and returns the results to the PDA.
The hospital had to decide which identification technology would be adopted before implementing the system. Although RFID provides several benefits such that it can store large information and it is easy to read and write data, it has critical problems in order to be adopted in healthcare environments. First of all, although there have been continuous improvement, its recognition rate are still under 95%. In addition, it costs much more than barcode-based systems11-13). Especially, the recognition rate of target objects containing metals or liquid components degrades drastically. Therefore, the hospital adopted the barcode technology as an identification method for the medication system for patient safety.
Patients' wrist bands are used for identifying patients, and simple one-dimensional barcodes are attached to the bands. Two-dimensional barcodes are attached to drug packages and blood bags because they can contain large size data prescribed by a physician.
When a patient is admitted to a ward, he or she receives a wristband with a one-dimensional barcode from the department of patient affair. Figure 3 illustrates a sample barcode of a patient's wristband. Although one-dimensional barcode can store up to 20 bytes14), the hospital uses only 10 bytes. The first byte indicates the start, and the next 8 bytes are used for the identification number of the patient. And the last byte indicates the end.
Barcodes are attached to anti-cancer drug bags at the pharmacy when they are dispensed by a pharmacist. Blood bags for transfusion are also labeled with a barcode by a phlebotomist at the blood bank. Although a two-dimensional barcode can store up to 2,000 bytes14), the hospital uses only 32 bytes. Figure 4 shows a sample of a drug bag label containing a two-dimensional barcode.
BIP-5300 PDAs of Bluebird Soft Inc., a PDA manufacturer, have been used by the hospital. The PDA has barcode reading capability to scan barcodes of wristbands, drug bags, and blood bags. Also, it has a wireless network driver to be connected with HIS network and transfer data to the server. Then the screen of the PDA can provide the results checked and received from the server.
The basic and core infrastructure of the barcode-based medication system is the wireless local area network. Most PDAs provide wireless networking functions. Due to the costs of wireless infrastructure, it is not so common to provide wireless network to the wards of hospitals. Fortunately, the target hospital in this research is completely equipped with wireless network infrastructure at wards in order to serve POC and Electronic Medical Record (EMR). Thus it does not induce additional costs for wireless networking. Through the wireless APs, a PDA can be connected with HIS and communicate with the server. About 800 wireless APs (Aruba AP-70) of Aruba Networks Inc. are used for the wireless network infrastructure.
There are various hardware machines at the server room in the hospital. Among them only 3 resources are related to the system. The first one is the main server which helps physicians prescribe orders. The second server is the legacy database server which stores the prescription information. The last one is the server for the barcode system which receives data from the PDA through wireless APs, checks the legacy database, and returns the results to the PDA.
The business flow of the barcode-based medication system is illustrated in Figure 5. As mentioned before, barcodes are attached to anti-cancer drug bags and blood bags, because the medication errors related to those bags can be fatal to the life of a patient. In case of anti-cancer drugs, physicians prescribe them for patients, and then the information is transferred to the pharmacy, and finally drugs are dispensed, packaged and labeled by pharmacists. After that, drugs dispensed by pharmacists are transported to the wards. In case of transfusion, the recipient information of a blood bag in the refrigerator is checked and then labeled with a barcode by phlebotomists. It is also transported to the wards.
Figure 6 illustrates screen shots of each medication step using the system. Before nurses administrate drugs and blood bag to patients, at first they log into the mobile HIS using the PDA. And then nurses check the identification of the patient, wristband, drug bag, and blood bag. Using the PDA, they scan barcodes on drug bags and blood bags. The scanned information is transferred to the server through the wireless AP. The server fetches the patient's ID from the legacy database and returns it to the PDA. Then the PDA display whether returned patient's ID is the same with the ID information acquired from the wristband. If both of the information are the same, nurses administrate drugs to the patient. In case of transfusion, before nurses provide blood to the patient, they have to scan nurses' ID in order to store information about who give blood to the patient. All data generated during the whole process are stored at the server.
The hospital issues about 1.5 million prescriptions for inpatients administration every month. The number of prescriptions relating to anti-cancer drugs and transfusion, to which the barcode-based medication system is applied, is about 30,000. It accounts for about 2% of whole prescriptions in the hospital. The system was deployed to 14 wards during the pilot period. The rate of applying the developed medication system to anti-cancer drugs and transfusion in prescribing orders at those wards were about 85% and 10% respectively.
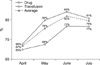
Figure 7 illustrates the system usage rate during the pilot period. From April to July 2009, the rate of barcode reading using the system before providing anti-cancer drugs to patients has been increased from 68% to 81%. In case of transfusion, it has been increased from 65% to 77%.
A help desk which holds specialized staffs in receiving and recording failure cases has been established in order to receive all the failures from users. All the failure cases collected by the help desk have been analyzed and major causes inducing such failures have been identified and categorized into several major types. Table 1 summarizes the number and the rate of each failure type during the demonstration period and the pilot period respectively.
In the demonstration period, the functions of the barcode-based medication system were tested from mid February 2009 to March 2009 after the server, network infrastructure, and application programs were deployed to the wards. Failures during this period were classified into three major categories. The most common failure type among them was 'malfunction of PDA' (47%). The next one was 'discharge of PDA battery' (24%) and another major failure type was 'confusion in reading barcodes' (15%). There have been other errors such as application errors, errors on barcode itself and so on (14%).
Failures of barcode reader, battery malfunctioning, and malfunctioning of application on the PDA belong to malfunction of PDA. The most commonly reported failures were related to the wireless network driver which enables a PDA to be connected with HIS through a wireless AP. The hospital has used BIP-5800 PDAs of Bluebird Soft Inc., which has no problem in being connected with only one wireless AP. However, if several APs are located in the vicinity of the PDA, connection failure happened because of the connection competition among multiple wireless APs.
The next major problem was discharge of PDA battery due to the carelessness of the users. It was common that after nurses used PDAs, they leaved them behind without care. Thus the battery was discharged completely and then all application programs on the PDA were removed automatically. The habit of putting the PDA into a battery charger would prevent this type of failures.
Confusion in reading barcodes occurs because there are multiple barcodes on the target bags. Especially, in case of transfusion, barcodes are placed during blood-collecting activities, transporting from one agency to another agency, and verification time in hospital. Nurses in administration should know the exact position of the target barcode for successful scanning.
Except for the three major failure types, other failures happened, which are caused because the application program of the new system could not provide fully satisfactory interoperability with the legacy database, and barcodes were printed poorly or barcodes were blurred after printing.
Among the major failure types identified during the demonstration period, malfunction of PDA was fixed at first. Specifically, the problem of wireless network driver of PDA (BIP-5300 of Bluebird Soft Inc.) was resolved. During the demonstration period, due to the network driver of the PDA, the connection between AP and PDA had experienced problems as mentioned earlier. After the network driver was redeveloped and uploaded to the PDA in order to provide stable connection between the PDA and APs, this type of failures has disappeared.
The number of failures which occurred during the pilot period was 115. In average, about 30 cases occurred every month. Confusion in reading barcodes was the most common failure type, which accounts for 53% failure cases. The next one was discharge of PDA battery (19%). Another 29% belonged to other failure types such as PDA's power problem, malfunction of the barcode reader on PDA, problem of barcode itself, application program errors, and so on.
Basically, confusion in reading barcodes is an industry-wide issue. Therefore, a hospital cannot solve the problem for itself. During the pilot period, as other types of failures have been resolved and the number of prescriptions increased, the number and rate of confusion in reading barcodes increased. Anti-cancer drugs and blood are liquid, and packaged into bags that have an oval-disc shape. And this makes it difficult to scan the barcodes correctly from the bags. When the blood bags kept in the refrigerator are taken out and treated at normal room temperature before transfusion, sometimes moisture in the air can blur barcodes on the surface of the bags. In this case, it is not easy to read the barcode properly.
The basic cause of discharge of PDA battery is the same with the during the demonstration period. Nurses are likely to leave PDAs aside, thus the battery can be discharged completely, which induces severe problems. If they would pay a little more attention to this matter, they could prevent such problems.
Although the number of malfunction of PDA decreased considerably, the problem of inexperienced user appeared newly during the pilot period. Sometimes, inexperienced users could not deal with the system appropriately. The rates of other errors such as badness of barcodes, and application errors were similar to those of the demonstration period. Essentially, these are problems to be solved gradually after the system begins to operate in hospital. It is not possible to sweep away such problems at a time because they would appear continuously.
As we found in the previous researches, the efforts for reducing medication errors and improving patient safety by adopting IT such as barcodes and RFID will lead to positive results. However, in order to implement a more successful and effective business model in clinical settings, the following issues including technical stability and standardization, establishment of barcode standards, and mitigation of user's resistance to emerging technologies should be considered and resolved.
In healthcare sector, HIS and mobile solutions supported by wireless network are becoming prevalent. Wireless network is a core infrastructure to enable POC, as described earlier in Section II. However, it is required to provide some improvements to make the barcode-based medication system stable. The urgent one is about the standardization of the communication protocol between APs and mobile devices such as PDA, especially for the case that several APs are competing to make a connection with a PDA. Initially, we had a huge trial and error in organizing PDA into the barcode-based medication system which have used wireless network for POC. We wasted a half of project time to resolve this kind of problem. If manufacturers or vendors of various wireless APs and PDAs would set a standard protocol between them, mobile solutions like the barcode-based medication system could be implemented in the hospital without difficulty. Otherwise, the same problems will happen at other sites where similar systems are to be implemented, which may induce a nation-wide waste of costs and negatively influence the effort for improving patient safety.
As mentioned in the previous section, a major failure type of the barcode-based medication system has been confusion in reading barcodes. It is expected that this type of failures will last continuously in the future until standardization of barcodes is accomplished. As happened in our system, several barcodes on the blood bags for transfusion might generate confusion in reading barcode information at the bedside. Recently, Korean government is endeavoring to adopt standardized barcodes for drugs named Korea Drug Code (KDC). Standardized barcodes will be a substantial assistance to improve patient safety and reduce medical errors.
During the pilot period, discharge of PDA was one of the common types of failures. Confusion in reading barcodes and standardization of barcodes are problems resulted from the industry-wide issues in healthcare sector. Actually, it seems that users are reluctant to utilize the barcode-based medication system because they are not sure the system is effective in administration of drugs to patients. According to a recent paper, although the proportion of time nurses spent on medication administration activities remained unchanged, the proportion of time spent in providing direct patient care increased because of streamlining the administration process15). Therefore, it is very important to make users be assured of the system and adopt it actively.
It is very hard to exactly estimate return on investment (ROI) of the barcode-base medication system. However, we believe the system is definitely providing an essential benefit concerning reducing medication errors and improving patient safety. If the issues discussed in this section such as standardization of wireless network protocols, standardized barcodes, and enhancing user acceptance of emerging technology would be resolved, it will be possible to effectively implement similar medication systems to reduce errors and improve safety or save human lives.
Recently, lots of studies on reducing medical errors by adopting emerging auto-ID technologies such as barcode and RFID are reported. However, there has been little research that implements such a technology and practically analyzes technical barriers in hospitals in Korea. We hope that in order to verify the clinical effects of the system, more studies on improving patient safety in both clinical and technical aspects would be performed in the future.
Figures and Tables
References
1. Huang HH, Ku CY. A RFID grouping proof protocol for medication safety of inpatient. J Med Syst. 2008. DOI 10.1007/s10916-008-9207-z.

2. Poon EG, Cina JL, Churchill W, Patel N, Featherstone E, Rothschild JM, et al. Medication dispensing errors and potential adverse drug events before and after implementing bar code technology in the pharmacy. Ann Intern Med. 2006. 145(6):426–434.

4. Flynn EA. A brief History of medication errors. Accessed August 29 2009. Available at: http://www.medaccuracy.com/Papers%20and%20Publications/A%20Brief%20History%20of%20Medication%20Errors.pdf.
5. Kaushal R, Bates DW. Information technology and medication safety: what is the benefit? Qual Saf Health Care. 2002. 11:261–265.

7. Bernard F, Brian M, Aziz S. Reducing medication-related adverse events in elderly patients. Rev Clin Gerontol. 2006. 16:79–87.

8. Sun PR, Wang BH, Wu F. A new method to guard inpatient medication safety by the implementation of RFID. J Med Syst. 2008. 32(4):327–332.

9. Lee SY. A study on medication error among nurses and prevention strategy [dissertation]. 2008. Daejeon: Eulji University;35.
10. Cho WS. A study on the types and causes of medication errors and related drugs. J Korea Community Health Nurs Acad Soc. 2002. 16(1):176–189.
11. A study on the introduction methodology of RFID. National Computerization Agency. Accessed August 29, 2009. Available at: http://www.nia.or.kr/open_content/board/fileDownload.jsp?tn=LC_0000047&id=51912&seq=1&fl=7http://www.nia.or.kr/open_content/board/fileDownload.jsp?tn=LC_0000047&id=51912&seq=1&fl=7.
12. Choi KA, Jung IS, Yu HS, Yoon ES, Lee YH, Kang UG. A study on RFID recognition rate for pharmaceutical storage management. J Korea Soc Comput Inform. 2008. 16(2):249–254.
13. Ji KY, Kim D, Kim MC, Lee YH, Kim SB, Lee SK, et al. Ubiquitous health. 2006. 1st ed. Seoul, Korea: Jinhan M&B;196.
14. Park SD. Mobile authentication system and it's application based on 2-dimensional barcode and OTP [dissertation]. 2009. Seoul: Hanyang University;3.




 PDF
PDF ePub
ePub Citation
Citation Print
Print









 XML Download
XML Download