Abstract
There are little data on the changes in lymph node (LN) size during the treatment of tuberculous lymphadenopathy (TB LAP). This study aimed to provide data on LN changes during treatment. Between March 2014 and December 2015, 20 patients who were diagnosed with cervical TB LAP were enrolled. LN enlargement within two months (50%, 4/8 vs. 8.3%, 1/12; P = 0.04) was more frequently observed in patients with initial LN size ≥ 7.5 cm2. Enlarged LNs were excised in three patients owing to pain and fistula formation. Initial LN size may be associated with LN enlargement during treatment.
Lymph nodes (LNs) are commonly affected sites in extrapulmonary tuberculosis. The treatment of tuberculous (TB) lymphadenopathy (LAP) is not usually different from that of pulmonary TB, typically consisting of a six-month anti-tuberculosis regimen [12]. The decrease in LN size is usually used as an indicator of treatment response in TB LAP, while negative conversion of sputum culture is used to determine treatment response in pulmonary TB. However, Using LN size as an indicator of treatment response can be problematic because LN nodes frequently persist despite the six-month treatment regimen and often paradoxically enlarge during treatment [34]. In order to use LN size as an indicator of treatment response, kinetic data on LN size during treatment is needed. However, little is known on how and when LN size changes during treatment. Thus, this study aimed to provide data on the change of LN size during treatment and to identify the difference in this kinetics according to the initial LN size.
Between March 2014 and December 2015, 31 patients diagnosed with cervical TB LAP were enrolled at the Soonchunhyang University Bucheon Hospital, Bucheon, Korea. Patients were considered to have TB LAP if their clinical specimens were positive for Mycobacterium tuberculosis on culture, acid-fast bacilli staining, or in M. tuberculosis polymerase chain reaction (PCR) assays. Microbiological and pathological specimens were processed using standard techniques and procedures [5]. Briefly, mycobacteria were cultured on liquid and solid culture media, and the M. tuberculosis complex was identified using a commercial DNA probe (AccueProbe M. tuberculosis Complex Culture Identification Test; Gen-Probe, San Diego, CA, USA). A commercially available PCR test kit (COBASAMPLICOR MTB; Roche Diagnostics, Branchburg, NJ, USA) was used to assay fresh and fixed samples. Of the patients diagnosed with TB LAP, four who were not followed up for 6 months and seven whose LN size was not estimated were excluded. Finally, 20 patients were included in the study. The local Institutional Review Board approved this study. The size (area, cm2) of the affected LN was determined by multiplying longest length and breadth and was assessed using a ruler once a month for 6 months. Treatment completion was defined as the administration of anti-TB regimens for at least 6 months without interruption. Increased LN size was defined as an increase of more than 1 cm2 during treatment. The large initial LN size group was defined as those patients with an initial LN size greater than 7.5 cm2, which was determined based on receiver operating characteristics curve analysis. The decision for excision was made according to the physicians’ judgment. Incision and curettage as a surgical intervention was not performed in our hospital. The results were analyzed using a commercially available software package (SPSS software, version 14.0 K for Windows; SPSS, Inc., Chicago, IL, USA). Categorical variables were evaluated using Fisher’s exact test. All tests of significance were two-tailed, and P values <0.05 were considered statistically significant.
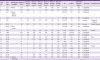
The clinical characteristics of the enrolled patients are shown in Table 1. Thirty percent of the patients were male and the median age was 39 years (range, 16 - 68 years). The median LN size was 4 cm2 (range, 0.25 - 25 cm2). Most of the patients were previously healthy. Four (20%) patients received anti-TB regimens for 7 to 9 months. In eight (40%) patients, the LN was palpable at the time of treatment completion. Anti-tuberculosis-regimen resistance was not observed in the four patients whose susceptibility test results were available. Five (25%) patients received LN excision for the following reasons: three for complaints associated with pain and fistula, one for diagnostic purposes, and one due to a request to remove the remaining LN. Treatment outcomes according to initial LN size are shown in Figure 1. Eight (40%) patients had initial LN sizes of 7.5 cm2 or more. In a half of these patients, LN size increased within two months of starting treatment. Of the four patients with an initial LN size of 7.5 cm2 or more whose LN enlarged during treatment, 75% (3/4) underwent LN excision owing to pain and fistula formation. Of the 12 patients with LN sizes less than 7.5 cm2, only one patient experienced LN enlargement during treatment. LN enlargement during treatment was more frequently observed in patients with an initial LN size ≥ 7.5 cm2, comparing to those with an initial LN size < 7.5 cm2 (50%, 4/8 vs. 8.3%, 1/12; P = 0.04).
Lymph node size was determined by multiplying the longest length and breadth. The size of the affected lymph node was assessed using a ruler once a month for 6 months. Treatment completion was defined as the administration of antituberculosis regimens for at least 6 months without interruption. Tissue biopsy findings of tuberculous lymphadenopathy included granulomatous inflammation with and without caseous necrosis. Resistance to the antituberculosis regimens was not observed in the four patients whose susceptibility test results were available.
This descriptive study showed that many patients with large LN at the time of diagnosis experienced LN enlargement within two months of starting treatment. These are useful kinetic data on LN size during treatment of TB LAP.
Several studies have assessed the association of LN size with outcome in TB LAP. In a retrospective study on paradoxical response of TB LAP, Cho et al. reported larger LN in patients with paradoxical responses compared to those without (3 cm [range 0.5 - 8.0 cm] vs. 2.5 cm [range 0.5 - 7.0 cm]; P = 0.01) [3], although the difference was not statistically significant in the multivariate analysis. The paradoxical response group included not only patients with LN enlargement during treatment but also those with sinus discharge and newly developed LN. In addition, LN size was analyzed as a continuous rather than a categorical variable. These differences may weaken the statistical power of this previous study. In a study performed in Thailand in which clinical cure was defined as the complete disappearance of TB LAP, only 47.4% (9/19) of patients with LN > 3 cm achieved a clinical cure, compared to 86.4% (19/22) clinical cure in those with LN < 3 cm [6]. Another study that measured TB LAP size using computed tomography (CT) showed that LN volume and the ratio of the necrotic area can be used to predict treatment response [7]. In this previous study, LN volume was larger in non-responders than that in responders (107 vs. 35 cm3; P < 0.001). Our findings also support the previous results that initial LN size is associated with outcome in TB LAP.
This study has several limitations in. Firstly, a small number of patients were included and many patients were excluded because the LN size was not evaluated. In addition, multivariate analysis was not possible owing to the small number of patients. Secondly, LN size as a unit of area (cm2) was manually evaluated using a ruler. CT can provide data on size as a unit of volume (cm3) and details such as necrosis [7] but would be practically impossible owing to the cost and radiation exposure. We indirectly estimated expected volume (cm3) by multiplying the estimated area (cm2) and mean length and breadth. This expected volume was correlated with estimated volume in 16 patients who underwent neck CT (coefficient of correlation 0.611; P = 0.02). Therefore, the area itself or expected volume calculated from the area could replace estimated volume. Thirdly, LN enlargement was arbitrary defined. A consensus on how LN enlargement is defined is necessary. Fourthly, there is no consensus on the indications for surgical intervention in TB LAP. This decision has been made according to individual judgment. Surgical intervention can resolve complaints such as pain and may be helpful to shorten treatment duration and reduce relapse rate. However, some studies reported that stable or worsened LN during treatment was naturally regressed in most patients despite extended treatment duration [89]. Surgical intervention frequently results in a large scar that may be a permanent cosmetic problem. Future studies should assess the costs and benefits of surgical intervention based on cosmetic outcome and relapse. Finally, this study did not assess long-term outcomes such as relapse or recurrence.
In conclusion, initial LN size may be associated with LN enlargement during treatment. Further studies should be followed to develop individualized treatment strategies according to initial LN size in TB LAP.
Figures and Tables
Figure 1
Treatment outcomes of tuberculous lymphadenopathy according to initial lymph node size.
Five (25%) patients received LN excision for the following reasons: athree for complaints associated with pain and fistula, bone due to a request for remaining LN excision, and cone for diagnostic purposes. LN enlargement during treatment was more frequently observed in patients with initial LN size ≥ 7.5 cm2, compared to those < 7.5 cm2 (50%, 4/8 vs. 8.3%, 1/12; P = 0.04).
LN, lymph node.

Table 1
Clinical characteristics and outcomes of patients with tuberculous lymphadenopathy and changes in lymph node size during treatment
References
1. Lee JY. Diagnosis and treatment of extrapulmonary tuberculosis. Tuberc Respir Dis (Seoul). 2015; 78:47–55.

2. Korean Society for AIDS. The 2015 clinical guidelines for the treatment and prevention of opportunistic infections in HIV-infected Koreans: guidelines for opportunistic infections. Infect Chemother. 2016; 48:54–60.
3. Cho OH, Park KH, Kim T, Song EH, Jang EY, Lee EJ, Chong YP, Choi SH, Lee SO, Woo JH, Kim YS, Kim SH. Paradoxical responses in non-HIV-infected patients with peripheral lymph node tuberculosis. J Infect. 2009; 59:56–61.

4. Polesky A, Grove W, Bhatia G. Peripheral tuberculous lymphadenitis: epidemiology, diagnosis, treatment, and outcome. Medicine (Baltimore). 2005; 84:350–362.
5. Kim SH, Choi SJ, Kim HB, Kim NJ, Oh MD, Choe KW. Diagnostic usefulness of a T-cell based assay for extrapulmonary tuberculosis. Arch Intern Med. 2007; 167:2255–2259.

6. Kanjanopas K, Siripan N, Phoophitphong R. Tuberculous cervical lymphadenopathy and the role of surgical treatment. Southeast Asian J Trop Med Public Health. 2014; 45:1419–1424.
7. Joo YH, Hwang SH, Seo JH, Kang JM. Treatment assessment based on computerized lymph node volume and ratio of necrotic area in tuberculous cervical lymphadenitis. Auris Nasus Larynx. 2012; 39:402–406.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download