Abstract
Background
Materials and Methods
Results
Figures and Tables
Table 1
Polystyrene microtiter plate assay results for three carbepenem-resistant Acinetobacter baumannii strains
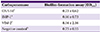
| Carbapenemase | Biofilm-formation assay (OD570) |
|---|---|
| OXA-51a | 0.73±0.62 |
| IMP-1a | 0.66±0.73 |
| VIM-2a | 8.04±2.16 |
| Negative controlb | 0.75±0.35 |
Table 2
Comparison of anti-biofim effects of diverse antibiotics on VIM-2 Acinetobacter baumannii after 48 hours of incubation

aComparison between positive control and each antibiotic regimen.
bNegative control; tests were carried out 36 times and the results were expressed as the mean ± SD.
cPositive control means OD values from the wells where bacteria were inoculated without antibiotics; tests were carried out 36 times and the results were expressed as the mean ± SD.
dTests were carried out six times and the results were expressed as the mean ± SD.
eSusceptible ≤4, resistant ≥8 by British Society for Antimicrobial Chemotherapy.
fSusceptible ≤2, resistant ≥4 by working party report of the British Society for Antimicrobial Chemotherapy.
gSusceptible ≤4, resistant ≥16 by CLSI.
hSusceptible ≤2, resistant ≥8 by Wyeth research.
VIM, verona imipenemase; OD, optical density; SD, standard deviation; MIC, minimum inhibitory concentration; CLSI, Clinical and Laboratory Standards Institute.
Table 3
Comparison of anti-biofim effects of diverse antibiotics on VIM-2 Acinetobacter baumannii after 96 hours of incubation

aComparison between positive control and each antibiotic regimen.
bNegative control; tests were carried out 18 times and the results were expressed as the mean ± SD.
cPositive control means OD values from the wells where bacteria were inoculated without antibiotics; tests were carried out 18 times and the results were expressed as the mean ± SD.
dTests were carried out six times and the results were expressed as the mean ± standard deviation.
eSusceptible ≤2, resistant ≥8 by Wyeth research.
fSusceptible ≤4, resistant ≥8 by British Society for Antimicrobial Chemotherapy.
gSusceptible ≤2, resistant ≥4 by working party report of the British Society for Antimicrobial Chemotherapy.
hSusceptible ≤4, resistant ≥16 by CLSI.
VIM, verona imipenemase; OD, optical density; SD, standard deviation; MIC, minimum inhibitory concentration; CLSI, Clinical and Laboratory Standards Institute.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download