Meningococcal disease presenting with meningitis or sepsis is a life-threatening illness with significant morbidity and mortality worldwide. Despite providing appropriate antibiotic therapy and supportive care, invasive meningococcal disease could lead to death within a few hours to days, with a case fatality rate of 10-15% [1]. The incidence of meningococcal disease varies from 1 to 1,000 cases per 100,000 persons in different regions of the world. Age-specific incidence of meningococcal disease is the highest among children younger than 1 year; the second incidence peak is observed in adolescents and young adults of 15-24 years of age. The burden of meningococcal disease in Korea was reported to be relatively low based on the national notifiable diseases surveillance system, which reported an annual incidence of 0.01 to 0.08 cases per 100,000 persons [2]. However, the burden of meningococcal disease in Korea was expected to be substantially higher than that shown by the documented reports. It was difficult to understand meningococcal disease in the Korean population because of limited epidemiological data.
Kang et al. [3] investigated age-specific seroprevalence of human serum bactericidal antibody (hSBA) titers against Neiserria meningitidis serogroups A, C, W-135, and Y in Korean adolescents and adults aged between 11 and 50 years nationwide. Their study could bridge the gap between surveillance data and actual burden of meningococcal disease.
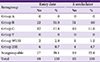
Their study suggests varied levels of natural immunity against the four serogroup meningococci, which reflects exposure to meningococcal capsular antigen. Meningococci are transmitted only from one human to another by infected respiratory secretions or saliva via airborne respiratory droplets usually under crowded living conditions. After exposure, it colonizes the oropharygeal mucosa known as carriage. The immune response elicited by the carried meningococci results in protective antibody responses [4]. In their study, protective antibodies with hSBA titers ≥8 were highly prevalent (74%) in serogroup W, and the lowest prevalence was observed in serogroup A (9%). To understand seroprevalance of N. meningitidis in Korean population, the carriage state needs to be investigated. Although carriage state was not included in that study, recent findings in carriage-related studies were slightly different from that in the seroprevalence study. A carriage- related study among freshmen living in a Korean university dormitory showed that serogroup C was the most prevalent serogroup among groupable isolates [5]. Another study among Korean military recruits showed that serogroup B had the highest proportion of groupable isolates, followed by serogroup C (Table 1) [6]. The proportion of serogroup W-135 in the two carriage-related studies was comparatively low (1.2-6.3%). In contrast to the findings of the carriage-related studies, serogroup W-135 was observed in a small outbreak of meningococcal disease at an army basic training center and in two sporadic cases in Korean soldiers since 2010 [7]. Furthermore, these isolates were all confirmed with a novel sequence type (ST) 8912 by multilocus sequence typing (MLST) analysis. Newly emerged ST N. meningitidis could be associated with case clusters or outbreaks. Meningococcal disease caused by W-135 ST-11 strain that emerged through recombination with hypervirulent lineage, serogoup C ST-11, has become globally a serious problem since the Hajj outbreak in 2000 [8]. W-135 ST-11 strain has spread in Asian countries, even though not identified in Korea. Therefore, for a Korean physician, W-135 meningococcal disease might be an unrecognized or under-reported infectious disease.
Why is it difficult to identify meningococcal disease in Korea? The reasons for under-reported meningococcal disease incidences might be related to antibiotic use and diagnostic methods used in Korea [9]. Because N. meningitidis is sensitive to changes in temperature, it is frequently difficult to culture it. Furthermore, administering antibiotic therapy prior to cerebrospinal fluid (CSF) or blood sample collection considerably increases the likelihood of the results of the samples being negative for N. meningitides culture. Meningococcal disease has been generally confirmed by isolation or antigen detection of N. meningitidis from the CSF or blood samples in Korea so far. Compared to diagnosis by using conventional methods like microbial culture, the use of polymerase chain reaction (PCR) tests might increase the meningococcal disease diagnosis sensitivity by approximately 60%. Previous prospective and population-based surveillances over a 2-year period showed that N. meningitidis affected 13.2% (92 of 608 cases) patients with bacterial meningitis, that is, children <5 years of age in Korea [10]. These results were obtained from culture-negative CSF specimens tested by a meningococcal species-PCR assay. In this study, the estimated incidence rate of meningococcal meningitis in Korean children <5 years of age was 6.8 cases (95% CI; 3.5-13.5) per 100,000 persons, with the highest rate of 27.2 cases (9.9-74.2) among young infants <6 months.
Studies on immunity to meningococcal disease conducted by Goldschneider in the 1960s showed an inverse correlation between age-related incidence of meningococcal disease and seroprevalence [11]. The age-specific seroprevalence of SBA titers observed in Korea is similar to the results of a study conducted in Germany [12]. High seropositivity against serogroup W-135 and low seropositivity against serogroup A were observed in two countries, while intermediate levels of seropositivity against serogroup C and Y were observed. An estimated incidence rate of invasive meningococcal disease in Germany was 1.1 cases per 100,000 inhabitants; the highest rate of 8.8 cases per 100,000 inhabitants was observed for children aged <5 years [13]. These findings are evidences that suggest that meningococcal disease in Korea was an under-recognized and under-reported infectious disease.
While the overall incidence of meningococcal disease in Korea might be relatively low, that is, approximately 1 case per 100,000 persons compared to that observed in the other countries, high mortality rate and intermittent outbreak are likely to continue. Further investigation on carriage state and molecular characterization such as MLST analysis for meningococci are warranted to improve our understanding of the epidemiology of meningococcal disease in Korea.
Figures and Tables
Table 1
The change of meningococcal carriage rate in Korean army recruits before and after admission to a training camp over a 5-week period [6]
References
1. Khatami A, Pollard AJ. The epidemiology of meningococcal disease and the impact of vaccines. Expert Rev Vaccines. 2010; 9:285–298.

2. Korea Centers for Disease Control and Prevention (KCDC). Infectious disease statistics system. Accessed 18 March 2016. Available at: http://is.cdc.go.kr/dstat/index.jsp.
3. Kang JH, Miao Y, Lee SY, Kim JH, Lee KY, Ma SH, Jo DS, Song HY, Haag M. A survey of serum bactericidal antibodies against Neisseria meningitidis serogroups A, C, W and Y in adolescents and adults in the Republic of Korea. Infect Chemother. 2016; 48:12–19.

4. Caugant DA, Tzanakaki G, Kriz P. Lessons from meningococcal carriage studies. FEMS Microbiol Rev. 2007; 31:52–63.

5. Durey A, Bae SM, Lee HJ, Nah SY, Kim M, Baek JH, Kang YH, Chung MH, Lee JS. Carriage rates and serogroups of Neisseria meningitidis among freshmen in a University dormitory in Korea. Yonsei Med J. 2012; 53:742–747.

6. Hwang IU, Lee HK, Seo MY, Kim JP, Seo YB, Bang YJ. The changes of Meningococcal carriage rate and the serogroup in Korean army recruits. J Korean Mil Med Assoc. 2010; 41:188–199.
7. Jo YM, Bae SM, Kang YH. Cluster of serogroup W-135 meningococcal disease in 3 military recruits. J Korean Med Sci. 2015; 30:662–665.

8. Abad R, López EL, Debbag R, Vazquez JA. Serogroup W meningococcal disease: global spread and current affect on the Southern Cone in Latin America. Epidemiol Infect. 2014; 142:2461–2470.

9. Vyse A, Wolter JM, Chen J, Ng T, Soriano-Gabarro M. Meningococcal disease in Asia: an under-recognized public health burden. Epidemiol Infect. 2011; 139:967–985.

10. Kim SA, Kim DW, Dong BQ, Kim JS, Anh DD, Kilgore PE. An expanded age range for meningococcal meningitis: molecular diagnostic evidence from population-based surveillance in Asia. BMC Infect Dis. 2012; 12:310.

11. Goldschneider I, Gotschlich EC, Artenstein MS. Human immunity to the meningococcus. I. The role of humoral antibodies. J Exp Med. 1969; 129:1307–1326.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download