This article has been
cited by other articles in ScienceCentral.
Abstract
Protothecosis is an uncommon human infection caused by achlorophyllic algae of the genus Prototheca, especially P. wickerhamii. The skin is the most frequently involved organ and cases of protothecal tenosynovitis are very rare. A 71-year-old woman without prior medical history except hypertension presented with painful swelling of her right hand that did not improve despite receiving antibiotic treatment. She underwent tenosynovectomy and drainage. Histopathologic examination revealed necrotizing granulomatous inflammation and numerous spherical or morula-like organisms with a spoked wheel appearance. P. wickerhamii was identified from tissue culture. The lesion did not improve with empirical fluconazole therapy. Conventional amphotericin B was administered according to antifungal susceptibility tests and the lesion completely resolved. Protothecosis should be considered in the differential diagnosis for chronic tenosynovitis that does not respond to conventional antibacterial treatment; tissue biopsy with culture is required for diagnosis.
Keywords: Protothecosis, Prototheca wickerhamii, Tenosynovitis, Immunocompetent, Antifungal susceptibility
Introduction
Protothecosis is a rare opportunistic infection in humans caused by the genus
Prototheca, which are achlorophyllic algae that are ubiquitous in nature [
1,
2]. Among this genus, only
P. wickerhamii and
P. zopfii have been associated with disease in humans, with
P. wickerhamii infection being more common. The skin is the most frequently involved organ. Cutaneous infections commonly develop in immunocompetent patients, whereas disseminated infections mainly affect immunocompromised patients [
1,
3,
4]. However, cases of protothecal tenosynovitis are very rare [
5]. Furthermore, no standard therapeutic regimen for protothecosis has been established. Here we describe a case of tenosynovitis caused by
P. wickerhamii in an immunocompetent patient that was successfully treated with amphotericin B according to the results of antifungal susceptibility tests.
Case Report
A 71-year-old woman presented with a 1-month's history of painful swelling of her right hand. She was diagnosed with hypertension 20 years previously, and had undergone partial thyroidectomy. She underwent a left total knee replacement 10 years previously. The patient was otherwise healthy. Her right hand was injured by a cow horn 7 months previously. This resulted in swelling of her hand, without an open sore, that resolved spontaneously. One month previously, her right hand again became swollen and painful. The swelling did not improve despite receiving antibiotic treatment at a local clinic. Ultrasonographic findings suggested tenosynovitis. She underwent tenosynovectomy and drainage twice under local anesthesia. Tissue biopsy suggested fungal infection, but the blood and tissue cultures remained negative. She was referred to our department for evaluation of a fungal infection of the hand.
At presentation, her body temperature and blood pressure were 37.2°C and 120/80 mmHg, respectively. Physical examination revealed an unhealed 10-cm wound incision with purulent discharge on the dorsum of her right hand. Routine laboratory blood analysis revealed a normal white blood cell count (7,000/mm3; normal 4,800-10,800/mm3), erythrocyte sedimentation rate (11 mm/hour; normal 0-20 mm/hour), and C-reactive protein level (0.16 mg/dL; normal value 0-0.3 mg/dL).
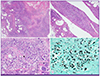
Histopathological examination of the biopsy specimen obtained at the local clinic revealed necrotizing granulomatous inflammation composed of geographic necrosis and dense lymphohistiocytic infiltrates, and reactive synovial hyperplasia (
Fig. 1A and B). Additionally, numerous spherical or morula-like organisms with a "spoked wheel" appearance were identified at a high magnification (
Fig. 1C). The organisms impregnated well with methenamine silver stain (
Fig. 1D).
P. wickerhamii was identified from pus culture by using the VITEK2 system (bioMérieux, Marcy l'Etoile, France) with 98% probability and matrix-assisted laser desorption ionization-time of flight mass spectrometry (MALDI-TOF MS)-based VITEK MS system (bioMérieux, Marcy l'Etoile, France) with confidence value of 99.9%. Bone scan showed no evidence of osteomyelitis in the affected area. She was administered fluconazole (400 mg/day) intravenously for 2 weeks. However, the wound did not improve. In vitro antifungal susceptibility testing was performed by using broth microdilution method according to Clinical and Laboratory Standards Institute (CLSI) standards [
6]. Minimal inhibitory concentrations (MIC) were 64 μg/mL for fluconazole, 1 μg/mL for voriconazole, 0.25 μg/mL for amphotericin B, and >4 μg/mL for both caspofungin and micafungin. After the antifungal therapy was changed to conventional amphotericin B (1 mg/kg/day), the wound healed gradually. Conventional amphotericin B was administered for 3 weeks and the patient showed no evidence of recurrence.
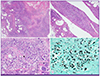 | Figure 1(A) The lesion showed necrotizing granulomatous inflammation composed of geographic necrosis and abundant inflammatory infiltration (hematoxylin and eosin stain, original magnification ×40). (B) Some portions of the synovial surfaces revealed reactive papillary hyperplasia (hematoxylin and eosin stain, original magnification ×100). (C) Numerous spherical organisms of variable sizes were identified at a high magnification (hematoxylin and eosin stain, original magnification ×400). An example of a sporangiospore with a “spoked wheel” appearance is indicated by an arrow head and its magnified image is in the inset box (hematoxylin and eosin stain, original magnification ×1000). (D) The organisms were identified using methenamine silver staining (original magnification ×400). 
|
Discussion
Prototheca species seem to have low virulence and are considered rare opportunistic pathogens [
2]. These algae can be isolated from various reservoirs, such as the environment, animals, and food. Infection may occur by penetration of the organism when the injured skin comes in contact with contaminated water [
1]. Protothecal infections mainly develop in patients with underlying immunosuppression or severe underlying disease such as local or systemic steroid use, hematologic malignancy, diabetes mellitus, acquired immunodeficiency syndrome, organ transplantation, alcoholism, and peritoneal dialysis [
7]. Protothecosis has also been reported in association with surgery and orthopedic procedures in a hospital setting. The majority of protothecosis cases are simple cutaneous infections in immunocompromised individuals. Additionally, olecranon bursitis in individuals who have penetrating or non-penetrating trauma to the affected elbow, and disseminated infection among those who are severely immunocompromised have been reported. However, cases of tenosynovitis are very rare [
5]. In this patient with a history of minor trauma, the protothecal tenosynovitis occurred without the underlying condition of immunosuppression.
In general, protothecosis is not suspected clinically in patients with a tenosynovitis, and the patients are subjected to various treatment modalities for long periods of time without satisfactory results [
2]. If the lesion is resistant to usual treatment especially in an immunocompetent patient, clinicians should consider tissue biopsy and culture. When a fungal infection is suspected and a biopsy and/or culture yield positive results for fungal infection, the correct diagnosis can be reached.
Surgical intervention coupled with administration of antifungal agents has been considered as the standard treatment for protothecal infections [
3]. Various treatment regimens including antifungal and antibacterial agents have been attempted. However, there are no official guidelines for performance or interpretation of in vitro susceptibility tests for these algae [
8].
Prototheca species show various susceptibility profiles and there is no direct correlation between in vitro activity and clinical response [
6]. Treatment failure is not common. Thus, in vitro antifungal susceptibility testing is not routinely recommended for patient management. Antifungals such as the azoles (ketoconazole, itraconazole, fluconazole) and polyenes (conventional amphotericin B, liposomal amphotericin B) appear to be the most effective medical treatment to date [
4,
7]. Nevertheless, in vitro antifungal susceptibility testing was performed because intravenous administration of fluconazole was not successful in this patient.
P. wickerhamii isolated from this patient was resistant to azoles and echinocandins, whereas it was susceptible to amphotericin B. After 3 weeks of conventional amphotericin B administration, the lesion was markedly improved. Therefore, in vitro susceptibility testing should be considered if clinical treatment is not successful.
Protothecosis should be included in the differential diagnosis for chronic tenosynovitis that does not respond to conventional antibacterial treatment and tissue biopsy with culture is required for establishing the diagnosis. Furthermore, antifungal susceptibility testing should be considered in patients who show clinical failure.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download