This article has been
cited by other articles in ScienceCentral.
Dear Editor,
A 46-year-old female patient with acute myeloid leukemia was admitted for the management of grade III acute graft-versus-host disease (GVHD) of gut, liver, and skin, 74 days after successful haploidentical hematopoietic stem cell transplantation. Methylprednisolone (250 mg/day) was started with tacrolimus intravenously (starting dose of 0.5 mg/day, modified according to the serum trough level of 5~15 ng/mL) for the management of GVHD. Despite 8 days of systemic steroid therapy, GVHD was considered as refractory and etanercept (50 mg/week) was added. Posaconazole oral suspension (600 mg/day) and ganciclovir (10 mg/kg/day) were administered for the antifungal prophylaxis and preemptive therapy for cytomegalovirus DNAemia (206,050 IU/ml), respectively. However, on day 14 of posaconazole prophylaxis, serum posaconazole level was subtherapeutic (161.8 ng/mL), and was considered as resulting from poor absorption of posaconazole due to gut GVHD. Since the patient complained swallowing difficulty with oral pain and diagnosed as oral candidiasis, posaconazole was changed into intravenous fluconazole (200 mg/day).
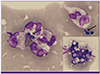
On day 19 of fluconazole treatment, extracellular and intracellular budding yeast cells, phagocytosed by monocytes, were fortuitously identified on peripheral blood smear (
Fig. 1). Complete blood cell count revealed a white blood cell count of 2,240/mm
3 (absolute neutrophil count of 910/mm
3). Fluconazole was changed into caspofungin (70 mg/day loading followed by 50 mg/day) for the treatment of breakthrough yeast infection. Five hours after checking peripheral blood smear, fever developed up to 39.4°C and subsequent blood culture revealed
Candida glabrata (4/4 bottles from both peripheral and central blood) with positive differential time to positivity; time to positivity of central and peripheral blood was 11 hours 5 minutes and 19 hours 4 minutes, respectively. Hickman catheter was removed, and tip culture also revealed the same
C. glabrata (≥15 colonies) as was isolated from blood. Antifungal susceptibility of
C. glabrata showed susceptible to amphotericin B deoxycholate (minimal inhibitory concentration [MIC] ≤0.25 mg/L), caspofungin (MIC ≤0.25 mg/L), and flucytosine (MIC ≤1 mg/L), while intermediate to fluconazole (MIC 16 mg/L), and resistant to voriconazole (MIC ≥8 mg/L). Ophthalmic examination showed there was no evidence of an intraocular lesion. Repeated blood cultures were negative after 2 days from starting caspofungin. Caspofungin was continued for 2 weeks after blood cultures became negative. The patient finally recovered from candidemia and acute GVHD.
Rapid diagnosis and appropriate antifungal treatment significantly impact a prognosis of candidemia, especially in immunocompromised patients [
1]. Despite the recent improvement of the microbiological diagnostic system, confirmatory diagnosis of candidemia is usually made by blood culture [
2]. Peripheral blood smear has low sensitivity to detect infection with unclear diagnostic values, which also depends on the burden of the organism, the degree of heightened vigilance for yeast cells when reviewing stained blood smears, and the selection of a specific patient population [
34]. Intracytoplasmic phagocytosed yeast cells and budding yeast can be indicative of candidemia [
45]. Yeast cells from blood smear could be a clue to early recognition of breakthrough candidemia that can lead to a successful outcome of patients.







 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download