Abstract
We investigated the antibiotic susceptibility of glycopeptide-resistant enterococci (GRE). Seventy consecutive GRE were tested. Sixty-two isolates were identified as Enterococcus faecium (88.6%), and 8 (11.4%) as Enterococcus faecalis. All strains were susceptible to linezolid and daptomycin, while 17.1% (12/70) and 11.4% (8/70) were resistant to quinupristin/dalfopristin (QD) and tigecycline, respectively. All E. faecalis isolates were resistant to QD, while 4 of 62 (6.5%) E. faecium isolates were resistant to QD. All E. faecalis isolates were susceptible to tigecycline, while 14.5% (9/62) E. faecium isolates were resistant. Continued surveillance of GRE antibiotic susceptibilities is important for combating these multi-resistant nosocomial pathogens.
Glycopeptide resistant enterococci (GRE) were first reported in Europe in 1988, and have since then been implicated as causative pathogens in nosocomial infections worldwide [1, 2]. In US hospitals, the number of infections caused by vancomycin resistant enterococci (VRE) increased from 9,820 in 2000 to 21,352 in 2006 [3]. GRE tend to colonize and infect immunocompromised hospitalized patients on prolonged courses of antibiotics [4]. These strains are generally resistant not only to vancomycin and teicoplanin, but also to various other antimicrobials due to intrinsic (low-level resistance to β-lactams and aminoglycosides) and acquired (high-level resistance to aminoglycosides) mechanisms. The emergence of resistance to newer classes of antibiotics is particularly worrisome, since it severely limits the available treatment options. The problem is further compounded by the potential transfer of GRE resistance genes to other pathogenic organisms, such as Staphylococcus aureus and Streptococcus species.
Several new antimicrobials demonstrate in vitro activity against GRE, namely linezolid, daptomycin, quinupristin/dalfopristin and tigecycline. Linezolid and tigecycline inhibit at low concentration both Enterococcus faecalis and Enterococcus faecium, daptomycin is more active against E. faecalis, while quinupristin/dalfopristin has substantial activity only against E. faecium [5].
The present microbiological study was performed to investigate the current susceptibility patterns of GRE isolated over a three year period from a variety of patients cared for in the University General Hospital of Heraklion, the only tertiary general hospital in the island of Crete, Greece against linezolid, quinupristin/dalfopristin, tigecycline and daptomycin.
All clinical samples were cultured in Enterococcus broth and bile esculin azide agar supplemented with 6 mg/L of vancomycin. Plates and broths were incubated at 37℃ for 24 hours. Esculin-positive broth cultures were subcultured onto bile esculin azide agar plates with 6 mg/L of vancomycin and incubated for 24 hours. Species level identification was performed by conventional methods, i.e., biochemical characteristics, motility, pigment production and the API® 20 Strep system (BioMérieux, Marcy L' Etoile, France). Identification was confirmed with the VITEK 2 automated system (BioMérieux), which has been shown to be reliable in identification of clinical Enterococcus isolates [6]. Resistance to vancomycin and teicoplanin was determined by the disk diffusion method, as recommended by the Clinical and laboratory standards institute (CLSI) [7] and the E-test method (BioMérieux). Resistance to linezolid, quinupristin/dalfopristin, tigecycline and daptomycin was determined by E-test.
A total of 70 consecutive GRE samples were tested from 67 patients, including 44 males (65.7%) and 23 females (34.3%). GRE positive samples originated from the Intensive Care Unit (18), and the Departments of Hematology (8), Internal Medicine (8), Nephrology (7), Gastroenterology (6), Oncology (3), Neurosurgery (3), Vascular Surgery (3), Cardiology including the Intensive Care Cardiology Unit (2), General Surgery (2), Surgical Oncology (2), Orthopedics (2), Emergency Medicine (2), Neurology (1), Pulmonology (1), Thoracic Surgery (1), and Pediatrics (1). GRE positive samples were collected from a variety of body fluids and sites, including blood (22), urine (18), pus from skin lesions including decubitus ulcers and soft tissue infections (11), ascitic fluid (4), peritoneal dialysis fluid (4), sputum (2), bronchoalveolar lavage (2), bone (2), tip of intravascular catheters (2), pleural fluid (1), bile (1), and Cerebrospinal fluid (CSF) (1). Three patients provided two positive samples each for glycopeptide-resistant E. faecium with different susceptibility patterns at different time-points. More specifically, a 63-year-old woman had two positive cultures from blood and pus, a 72-year-old man had two positive urine cultures collected from a nephrostomy tube on two occasions separated by10 months, and a 51-year-old woman had two positive cultures from blood and an infected decubitus ulcer.
Median age of patients was 65 years (range 0.1-96), and did not differ by sex (men 65.4±15.4 versus women 64.5±17.5 years, P = 0.82). The majority of patients besides advanced age had some underlying chronic disease and/or immunosuppression, including renal or liver failure, chronic neurologic disease, hematologic malignancy or solid tumor. All had received prior courses of several antibiotics.
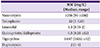
Among the 70 GRE isolates, 62 were identified as E. faecium (88.6%), and 8 (11.4%) as E. faecalis. Median value and range of the minimal inhibitory concentrations (MIC) against the tested antimicrobials is shown in Table 1. As shown, 100% of the isolated GRE strains were susceptible to linezolid and daptomycin, while 17.1% (12/70) and 11.4% (8/70) were resistant to quinupristin/dalfopristin and tigecycline, respectively. The antibiotic susceptibility patterns were species-specific. Thus, 100% of E. faecalis isolates were resistant to quinupristin/dalfopristin, while only 4 of 62 (6.5%) E. faecium isolates were resistant and 1 was partially resistant (intermediate susceptibility) to quinupristin/dalfopristin (P < 0.0001 by Fisher's exact test). Regarding tigecycline, all 8 E. faecalis isolates were susceptible to it, while 14.5% (9/62) E. faecium isolates were resistant (P = 0.58).
Vancomycin resistance is more common among E. faecium than E. faecalis isolates [8]. Hence, the observed distribution of GRE in our study was not unexpected, and is very similar to the current situation reported from several countries like Brazil and USA, where > 89-90% of VRE isolates are E. faecium [9, 10]. Regarding European countries, the majority of 902 VRE isolated from 2006 to 2008 in France were also E. faecium (94.8%) [11].
None of our GRE isolates were resistant to linezolid. In the study by Bourdon et al, no tested isolate among 602 E. faecium and 30 E. faecalis was resistant to linezolid [11]. In a previous study from Greece originating from 8 tertiary-care hospitals, not including ours, and reporting on VRE isolates collected in 2007, resistance to linezolid was detected in only 1.9% of E. faecium isolates [12]. In yet another study from a university hospital of Northern Greece, linezolid resistance was noted among only 0.3% and 1.6% of all E. faecalis and E. faecium isolates, respectively [13].
Regarding quinupristin/dalfopristin, approximately 6.5% of our E. faecium and 100% of our E. faecalis isolates were resistant to it. Resistance rates of 98.2% to 100% to quinupristin/dalfopristin have been described among E. faecalis isolates in Europe and North America. It is noteworthy that higher resistance rates to quinupristin/dalfopristin have been observed among European compared to North American E. faecium strains (10% versus 0.6%) [14].
Regarding tigecycline, we had no resistant E. faecalis isolates. On the other hand, 14.5% of our glycopeptide-resistant E. faecium isolates were resistant to this glycylcycline antibiotic, a higher than previously described figure. This is likely due to the frequent use of tigecycline among critically ill patients in our hospital, since tigecycline resistance is selected mainly by its use [15]. In a study from Korea describing susceptibility of clinical VRE isolates collected over the period 1998 to 2005 to mupirocin and the four antibiotics used in our study, tigecycline was the most active agent in vitro [16]. Among 219 vancomycin-resistant E. faecium isolates collected in 20 Taiwanese hospitals from 2006 to 2010, all of which were susceptible to linezolid and daptomycin, 1.4% were resistant to tigecycline [17]. In the study by Bourdon et al, none of the 602 E. faecium and 30 E. faecalis tested isolates was resistant to tigecycline [11]. In the longitudinal 2004-2011 assessment of organisms collected from Italy as part of the tigecycline evaluation and surveillance trial, susceptibility to tigecycline was noted among 94.5% of vancomycin-resistant E. faecium and 100% of E. faecalis isolates [18].
Finally regarding daptomycin, all tested GRE isolates of our study were susceptible to it. Daptomycin has shown excellent in vitro activity against enterococci collected from European medical centers, and it is of note that neither resistance to vancomycin nor quinupristin/dalfopristin compromised its activity [19]. In our isolates, it was particularly active against E. faecalis, as previously shown by others [20].
Our study is somewhat limited by the very small number of E. faecalis isolates. On the other hand, our data are much more robust regarding E. faecium, an important and rising pathogen in our hospital.
In conclusion, we describe the susceptibilities of 70 GRE clinical isolates from a single tertiary hospital of Greece to linezolid, quinupristin/dalfopristin, tigecycline and daptomycin. Judicious antibiotic utilization practices must be constantly implemented in order to limit the further emergence of GRE and of other resistant nosocomial pathogens. To this extend, continued surveillance of GRE antibiotic susceptibilities at the local, national and international levels is of paramount importance for combating these tough to kill and increasingly dangerous nosocomial microorganisms.
Figures and Tables
References
1. Lautenbach E, Bilker WB, Brennan PJ. Enterococcal bacteremia: risk factors for vancomycin resistance and predictors of mortality. Infect Control Hosp Epidemiol. 1999; 20:318–323.

2. DiazGranados CA, Jernigan JA. Impact of vancomycin resistance on mortality among patients with neutropenia and enterococcal bloodstream infection. J Infect Dis. 2005; 191:588–595.

3. Ramsey AM, Zilberberg MD. Secular trends of hospitalization with vancomycin-resistant enterococcus infection in the United States, 2000-2006. Infect Control Hosp Epidemiol. 2009; 30:184–186.

4. Yeh KM, Siu LK, Chang JC, Chang FY. Vancomycin-resistant enterococcus (VRE) carriage and infection in intensive care units. Microb Drug Resist. 2004; 10:177–183.

5. Dobbs TE, Patel M, Waites KB, Moser SA, Stamm AM, Hoesley CJ. Nosocomial spread of Enterococcus faecium resistant to vancomycin and linezolid in a tertiary care medical center. J Clin Microbiol. 2006; 44:3368–3370.

6. Fang H, Ohlsson AK, Ullberg M, Ozenci V. Evaluation of species-specific PCR, Bruker MS, VITEK MS and the VITEK 2 system for the identification of clinical Enterococcus isolates. Eur J Clin Microbiol Infect Dis. 2012; 31:3073–3077.

7. Clinical and Laboratory Standards Institute (CLSI). Performance standards for antimicrobial susceptibility testing; Twenty-third informational supplement. CLSI Document M100-S23. Wayne, PA: CLSI;2013.
8. Henwood CJ, Livermore DM, Johnson AP, James D, Warner M, Gardiner A. The Linezolid Study Group. Susceptibility of gram-positive cocci from 25 UK hospitals to antimicrobial agents including linezolid. J Antimicrob Chemother. 2000; 46:931–940.

9. Conceição N, Oliveira Cda C, Silva PR, Avila BG, Oliveira AG. Trends in antimicrobial resistance among clinical isolates of enterococci in a Brazilian tertiary hospital: a 4-year study. Rev Soc Bras Med Trop. 2011; 44:177–181.

10. Arias CA, Murray BE. Antibiotic-resistant bugs in the 21st century--a clinical super-challenge. N Engl J Med. 2009; 360:439–443.

11. Bourdon N, Fines-Guyon M, Thiolet JM, Maugat S, Coignard B, Leclercq R, Cattoir V. Changing trends in vancomycin-resistant enterococci in French hospitals, 2001-08. J Antimicrob Chemother. 2011; 66:713–721.

12. Damani A, Klapsa D, Panopoulou M, Spiliopoulou I, Pantelidi K, Malli E, Kolonitsiou F, Grapsa S, Alepopoulou E, Frantzidou F, Vlahaki E, Koutsia-Carouzou C, Malamou-Lada H, Zerva L, Kartali-Ktenidou S, Anastassiou ED, Maniatis AN, Petinaki E. A newly described vancomycin-resistant ST412 Enterococcus faecium predominant in Greek hospitals. Eur J Clin Microbiol Infect Dis. 2010; 29:329–331.

13. Protonotariou E, Dimitroulia E, Pournaras S, Pitiriga V, Sofianou D, Tsakris A. Trends in antimicrobial resistance of clinical isolates of Enterococcus faecalis and Enterococcus faecium in Greece between 2002 and 2007. J Hosp Infect. 2010; 75:225–227.

14. Deshpande LM, Fritsche TR, Moet GJ, Biedenbach DJ, Jones RN. Antimicrobial resistance and molecular epidemiology of vancomycin-resistant enterococci from North America and Europe: a report from the SENTRY antimicrobial surveillance program. Diagn Microbiol Infect Dis. 2007; 58:163–170.

15. Sun Y, Cai Y, Liu X, Bai N, Liang B, Wang R. The emergence of clinical resistance to tigecycline. Int J Antimicrob Agents. 2013; 41:110–116.

16. Lee do K, Kim Y, Park KS, Yang JW, Kim K, Ha NJ. Antimicrobial activity of mupirocin, daptomycin, linezolid, quinupristin/dalfopristin and tigecycline against vancomycin-resistant enterococci (VRE) from clinical isolates in Korea (1998 and 2005). J Biochem Mol Biol. 2007; 40:881–887.

17. Tsai HY, Liao CH, Chen YH, Lu PL, Huang CH, Lu CT, Chuang YC, Tsao SM, Chen YS, Liu YC, Chen WY, Jang TN, Lin HC, Chen CM, Shi ZY, Pan SC, Yang JL, Kung HC, Liu CE, Cheng YJ, Liu JW, Sun W, Wang LS, Ko WC, Yu KW, Chiang PC, Lee MH, Lee CM, Hsu GJ, Hsueh PR. Trends in susceptibility of vancomycin-resistant Enterococcus faecium to tigecycline, daptomycin, and linezolid and molecular epidemiology of the isolates: results from the Tigecycline In vitro Surveillance in Taiwan (TIST) study, 2006 to 2010. Antimicrob Agents Chemother. 2012; 56:3402–3405.

18. Stefani S, Dowzicky MJ. Longitudinal assessment of antimicrobial susceptibility among Gram-negative and Gram-positive organisms collected from Italy as part of the tigecycline evaluation and surveillance trial between 2004 and 2011. Pharmaceuticals (Basel). 2013; 6:1381–1406.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download