Abstract
Encephalitis associated with antibodies to the N-methyl-D-aspartate receptor (NMDAR) has variable clinical manifestations. Patients are often diagnosed with infectious processes because of prodromal symptoms and autonomic manifestations. Approximately 70% of patients have prodromal symptoms consisting of headache, fever, nausea, vomiting, and diarrhea, along with frequent autonomic manifestations, including tachycardia, and fluctuating blood pressure. A 36-year-old woman presented with uncontrolled fever and skin and soft tissue infections. She had shown psychiatric symptoms and abnormal behavior, and had been diagnosed with bipolar disorder. Antibodies to NMDAR were positive in cerebrospinal fluid (CSF) and serum samples, and pelvic computed tomography detected a large ovarian teratoma. The patient improved dramatically after removal of the teratoma and administration of corticosteroid therapy. When confronted with a young woman with uncontrolled fever and acute psychiatric symptoms, physicians should suspect anti-NMDAR encephalitis.
Anti-N-methyl-D-aspartate receptor (NMDAR) encephalitis is an autoimmune disease that generates antibodies to the NMDA receptor. It typically affects young women and is accompanied by abnormal behavior, seizure, mental deterioration, and dysautonomia [1]. The clinical course begins with viral prodromal symptoms during the first week, followed by insanity symptoms for up to three weeks and neurological symptoms such as severe abnormal movements, hypoventilation, and seizure for several weeks to several months. Sequelae such as impulse disorder and sleep disorder remain for several years [2]. Recently in South Korea, many case reports of this disease have been published, as the neurology department of a university hospital can perform an antibody test for anti-NMDAR encephalitis [3]. In our case, the patient was referred to us following continued fever after hospitalization due to abnormal behavior and frequent mood changes. She had no abnormal findings on brain MRI and cerebrospinal fluid (CSF) testing, but a malformation of the ovary was found and antibodies to NMDAR were found in the blood and CSF, which led to the diagnosis of anti-NMDAR encephalitis. Her continued uncontrollable fever was due to dysautonomia. We report this case because it is critical to check for anti-NMDAR encephalitis as a cause of fever when the patient shows neurological and psychiatric symptoms along with fever.
36-year-old woman who was hospitalized by the psychiatry department due to abnormal behavior and frequent mood changes for 2 days was referred to the department of infectious diseases on day 6 for continued fever, which lasted for 2 more days. She had been healthy with no particular medical history, but complained of chills and headache starting 5 days before her hospitalization. Two days before her hospitalization, she showed frequent mood changes, such as suddenly crying about difficult work and then smiling soon after, saying she felt better. She also complained of visual hallucinations and insomnia, and showed hyperactivity such as desultorily walking around the house. She was diagnosed with type 1 bipolar disorder and was hospitalized by the psychiatry department. After calming down, she remembered everything she had said and done. On the second day of hospitalization, she shouted that she gave birth to a baby and bit her own and her mother's hands, indicating catatonia. She then developed a fever and was referred to the infectious disease department. At the time, the patient looked at other people only when she was called, and she spoke in gibberish with unclear pronunciations. She had strained her limbs, but was not spasmodic. Her temperature was 38.8℃ and she had no headache or nausea. Blood pressure was 150/100 mmHg, heart rate was 109 per minute, and respiratory rate was 23 per minute. She had no catheters in her body. There was no sign of meningism. Her test results for cranial nerves, movement, senses, and reflexes were normal. She had lacerations on her right thumb and left forefinger. The nail bed of her right thumb required a suture. The brain MRI conducted on the first day of her hospitalization showed no special findings. Due to continued catatonia and abnormal behavior, the patient was administered lorazepam and valproic acid. The hematologic test results showed a white blood cell count of 13,370/mm3, (neutrophils 73.7%, lymphocytes 19.3%), hemoglobin of 12 g/dL, platelet count of 369,000/mm3, erythrocyte sedimentation rate of 3 mm/H, procalcitonin of 0.06 ng/mL, blood urea nitrogen of 2.84 mg/ dL, creatinine of 0.59 mg/dL, and albumin of 4.26 g/dL. Antinuclear antibodies were negative. C-reactive protein was 1.09 mg/dL, aspartate aminotransferase was 189 IU/L, alanine aminotransferase was 72 IU/L, creatine phosphokinase was 24,406 IU/L, and lactate dehydrogenase was 1,255 IU/L. Because there was a fever after the contaminated wound on her finger and her creatine phosphokinase and lactate dehydrogenase were increased, the fever was judged to be caused by skin soft tissue infection. Thus, cefazolin (1 g every 8 hours) was administered for 7 days. She was vaccinated against tetanus, and tetanus Ig was administered. No strain was identified from the blood culture, but Enterococcus faecalis was identified in the wound culture. The wound improved but the fever continued so the medication was changed to levofloxacin (750 mg/day), which was administered for 5 days. After that, her fever continued at 37.8℃ to 38.9℃, so the drug was changed to ampicillin/sulbactam (2,000/1,000 mg every 8 hours). No strain was identified on repeated blood cultures, and no heart noise was detected by stethoscope. Her creatine phosphokinase and lactate dehydrogenase decreased to normal ranges during week 3 of her hospitalization.
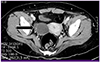
The patient's fever and abnormal behavior continued, so her CSF was tested on day 21 of her hospitalization. The CSF pressure was 10 cm H2O, proteins were 26.19 mg/dL, sugar was 78 mg/dL, and white blood cells were 2/mm3 (lymphocytes 100%). There were no red blood cells. A pelvic CT on day 26 of the hospitalization found a 5.5 cm mixed density in the right adnexa, which was mixed with a 2.5 × 1.3 cm cyst, adipose tissues, and a calcified area (Fig. 1). The patient was diagnosed with anti-NMDAR encephalitis and methylprednisolone (1 g/day) was administered. On day 28, the right adnexa was removed laparoscopically. The tissue findings indicated a mature cystic teratoma. On day 29 of the hospitalization, which was the third day of steroid administration and 2 days after the operation, the patient's fever was alleviated. After 5 days of administration of methylprednisolone, it was changed to dexamethasone (10 mg/day for 14 days). On day 40 of her hospitalization, nonspecific slow waves appeared on the electroencephalogram. On day 46 of her hospitalization, the patient's mini-mental state examination score was 27. She was discharged and her medication was changed to 60 mg of oral prednisolone, which was slowly reduced until it was fully stopped after 4 weeks. At present, she is leading a normal life with no signs of type 1 bipolar disorder, and is under follow up. Antibodies to NMDAR were positive in CSF and serum samples.
This is a case report of the diagnosis of anti-NMDAR encephalitis as a cause of fever that developed during the hospitalization of a patient in the psychiatry department due to abnormal behavior and insanity symptoms. After it was reported in 2005 that 4 women with ovarian teratoma showed symptoms such as memory loss, insanity, metal deterioration, and decreased respiration, the possibility of paraneoplastic syndrome was raised. Later, anti-NMDAR encephalitis received much attention and has been frequently reported since the discovery of antibodies to NMDAR was reported by Dalmau, et al. in 2007 [14]. NMDAR is involved in the formation and memory of synapses and is an isoform of the NR1 subunit that combines with glycin and the NR subunit, which combines with glutamate. Anti-NMDAR encephalitis has been found to be caused by immunoglobulin (Ig)-G1 and IgG3, which combine with the NR1 subunit [5].
The prevalence of anti-NMDAR encephalitis is not accurately known, but it accounts for about 37-50% of encephalitis cases of unknown origin [67]. A prospective multicenter study on the cause of encephalitis in the United Kingdom found that anti-NMDAR encephalitis accounted for approximately 4% of cases and was the next most frequent cause after acute disseminated encephalomyelitis [6]. In the California Encephalitis Project, anti-NMDAR encephalitis appeared in 4.2% of patients aged 30 or under and was the most frequent cause of encephalitis of unknown origin [7]. In South Korea, a university conducted a test of antibodies to NMDAR in 721 patients with encephalitis of unknown origin, and 40 of them were positive [3]. Therefore, anti-NMDA receptor encephalitis seems to be not uncommon. A test of the antibodies to NMDAR will help in the diagnosis in cases of encephalitis of unknown origin.
Seventy percent of patients start with symptoms similar to a cold, such as nausea, fever, headache, and fatigue [58]. Psychiatric symptoms appear within 2 weeks and may include cognitive disorders such as confusion and memory loss, insanity such as paranoia, hallucinations, agitation, depression, anxiety, and automutilation, as well as convulsions. These symptoms are often misdiagnosed as schizophrenia or bipolar disorder. For several weeks to several months, neurological complications may lead to hypoventilation and trance, which requires mechanical ventilation. After that, the patient may exhibit sequelae such as impulse disorder and sleep disorder for several months to several years. Our case also showed abnormal behavior and fever as initial symptoms, but the cause of the fever was mistaken as skin and soft tissue infection because she had lacerated wounds on her right thumb and left forefinger and was treated with antibiotics, which brought about difficulty in the diagnosis.
Ovarian teratoma is often discovered in anti-NMDAR encephalitis. It has been found that ovarian teratoma is associated with a higher frequency of the characteristic symptoms of anti-NMDAR encephalitis and the removal of the teratoma improves the symptoms more quickly and decreases recurrences [9]. In the present case, a cystic teratoma was discovered in the right adnexa on a pelvic CT after anti-NMDAR encephalitis was suspected as the cause of the fever of unknown origin. The adnexa was immediately removed and the patient's fever was alleviated by the second day after the operation.
If examination findings are not characteristic, an NMDAR antibody test can be conducted on the serum and CSF. If the result is positive, ultrasound, CT, and MRI tests are conducted to look for a tumor. If no tumor is found, high dose steroid shock therapy and immunoglobulin or plasma exchange should be considered [8]. If the patient shows a good response to treatment, he/she will need conservative treatment, and sustained treatment with immunosuppressants such as mycophenolate mofetil is required, as well as periodic follow up because of the possibility of future tumor development. If there is a tumor, high dose steroid shock therapy and immunoglobulin or plasma exchange should be considered when the tumor is removed. If the patient is not responsive to the treatment, rituximab, cyclophosphamide, or both could be used. At present, our patient has slowly decreased and stopped the steroids without using any immunosuppressants, and she is now under follow up.
Recovery is generally slow, and often requires rehabilitation treatment for a few months [5]. However, some patients have continued problems with cognitive functions such as under standing, memory, concentration, and expression, and with motor functions such as walking and swallowing. A two-year follow up study found that about 80% of the patients showed good results (modified Rankin scale of 0-2). Patients who did not use immunosuppressants in the early stage and patients who did not receive treatment in the intensive care unit showed a better prognosis. The recurrence rate was about 12%, which increased in cases with no tumor [10]. The mortality for 24 months was about 7%.
The present case report shows that the possibility of anti-NMDAR encephalitis should be considered in patients with fever of unknown origin who exhibit insanity symptoms, because it is not uncommon. The presence of a tumor must be determined immediately and the tumor must be removed if one is found, and steroid or immunoglobulins must then be used quickly.
Figures and Tables
References
1. Dalmau J, Tüzün E, Wu HY, Masjuan J, Rossi JE, Voloschin A, Baehring JM, Shimazaki H, Koide R, King D, Mason W, Sansing LH, Dichter MA, Rosenfeld MR, Lynch DR. Paraneoplastic anti-N-methyl-D-aspartate receptor encephalitis associated with ovarian teratoma. Ann Neurol. 2007; 61:25–36.

2. Kayser MS, Dalmau J. Anti-NMDA receptor encephalitis, autoimmunity, and psychosis. Schizophr Res. 2014; [Epub ahead of print].

3. Lim JA, Lee ST, Jung KH, Kim S, Shin JW, Moon J, Byun JI, Kim TJ, Shin YW, Lee KJ, Kim YS, Park KI, Lee SK, Chu K. Anti-N-methyl-d-aspartate receptor encephalitis in Korea: clinical features, treatment, and outcome. J Clin Neurol. 2014; 10:157–161.

4. Vitaliani R, Mason W, Ances B, Zwerdling T, Jiang Z, Dalmau J. Paraneoplastic encephalitis, psychiatric symptoms, and hypoventilation in ovarian teratoma. Ann Neurol. 2005; 58:594–604.

5. Mann AP, Grebenciucova E, Lukas RV. Anti-N-methyl-D-aspartate-receptor encephalitis: diagnosis, optimal management, and challenges. Ther Clin Risk Manag. 2014; 10:517–525.

6. Granerod J, Ambrose HE, Davies NW, Clewley JP, Walsh AL, Morgan D, Cunningham R, Zuckerman M, Mutton KJ, Solomon T, Ward KN, Lunn MP, Irani SR, Vincent A, Brown DW, Crowcroft NS. UK Health Protection Agency (HPA) Aetiology of Encephalitis Study Group. Causes of encephalitis and differences in their clinical presentations in England: a multicentre, population-based prospective study. Lancet Infect Dis. 2010; 10:835–844.

7. Gable MS, Sheriff H, Dalmau J, Tilley DH, Glaser CA. The frequency of autoimmune N-methyl-D-aspartate receptor encephalitis surpasses that of individual viral etiologies in young individuals enrolled in the California Encephalitis Project. Clin Infect Dis. 2012; 54:899–904.

8. Dalmau J, Lancaster E, Martinez-Hernandez E, Rosenfeld MR, Balice-Gordon R. Clinical experience and laboratory investigations in patients with anti-NMDAR encephalitis. Lancet Neurol. 2011; 10:63–74.

9. Dalmau J, Gleichman AJ, Hughes EG, Rossi JE, Peng X, Lai M, Dessain SK, Rosenfeld MR, Balice-Gordon R, Lynch DR. Anti-NMDA-receptor encephalitis: case series and analysis of the effects of antibodies. Lancet Neurol. 2008; 7:1091–1098.

10. Titulaer MJ, McCracken L, Gabilondo I, Armangué T, Glaser C, Iizuka T, Honig LS, Benseler SM, Kawachi I, Martinez-Hernandez E, Aguilar E, Gresa-Arribas N, Ryan-Florance N, Torrents A, Saiz A, Rosenfeld MR, Balice-Gordon R, Graus F, Dalmau J. Treatment and prognostic factors for long-term outcome in patients with anti-NMDA receptor encephalitis: an observational cohort study. Lancet Neurol. 2013; 12:157–165.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download