Abstract
To our knowledge, this is the first study that focuses on risk factor of urethral condyloma (UC). The subjects of our study included genital warts patients who had been diagnosed as having condyloma acuminatum of penile skin (CAPS) with/without UC. Relationship with UC of number of life time female partners, co-infection with urethritis, circumcision status, number of CAPS and wart diameter were studied by use of multivariate analysis. Co-infection with urethritis, circumcision status were risk factors of UC in heterosexual young male patients with CAPS. This information will be helpful for providing more professional counseling to patients with genital warts.
Genital warts caused by human papillomavirus (HPV) infection, is the most common sexually transmitted disease (STD) [12]. The most common sites for genital warts in men are the balanopreputial sulcus, frenulum and the glans’ mucosa [3]. Urethral condyloma (UC) is relatively uncommon [4]. Generally, urethral viral infection in male is likely to be difficult, because of the mucosal immune system, even if the penile skin is exposed to HPV. However, it may be possible that HPV is disseminated into the urethra [5]. About 20% of all genital warts caused by HPV are found in the urethra, preferentially on the urethral meatus of the urethra [6]. There are various treatments for UC; as a rule, they are limited by a difficult approach, by recurrences, and by potential complications, the most significant of which is urethral stenosis. However, studies about risk factors of UC are limited worldwide. The objective of this manuscript was report the risk factors of UC among heterosexual young male patients with condyloma acuminatum of penile skin (CAPS). To our knowledge, this is the first study that focuses on risk factor of UC.
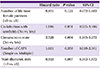
The subjects of our study included genital warts patients who had been diagnosed as having CAPS with/without UC who had been surgically treated from June 2012 to September 2015 (Fig. 1). Condyloma acuminatum (CA) was confirmed by performing a histopathological examination. The mPCR was used to figure out co-infection with urethritis in all patients. In CAPS with UC group, urethro-cystoscopy was performed to rule out intra-urethral and bladder warts. We analyzed age, number of life time female partners, co-infection with urethritis, circumcision status, number of CAPS and wart diameter (maximum size). Student’s t-test and Fisher’s exact test was applied to perform the comparison of patients characteristics between CAPS without UC group and CAPS with UC group. Relationship with UC of number of life time female partners, co-infection with urethritis, circumcision status, number of CAPS and wart diameter were studied by use of multivariate multiple regression analysis. Statistical analysis was carried out by using SPSS 18.0 software (IBM Co., Armonk, NY, USA), and P-values of <0.05 were considered statistically significant. Patients were excluded from the study if they had a history of urethral instrumentation or malformation. The enrolled 179 subjects were all heterosexual males. The subjects characteristics of two groups: age, number of life time female partners, co-infection with urethritis, circumcision status, number of CAPS and wart diameter were illustrated in the Table 1. The co-infection with urethritis was higher in the CAPS with UC group compare to the CAPS without UC group (P = 0.025) (Table 1). The circumcision state was lower in CAPS with UC group compare to the CAPS without UC group (P = 0.006) (Table 1). Multivariate analysis revealed that co-infection with urethritis (hazard ratio [HR] 1.816, P = 0.031) and circumcision state (HR 2.528, P = 0.004) were significantly associated with UC, respectively (Table 2).
Uncircumcised patients with genital warts may have more contact of the HPV infected inner preputial surface with the mucosal surfaces of the urethra meatus. These facts may explain the reason why uncircumcised patients showed higher rate of CAPS with UC group in results of our study. Zvulunov et al. reported that a high prevalence of Ureaplasma urealyticum infection among patients with CA [7]. It was because U. urealyticum antigens have a mitogenic effect on peripheral blood and synovial fluid macrophages. Possibly, this mitogenic effect plays a role in the high prevalence of CA among U. urealyticum positive patients. It is also possible that urethritis patients with CA had some unrevealed risk factors for STD, such as higher number of lifetime partners or different sexual habits. Similarly, in our study, patients who had active urethritis were consistently more to have UC.
Although this survey has several limitations. First, it involves exclusively young male patients between the ages of 18 and 28 years, and therefore should be extrapolated with caution. However, young adults between the ages of 18 and 28 are at high risk for STD, allowing important insights about the prevalence and risk factors of several diseases more or less common to these age groups. Seconds, more variables should be considered including the viral factors. The genotype of HPV and host factors were not evaluated. Further prospective randomized controlled trials should validate the consistency of these associations.
In conclusion, the major finding of our study is that co-infection with urethritis, circumcision status were risk factors of UC in heterosexual young male patients with CAPS. This information will be helpful for providing more professional counseling to patients with genital warts.
Figures and Tables
Table 1
Comparison of patients characteristics between CAPS without UC group and CAPS with UC group

Table 2
Multivariate analysis of relationship with UC
References
1. Scheurer ME, Tortolero-Luna G, Adler-Storthz K. Human papillomavirus infection: biology, epidemiology, andprevention. Int J Gynecol Cancer. 2005; 15:727–746.

2. Lee CS, Park WB, Lee KD, Jang HC, Kang CI, Park SY, Kim JH, Kim HB, Oh MD, Choe KW. Two cases of anal cancer in patient with acquired immunodeficiency syndrome infected by human papillomavirus. Infect Chemother. 2005; 37:50–54.
3. Ting PT, Dytoc MT. Therapy of external anogenital warts and molluscum contagiosum: a literature review. Dermatol Ther (Heidelb). 2004; 17:68–101.

4. Zaak D, Hofstetter A, Frimberger D, Schneede P. Recurrence of condylomata acuminata of the urethra after conventional and fluorescence-controlled Nd:YAG laser treatment. Urology. 2003; 61:1011–1015.

5. Sumino Y, Mimata H, Nomura Y. Urethral condyloma acuminata following urethral instrumentation in an elderly man. Int J Urol. 2004; 11:928–930.

7. Zvulunov A, Medvedovsky E, Biton A, Horowitz S, Vardy D. Association of Ureaplasma urealyticum colonization in male urethra and Condyloma acuminatum
. Isr Med Assoc J. 2000; 2:580–582.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download