Abstract
The prevalence of carbapenem-resistant gram-negative bacterial pathogens (CRGNs) has increased dramatically during the last 10 years, but the optimal treatment for CRGN infections is not well established due to the relative scarcity of robust clinical data. The polymyxins remain the most consistently active agents against CRGNs in vitro. Tigecycline, based on its in vitro antibacterial spectrum, could also be considered as a therapeutic option in the treatment of infections caused by certain CRGNs. Other agents, including aminoglycosides, rifampin, trimethoprim-sulfamethoxazole, fosfomycin and fluoroquinolones, could be considered as monotherapy or combination therapy against CRGNs in appropriate contexts, as combination therapy with two or more in vitro active drugs appears to be more effective than monotherapy based on some clinical data. Several promising new agents are in late-stage clinical development, including ceftolozane-tazobactam, ceftazidime-avibactam and plazomicin. Given the shortage of adequate treatment options, containment of CRGNs should be pursued through implementation of adequate infection prevention procedures and antimicrobial stewardship to reduce the disease burden and prevent future outbreaks of CRGNs.
Carbapenems (ertapenem, imipenem, meropenem, and doripenem) are often considered the last resort agents reserved for treatment of infections due to highly antimicrobial-resistant organisms such as Pseudomonas aeruginosa, Acinetobacter baumannii, and Enterobacteriaceae producing extended-spectrum β-lactamase (ESBL) or plasmid-mediated AmpC β-lactamase. However, the prevalence of carbapenem-resistant gram-negative pathogens has increased dramatically in the last decade [1]. The most common and clinically relevant mechanism underlying carbapenem resistance is production of carbapenem-hydrolyzing β-lactamases, or carbapenemeases, which often confer resistance not only to carbapenems but to most β-lactam agents. Many factors, such as antimicrobial use in humans and food animals, international travel, migration, and importation of food products, contribute to the emergence and spread of these organisms far beyond their countries of origin. The current and extensive spread of carbapenem-resistant gram-negative pathogens is a cause for concern since they are also frequently resistant to non-β-lactam agents, therefore presenting with multidrug resistance (MDR), or even extensive drug resistance (XDR).
The aim of this review is to summarize treatment considerations for six representative gram-negative pathogens which clinicians commonly encounter in hospitals in the context of carbapenem resistance: 1) Acinetobacter baumannii, 2) Pseudomonas aeruginosa, 3) Klebsiella pneumoniae, 4) Escherichia coli, 5) Enterobacter spp., and 6) Stenotrophomonas maltophilia. We will focus our discussion on the management of infections caused by carbapenem-resistant strains, and also MDR and XDR strains as appropriate.
Carbapenemases are the β-lactamases with the widest spectrum of activity in general (Table 1). In addition to carbapenems, carbapenemases also hydrolyze most other members of the β-lactam family with a few exceptions. On the basis of their molecular structure, carbapenemases are classified into Ambler's class A, B, or D enzymes [2]. The plasmid-borne, class A Klebsiella pneumoniae carbapenemases (KPCs) are currently the most prevalent and widely distributed carbapenemases [3]. Detection of KPC-producing organisms in microbiology laboratories is not always straightforward because some isolates display minimum inhibitory concentrations (MICs) against imipenem or meropenem that remain in the susceptible range. In vitro studies have suggested that ertapenem is the most sensitive carbapenem substrate for detection of KPC production [4]. Other clinically important carbapenemases include the class B metallo-β-lactamases (MBLs; e.g., NDMs, IMPs, VIMs) and the class D OXA-type carbapenemases (e.g., OXA-23 in A. baumannii and OXA-48 in K. pneumoniae). The latter group is unique in that they hydrolyze penicillins and carbapenems but not cephalosporins. These carbapenemase genes are borne on plasmids, which can facilitate their intra- and interspecies dissemination. Besides carbapenemase production, these organisms may exhibit additional carbapenem resistance mechanisms, such as augmentation of efflux pumps and porin loss that can further elevate carbapenem MICs [5].
A. baumannii has become a major healthcare-associated pathogen worldwide in the last two decades [6]. The common and challenging presentations include ventilator-associated pneumonia, bacteremia, and wound infection. Mortality from invasive A. baumannii infection is high for carbapenem-resistant isolates, with crude mortality ranging from 16 to 76%, which is higher than the mortality of 5 to 53% from infections with carbapenem-susceptible isolates [7]. In the treatment of carbapenem-resistant A. baumannii infection, colistin, tigecycline and sulbactam (as part of ampicillin-sulbactam or cefoperazone-sulbactam) are often used alone or in various combinations.
Polymyxins (colistin and polymyxin B) exert their bactericidal activity through interactions with lipid A on the outer membrane and are active against most gram-negative species with a few exceptions (e.g. Serratia marcescens, Proteus spp., Providencia spp.) Between colistin and polymyxin B, colistin is used more extensively worldwide due to its better availability. Among Acinetobacter clinical isolates collected from hospitals in the United States in 2010, 94.7% were susceptible to colistin [8]. Clinical data on the efficacy of colistin in the treatment of carbapenem-resistant A. baumannii infections are mostly observational, but data from several prospective, randomized studies addressing the efficacy of colistin-based combination therapy are also emerging.
Colistin maintains excellent activity against A. baumannii, but whether treatment of invasive infection due to A. baumannii with this agent alone is adequate has not been definitively established. In a retrospective study of patients with ventilator-associated pneumonia caused by A. baumannii who were treated according to susceptibility of the organism with colistin or imipenem, clinical cure and in-hospital mortality rates were comparable at 57% each and 61.9% and 64.2%, respectively, suggesting that colistin might be a reasonable alternative for imipenem [9]. On the other hand, in another study of invasive infections caused by carbapenem-resistant A. baumannii and treated with a polymyxin or ampicillin-sulbactam, therapy with a polymyxin was an independent risk factor for in-hospital mortality (odds ratio [OR]: 2.07, P = 0.041), but the medial daily dose of colistin was quite low compared with today's standards [10]. Overall, the limited data suggest that colistin likely has clinical efficacy comparable with carbapenem for invasive A. baumannii infection when an adequate dose is used [11].
Nebulized colistin is increasingly utilized in the management of acute A. baumannii infection, with or without intravenous colistin. In a case-control study conducted in Taiwan, patients with respiratory secretions growing MDR A. baumannii eradicated the organism sooner when they were given nebulized colistin, with or without intravenous colistin, compared with when no nebulized colistin therapy was given (8.2 days and 21.5 days; P < 0.001) [12]. However, there were no differences in the in-hospital mortality. In a randomized, open-label trial of 100 patients with MDR gram-negative pathogens including A. baumannii conducted in Thailand, favorable microbiological outcome was achieved significantly more frequently among those receiving both nebulized and intravenous colistin (60.9%) than among those receiving intravenous colistin only (38.2%; P = 0.03), but there was no difference in the rates of favorable clinical outcome in this study, either [13]. Nebulized colistin may therefore expedite microbiological eradication in the airways but has not been associated with clinical benefit.
Sulbactam is a β-lactamase inhibitor which also has intrinsic activity against Acinetobacter spp. including A. baumannii. Ampicillin-sulbactam susceptibility of 63.6% has been reported for Acinetobacter spp. isolates collected from U.S. hospitals in the early 2000s [14]. However, the susceptibility rate declined from 89% in 2003 to 40% in 2008 in one hospital system in the U.S. along with increased use of this agent [15]. Carbapenemases produced by A. baumannii, such as OXA-23, do not affect sulbactam. Therefore, some carbapenem-resistant strains remain susceptible to sulbactam, making it a potentially useful alternative.
A head-to-head comparison of ampicillin-sulbactam and colistin was made in a small randomized study, where 28 patients with ventilator-associated pneumonia due to XDR A. baumannii received either ampicillin-sulbactam (9 g of sulbactam/day) or colistin (270 mg colistin base activity [CBA]/day) [16]. The clinical response rates, bacteriological success rates, 14- and 28-day mortality rates and the rates of adverse events were all comparable between the two groups. These limited data suggest that sulbactam-containing regimens may have a role in the treatment of infections caused by carbapenem-resistant A. baumannii that remain susceptible to sulbactam.
Tigecycline is a glycylcycline derivative of minocycline which was designed to circumvent common tetracycline resistance mechanisms. It has unique pharmacokinetics with a large volume of distribution resulting in low serum peak concentration of 0.7 to 0.8 µg/mL after the standard loading dose of 100 mg [17]. The use of tigecycline for bacteremia is controversial for this reason. An infection-related mortality of 56% has been reported for patients with carbapenem-resistant A. baumannii bloodstream infection who were treated with tigecycline despite in vitro susceptibility in a small series [18]. In a larger case series on the use of tigecycline for XDR A. baumannii infections, 266 patients were treated with tigecycline alone or in combination with another agent (a carbapenem, expanded-spectrum cephalosporin or piperacillin-tazobactam), and 120 were treated with imipenem and sulbactam [19]. The patients who received tigecycline were less ill, evidenced by significantly lower rates of intensive care unit stay, febrile illness, abnormal serum creatinine and sepsis. There was no difference in 30-day mortality between the two groups, and a lower percentage of patients experienced unfavorable clinical outcome in the tigecycline group (30.8% and 50.0%; P < 0.001). On the other hand, in a series of 9 patients who received tigecycline for bacteremia due to tigecycline-susceptible, carbapenem-resistant A. baumannii, 5 (56%) deaths were related to bacteremia and 1 breakthrough carbapenem-resistant Acinetobacter baumannii bacteremia case was observed during therapy with tigecycline [18]. It has been suggested in a randomized study of hospital-acquired pneumonia that a higher dose of tigecycline (a loading dose of 200 mg followed by 100 mg instead of the approved 50 mg twice a day) may improve the clinical response rate without increasing adverse events, but there were too few patients with A. baumannii pneumonia in this study to draw definitive conclusions [20]. Overall, tigecycline may have a role in the definitive therapy of carbapenem-resistant A. baumannii infections when the patients are not severely ill, but it should probably be avoided for critically ill patients, at least as monotherapy.
Minocycline, like tigecycline, inhibits the 30S ribosomal subunits. It is more active against A. baumannii than doxycycline which is prone to efflux-mediated resistance. In a surveillance study of MDR A. baumannii isolates collected in the U.S., 72.1% were susceptible to minocycline despite a very low susceptibility rate to carbapenems (8.7%) [21]. Clinical data on the use of this agent are scarce. In a series of 8 military patients treated with oral minocycline for traumatic wound infections due to MDR A. baumannii, minocycline therapy resulted in clinical cure in 7 of the patients [22]. In another small series, 4 patients with ventilator-associated pneumonia due to XDR A. baumannii were treated with intravenous minocycline [23]. All 4 patients had clinical improvement, and 3 of them had microbiologic clearance as well. While clinical data are lacking, the compelling in vitro activity suggests that minocycline should be studied further in the context of de-escalation therapy given the availability of oral formulations.
Rifampin by itself is not considered for treatment of A. baumannii infection due to rapid emergence of resistance, but its potential role as an adjunct to other active agents has been explored. In an open-label, randomized trial comparing the efficacy of colistin and colistin plus rifampin for ventilator-associated pneumonia due to carbapenem-resistant A. baumannii, 22 patients were treated with colistin alone, and 21 patients were treated with the combination [24]. The baseline patient characteristics were largely comparable. The crude in-hospital mortality and pneumonia-related mortality were higher for the colistin group (72.7% and 63.6%) compared with the combination group (61.9% and 38.1%), though the differences did not reach statistical significance. No hepatotoxicity from rifampin was observed. Another study was conducted in Italy as a multicenter, open-label, randomized trial comparing the efficacy of colistin and colistin plus rifampin [25]. A total of 210 patients with life-threatening infection due to XDR, colistin-susceptible A. baumannii were enrolled. The baseline characteristics were again comparable between the groups. There was no mortality difference between the two groups (43.4% for the combination group, 42.9% for the colistin group), although the microbiologic eradication rate was significantly higher in the combination group (60.6% and 44.8%; P = 0.034). Hepatic dysfunction was more common in the combination group, but the difference was not statistically significant (20.8% and 11.9%; P = 0.13). These data suggest that the addition of rifampin to colistin may facilitate microbiological clearance of A. baumannii but is unlikely to convey clinical benefit in terms of improved patient survival.
Fosfomycin is not active against A. baumannii, but in vitro synergy has been reported between fosfomycin and colistin or sulbactam [26], and a pilot randomized controlled trial has been conducted comparing the efficacy of colistin and colistin plus fosfomycin for infections caused by carbapenem-resistant A. baumannii [27]. In this study of 94 patients, fosfomycin was given at 4 g every 12 hours intravenously, and therapy was given for 7 to 14 days. The two groups did not differ in favorable clinical outcomes (59.6% and 55.3%) or mortality at 28 days (46.8% and 57.4%), whereas microbiological eradication rates were significantly higher in the combination group (100% and 81.2%; P = 0.01). The small size of the study precludes definitive conclusions, and dosing of fosfomycin was relatively conservative. Nonetheless, this combination may merit further investigation given the trend for lower mortality in the combination group coupled with the favorable safety profile of fosfomycin.
In an observational study of 250 XDR A. baumannii bloodstream infections, 36 patients received colistin monotherapy and 214 patients received colistin-based combination therapy, including 102 with a carbapenem, 69 with ampicillin-sulbactam or sulbactam, and 43 with other agents [28]. The baseline characteristics were comparable among the 4 groups, and all isolates were susceptible to colistin. The in-hospital mortality rate was significantly lower in the colistin-based combination groups compared to the colistin monotherapy group (52.3 % and 72.2 %; P = 0.03), and the rate of microbiological eradication was significantly higher in the combination groups than the monotherapy group (79.9 % and 55.6 %; P = 0.001). In another observational study of 69 patients with solid organ transplantation who developed XDR A. baumannii infection, treatment with a combination of colistin and a carbapenem was an independent predictor of survival [29]. While these data are limited by the observational and retrospective nature of the studies they are derived from, they overall support the use of colistin-containing combination regimens for the treatment of invasive carbapenem-resistant and XDR A. baumannii infections.
Eravacycline is a novel fluorocycline with activity against gram-positive and gram-negative pathogens in vitro, including A. baumannii. Among 52 A. baumannii isolates displaying resistance to carbapenems, fluoroquinolones, and aminoglycosides, MIC50/90 values of eravacycline were 0.5/2 µg/mL [30]. A phase 2, randomized, double-blind study was conducted to evaluate the efficacy and safety of eravacycline in comparison with ertapenem in patients with complicated intra-Habdominal infections [31]. The clinical success rates were 92.9% to 100% for those receiving eravacycline and 92.3% for those receiving ertapenem, respectively. The adverse event rates were 28.6% to 35.8% and 26.7%, respectively. The study however did not include infections due to A. baumannii.
P. aeruginosa is found in various environmental sources but also causes serious hospital-acquired infections. Like A. baumannii, it has the ability to develop resistance to multiple classes of antimicrobial agents which often includes carbapenems. The common types of infections include healthcare-associated pneumonia, bloodstream infection and urinary tract infection. P. aeruginosa is also a major pathogen that colonizes the airways of cystic fibrosis patients and causes repeated exacerbations with progressive development of multidrug resistance.
Studies have shown that, despite the risk for nephrotoxicity in patients receiving colistin, colistin may be useful for salvage therapy of P. aeruginosa infection when therapeutic choices are severely limited due to resistance to commonly used agents, including carbapenems. A recent survey in the U.S. indicated 98.8% susceptibility of P. aeruginosa to this agent [32]. In a retrospective cohort study where colistin use in 23 critically ill patients with MDR P. aeruginosa infection was examined, favorable clinical response was observed in 14 patients (61%), with only 3 patients experiencing relapse of infection. Bacteremia was the only significant factor associated with treatment failure (P = 0.02) [33]. In another retrospective analysis of 258 episodes of MDR gram-negative infections, which included 68 cases caused by P. aeruginosa, higher daily doses of colistin were independently associated with better survival regardless of the pathogen [34]. Finally, in a retrospective cohort study of 95 cancer patients with MDR P. aeruginosa infections who were treated with either colistin or another anti-pseudomonal agent, a significantly higher clinical response rate was observed among patients who received colistin (P = 0.026) [35]. Although randomized studies are lacking, these data suggest that colistin is likely a viable alternative for the therapy of P. aeruginosa infections when other anti-pseudomonal agents are inactive or treatment with them has failed.
Nebulized colistin has been used in patients with P. aeruginosa respiratory tract infection, particularly in the setting of cystic fibrosis. This mode of delivery is used to achieve high drug levels in the respiratory tract while minimizing systemic adverse effects. In one retrospective cohort study, nebulized colistin was used alone in the treatment of 21 patients with pneumonia due to MDR A. baumannii or P. aeruginosa [36]. The overall clinical and microbiological response rates were 57% and 86%, respectively, and nephrotoxicity was not observed. Another prospective observational study compared the efficacy of nebulized colistin for 14 days plus 3 days of intravenous aminoglycoside for ventilator-associated pneumonia due to MDR P. aeruginosa or A. baumannii and 14 days of intravenous β-lactam therapy plus 3 days of intravenous aminoglycoside or fluoroquinolone for the same condition due to susceptible P. aeruginosa or A. baumannii [37]. In this study, 67% of those treated with nebulized colistin were clinically cured at the end of treatment compared with 66% treated with intravenous β-lactams, suggesting that nebulized colistin with a short course of intravenous aminoglycoside may be as efficacious as β-lactam-based intravenous therapy. These data suggest that nebulized colistin may be a useful adjunct to intravenous therapy in the treatment of P. aeruginosa, but whether it can be used alone in the management of pneumonia remains to be seen.
MICs of fosfomycin for P. aeruginosa cluster around 64 µg/mL, and its role in the management of carbapenem-resistant P. aeruginosa infections has been explored. In a series of 8 hospitalized patients with a urine culture growing carbapenem-resistant P. aeruginosa who were treated with fosfomycin, the microbiological cure rate was 38% after receiving an average of 2.9 fosfomycin doses per treatment course [38]. In a cohort study examining the outcome of 30 patients with P. aeruginosa infection treated with fosfomycin, 86.7% had favorable clinical outcomes [39]. In another observational case series, the outcomes of critically ill patients treated with fosfomycin for infections due to XDR, carbapenemase-producing gram-negative bacteria were examined [40]. Among the 17 patients with P. aeruginosa infection, the clinical success rate was 83.3% and the microbiological success rate was 66.7% at day 14. Finally, a recent retrospective study compared the outcomes of patients with hospital-acquired and ventilator-associated bacterial pneumonia due to P. aeruginosa with intermediate resistance to carbapenems who were treated with doripenem and fosfomycin or colistin and fosfomycin [41]. No differences were detected between the groups regarding clinical cure rates (60% and 58%), microbiological eradication rates (72% and 63%) and all-cause mortality (40% and 42%). These studies, while informative, did not address the specific clinical efficacy of fosfomycin in P. aeruginosa infections since an overwhelming majority received additional agents. A prospective study where patients would receive standard therapy with or without fosfomycin would be required to answer this question.
Among the agents in late-stage clinical development, ceftolozane-tazobactam (formerly CXA-201) is undergoing phase 3 studies for complicated urinary tract infection and complicated intra-abdominal infection. Ceftolozane is a novel anti-pseudomonal cephalosporin. This combination is active against P. aeruginosa, including many isolates that are resistant to carbapenems [42]. Ceftazidime-avibactam is also in phase 3 studies for the same indications. Avibactam (formerly NXL104) is a β-lactamase inhibitor which restores the activity of ceftazidime against class A, C, and some class D β-lactamase-producing gram-negative bacteria [43]. Ceftazidime-avibactam is active against some P. aeruginosa isolates that are resistant to carbapenems. However, it is not active against isolates producing MBL.
The emergence and spread of carbapenem-resistant Enterobacteriaceae (CRE) is one of the most recent and worrisome developments in antimicrobial resistance. The problem is most acute with K. pneumoniae. In the U.S., 8 to 13% of K. pneumoniae causing hospital-acquired infections are now resistant to carbapenems [44]. While resistance to carbapenems may involve several combined mechanisms including modifications to outer membrane permeability and up-regulation of efflux systems, the recent surge in CRE is mostly mediated by production of carbapenemases. Among various carbapenemases, the most frequently encountered one is KPC, therefore clinical outcome data are most abundant for KPC-producing K. pneumoniae. Some data are also available on MBL-producing K. pneumoniae. Options for treating patients infected with carbapenem-resistant K. pneumoniae are limited as they are typically resistant to all β-lactam agents including carbapenems, but some strains remain susceptible to gentamicin, and most remain susceptible to tigecycline and colistin.
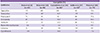
Agents consistently shown to have in vitro activity against KPC-producing K. pneumoniae include tigecycline (65-100% susceptible), colistin (73-93%), the aminoglycosides (gentamicin 30-63%, amikacin 6-77%) and tetracyclines (32-67%) (Table 2) [4, 45, 46, 47, 48].
Tigecycline has been used either alone or in combination with another agent in a number of patients. In a series of 12 patients infected with MBL-producing K. pneumoniae and treated with tigecycline alone at the standard dose, the overall clinical response rate was 75% [49]. In a review of 10 clinical studies investigating the outcomes of infections due to carbapenem-resistant, ESBL-producing or MDR Enterobacteriaceae, 69.3% of the 33 reported patients treated with tigecycline achieved resolution of infection [50]. Uniquely low serum concentrations of tigecycline warrant caution when using this agent alone to treat documented or potential bacteremic infections, as discussed in 1.3. Highlighting this concern, a case with persistent breakthrough bacteremia due to a K. pneumoniae isolate producing both MBL and ESBL while on tigecycline therapy has been reported [51]. Furthermore, it is not recommended for the treatment of urinary tract infections due to its low urine concentration [52].
In vitro susceptibility of carbapenemase-producing Enterobacteriaceae isolates to colistin ranges between 80 and 100% worldwide [53]. Colistin is often the only agent against carbapenemase-producing Enterobacteriaceae that achieves adequate serum levels exceeding the MICs [54].
In a case series including 17 seriously ill patients, 12 patients were treated successfully with colistin alone or in combination with either a carbapenem or an active aminoglycoside [55]. In an outbreak of KPC-producing K. pneumoniae, infection was successfully treated in 12 patients with an antimicrobial regimen containing colistin either as the only active agent, or with an aminoglycoside, tigecycline, or carbapenem [56]. In a prospective observational study of 67 patients with bloodstream infection caused by MBL-producing K. pneumoniae, 12 received appropriate combination therapy with two active drugs (carbapenem in combination with either colistin or an active aminoglycoside), and 37 received appropriate therapy with one active drug (14 carbapenem, 15 colistin, and 8 an active aminoglycoside) [57]. Mortality rates were 8.3% for those who received combination therapy with two active drugs and 27% for those who received therapy with one active drug, suggesting these combinations, almost half of which included colistin, may be efficacious. However, the outcome was not stratified for the use of colistin.
More recently, 127 patients with infections due to carbapenem-resistant K. pneumoniae in intensive care units across Greece were studied, which primarily included central venous catheter-related bacteraemia and ventilator-associated pneumonia [58]. Resistance to colistin, tigecycline, gentamicin and amikacin was detected in 20%, 33%, 21% and 64% of the isolates, respectively. Fourteen-day mortality rates were as follows: colistin monotherapy, 23.1%; aminoglycoside monotherapy, 22.7%; tigecycline monotherapy, 31.3%; tigecycline plus aminoglycosides, 18.1%; colistin plus aminoglycosides, 11.7%; colistin plus tigecycline, 44.4%. Mortality from inappropriate therapy (i.e., no active agent) was 35.0%. As such, colistin is a key agent in the treatment of carbapenem-resistant K. pneumoniae, with available clinical data generally favoring combination therapy over monotherapy in general (see also 3.8.).
The use of aminoglycosides for KPC-producing K. pneumoniae infections was reviewed earlier by Hirsch and Tam [59]. The aminoglycosides were used, alone or in combination, in a total of 8 patients with a 75% success rate. They had pneumonia, bacteremia or urinary tract infection and were treated with gentamicin or amikacin, alone or in combination with ciprofloxacin or tetracycline. However, the small number of patients and the heterogeneity of patient conditions and regimens precluded interpretation of the outcome data.
In a study of bloodstream infections due to CRE among patients with hematologic malignancies, gram-negative antimicrobial therapy was initiated in response to fever and/or sepsis on the day of blood culture collection in nearly all patients [47]. Only 2 patients received empirical therapy with an agent to which the CRE isolate was susceptible in vitro, with both clearing bacteremia. Three patients died before susceptibility data were available and never received an active agent. Among the remaining patients, 10 patients received one active agent, of which amikacin was most common, and 5 patients received two active agents. The 7-day, 14-day and in-hospital mortality rates were 39%, 53% and 56%, respectively. All 10 deaths were CRE-related [47]. The high mortality rates are likely due to the severity of the underlying illnesses in this population, but it is also possible that effective monotherapy with amikacin also contributed to the suboptimal clinical outcome. Overall, there are not sufficient data to support the use of aminoglycosides monotherapy for the therapy of carbapenem-resistant K. pneumoniae infections.
Carbapenems are rarely used alone for treatment of carbapenem-resistant K. pneumoniae infections, but before the carbapenem breakpoints were lowered by the Clinical and Laboratory Standards Institute (CLSI) in 2010, some cases that were reported as susceptible to a carbapenem despite production of KPC were treated with carbapenem monotherapy.
The aforementioned review by Hirsch and Tam complied reports on a total of 19 patients who were treated with a carbapenem alone or in combination with another agent due to the apparent susceptible testing results for carbapenems [59]. Strikingly, only 6 of 15 patients treated with carbapenem monotherapy had clinical success. While infections from isolates with carbapenem MICs of ≤ 4 µg/mL may be treated with high-dose carbapenem alone from pharmacokinetic and pharmacodynamics standpoints [60], the proportion of isolates falling within this range is small, and there is a concern for inadequate response as changes in the porin function may further raise the carbapenem MICs [61]. Therefore, the existing data do not support the use of carbapenem alone for invasive carbapenem-resistant K. pneumoniae infections, but it is increasingly suggested that it should be part of combination regimens (also see 3.8.).
Fosfomycin is active against over 90% of KPC-producing K. pneumoniae when using the susceptibility breakpoint of 64 µg/mL [62]. In a retrospective study of 13 hospitalized patients with urine culture growing KPC-producing K. pneumoniae and treated with oral fosfomycin, patients received an average of 2.9 fosfomycin doses per treatment course, resulting in a microbiological cure rate of 46% [38]. In another study, intravenous fosfomycin in combination with colistin, gentamicin, or piperacillin-tazobactam resulted in a promising clinical success rate (100%) in the treatment of serious infections caused by carbapenem-resistant K. pneumoniae [63]. In a recent prospective case series, the outcomes of critically ill patients treated with fosfomycin for infections due to XDR, carbapenemase-producing gram-negative bacteria were examined [40]. Among 23 patients with monomicrobial K. pneumoniae infection, clinical success rate was 56.5% and microbial success rate was 65.2%, but most of them appear to have received fosfomycin in combination with another agent (colistin for the most part). These data suggest that benefit of fosfomycin in the treatment of infections caused by carbapenem-resistant K. pneumoniae may exist, but only in the context of combination therapy. It should also be kept in mind that fosfomycin resistance may emerge during therapy, even when combination therapy is used [64].
Temocillin is a 6-α-methoxy derivative of ticarcillin that is approved for clinical use in several European countries. It is relatively resistant to hydrolysis by class A β-lactamases including KPC [65]. The MICs of temocillin for KPC-producing K. pneumoniae ranged between 16 and 64 µg/mL, and production of KPC in itself does not influence the temocillin MICs [66]. The susceptibility breakpoints available from the British Society for Antimicrobial Chemotherapy (BSAC) are 32 µg/mL for urinary tract infection and 8 µg/mL for systemic infections. Therefore, while specific clinical data are lacking, it may have a role in the treatment of urinary tract infection due to CRE. Although the currently licensed dosage is 2 g intravenously twice daily, 2 g thrice daily regimen is under evaluation and may justify a higher breakpoint for systemic infections [65].
Since the clinical efficacy of β-lactam agents is pharmacokinetically predicted by time above MIC, an extended infusion or continuous infusion is a potential strategy to overcome higher carbapenem MICs in carbapenemase-producing gram-negative bacteria. The advantage of this approach has been suggested in immunocompetent and neutropenic murine thigh models [67]. A case of successful treatment of KPC-producing K. pneumoniae bacteremia with high-dose continuous infusion meropenem has been reported [68]. However, no other clinical data addressing the utility this approach specifically for the treatment of CRE infections are available at this time.
Studies addressing the clinical outcome of CRE infections have been reviewed recently by Tzouvelekis et al. [69]. Among 889 patients included in this analysis, 441 received combination therapy and 346 received monotherapy. The mortality rates were 27.4% for combination therapy and 38.7% for monotherapy (P < 0.001). The mortality rates for monotherapy were 40.1% for carbapenem, 41.1% for tigecycline and 42.8% for colistin. The mortality rates for combination therapy were 30.7% for carbapenem-sparing combinations and 18.8% for carbapenem-containing combinations, suggesting that the inclusion of a carbapenem in the combination may provide survival benefit. A large proportion of patients in this analysis were derived from four studies conducted in the U.S., Greece and Italy addressing the clinical outcome of carbapenemase-producing K. pneumoniae bacteremia, most of which were due to KPC producing isolates. In the study from the U.S., the outcomes of a total of 41 patients with bacteremia were examined [70]. The overall 28-day crude mortality rate was 39.0% in this cohort. In the multivariate analysis, definitive therapy with a combination regimen was independently associated with survival (odds ratio [OR]: 0.07, P = 0.02). The 28-day mortality was 13.3% in the combination therapy group compared with 57.8% in the monotherapy group (P = 0.01). Despite in vitro susceptibility, patients who received monotherapy with colistin, polymyxin B or tigecycline had a high mortality of 66.7%. In the first study from Greece, a total of 53 patients with bacteremia were identified and included [71]. The overall mortality was 52.8%, and the infection-related mortality was 20%. Appropriate antimicrobial therapy was administered to 35 patients. All 20 patients who received combination therapy (colistin plus tigecycline or tigecycline with gentamicin) had favorable clinical outcome. In contrast, 7 of 15 patients given appropriate monotherapy (colistin, tigecycline, gentamicin) died (P = 0.001). The study from Italy examined the clinical outcomes of 125 patients with bloodstream infections caused by KPC-producing K. pneumoniae [72]. The overall 30-day mortality rate was 41.6%. A significantly higher mortality rate was observed among patients treated with monotherapy (54.3%) compared with those who received combined therapy (34.1%; P = 0.02). Mortality rates with the most frequent combinations were 30% for colistin plus tigecycline and 50% for tigecycline plus gentamicin. Notably, definitive therapy with a triple combination of tigecycline, colistin, and meropenem was associated with increased survival (OR: 0.11, 95% CI: 0.02 to 0.69, P = 0.01). Finally, the second study from Greece examined the outcome of 205 patients with bacteremia due to carbapenemase-producing K. pneumoniae, 163 of which produced KPC [73]. The rate of resistance to colistin was high at 25.4%. Of 175 patients who received active definitive therapy, 103 received combination therapy and 72 received monotherapy. The 28-day mortality rates were 27.2% and 44.4%, respectively (P = 0.003). Additionally, a low mortality rate (19.3%) was seen among patients given carbapenem-containing combinations, and lower carbapenem MICs were associated with lower mortality, as in the study from Italy.
These data support the use of combination therapy that includes colistin and/or tigecycline along with a carbapenem in the therapy of invasive infections due to carbapenem-resistant K. pneumoniae. On the other hand, patients may fare well regardless of therapy for non-invasive infections such as uncomplicated urinary tract infection. In a retrospective study examining the clinical outcome of 21 patients with urinary tract infection due to carbapenem-resistant K. pneumoniae, 90% of them had clinical success regardless of therapy given, and the overall 30-day mortality was low at 6% [70]. Therefore, it is important to stratify cases into invasive (i.e. high mortality) and non-invasive (low mortality) infections and consider therapeutic approaches accordingly.
There are several new agents with activity against CRE in late clinical development that merit mention. Avibactam is a non-β-lactam β-lactamase inhibitor that is active against known Ambler class A and C β-lactamases with activity against some Ambler class D enzymes as well [74]. In vitro, avibactam inhibits the activity of Ambler class A (including ESBL and KPC), class C (i.e. AmpC), and some class D (including OXA-48) enzymes. It is not active against MBLs (e.g. NDM, VIM, IMP) due to the absence of the active-site serine residue in these enzymes, and it does not inhibit OXA-type carbapenemases produced by A. baumannii [75, 76]. Of note, avibactam has a potent inhibitory activity against KPC that is substantially greater than that of clavulanate and tazobactam [74, 77]. Ceftazidime-avibactam is currently in phase 3 trials for the treatment of complicated intra-abdominal infections and complicated urinary tract infections. Once approved, it is expected to play a role in the empiric monotherapy of invasive infections suspected to be caused by resistant Enterobacteriaceae pathogens, and also potentially as definitive therapy of KPC-producing Enterobacteriaceae infection.
Plazomicin is a novel aminoglycoside that is designed to resist most clinically relevant aminoglycoside modifying enzymes and holds promise for the treatment of infections caused by CRE, including KPC-producing K. pneumoniae [78]. It is currently undergoing a phase 3 superiority trial targeting CRE bacteremia and pneumonia, where plazomicin-based regimens will be compared with colistin-based regimens. It is however not active against many of the NDM-producing isolates due to the co-production of 16S ribosomal RNA methyltransferase.
Carbapenem resistance in Escherichia coli does not occur naturally, and acquired resistance is rare in this species [79]. More recently, however, KPC-producing E. coli is increasingly reported in the literature. Clinical outcome data regarding carbapenem-resistant E. coli infection are extremely scarce to date. In one case series in the U.S., a total of 13 patients with infection due to KPC-producing E. coli were identified. Ten patients were deemed to have infection due to this organism, whereas 3 patients were found to be colonized only. They were treated with a variety of definitive antimicrobial therapy, which included carbapenems, cefepime, trimethoprim-sulfamethoxazole, ciprofloxacin, amikacin, tigecycline, and colistimethate, alone or in combination. Of those with infection, 6 were alive and 3 had died by 28 days after infection [80]. The study was not large enough to correlate specific regimens with clinical outcome. It is noteworthy that the carbapenem MICs of carbapenemase-producing E. coli strains are much lower than those of carbapenemase-producing K. pneumoniae strains, often falling in the susceptible range for imipenem, meropenem and doripenem [81, 82]. However, exposure to a carbapenem has been shown to result in elevated MICs in a pharmacodynamic model [83]. Therefore, it seems prudent to avoid the use of carbapenem alone for treatment carbapenem-resistant E. coli infection even when the isolate tests susceptible to a specific carbapenem. Fortunately, they remain relatively susceptible to non-β-lactam agents such as gentamicin, amikacin, minocycline and fosfomycin as well as tigecycline and colistin [82, 84].
Acquired carbapenem resistance is still uncommon among Enterobacter spp., thus clinical studies of carbapenem-resistant E. cloacae infection are limited in number. In a study of 6 patients infected or colonized with MBL-producing E. cloacae, 4 of 5 patients who had infection died in hospital, 3 of them before the susceptibility results became available [85]. In another series of 7 patients with carbapenem-resistant E. cloacae, 2 of which were produced MBL, 3 cases were considered to represent infection. Two of these 3 patients died by day 30 [86]. Finally, a series of 11 patients with KPC-producing Enterobacter spp., including 8 E. cloacae and 3 Enterobacter aerogenes, was recently published [87]. Six patients had infection, 2 with bacteremia, 2 with urinary tract infection, and 1 each with meningitis and peritonitis. Two of them did not survive the hospitalization, including one of the patients with bacteremia and the patient with meningitis. While they received various antimicrobial therapies, the outcome appeared to be associated with the severity of underlying illness. Interestingly, 2 patients with urinary tract infection had clinical success with amikacin and fosfomycin or trimethoprim-sulfamethoxazole, highlighting that that the type and severity of infection matters when considering clinical outcome.
S. maltophilia is a gram-negative, non-fermentative bacillus which is increasingly being recognized as a cause of hospital-acquired infections. It is inherently resistant to multiple classes of antibiotics including cephalosporins, carbapenems and aminoglycosides [88]. Attributable mortality due to invasive S. maltophilia infection has historically ranged around 30% [89, 90], but may increase to 60% among patients who acquire their infection while in the intensive care unit [91]. Trimethoprim-sulfamethoxazole (TMP-SMX) is considered the first-line therapy because of its excellent in vitro activity against the majority of isolates, whereas fluoroquinolones are an alternative option for treatment, if the pathogen is shown to be susceptible to them in vitro. Ticarcillin-clavulanate has also been proposed as an alternate therapy to TMP-SMX, but resistance rates to this agent can be significant depending on the local epidemiology. While in vitro synergy of various combinations of agents has been studied extensively [92], the majority of clinical data available on the therapy of S. maltophilia infection address monotherapy by an active agent.
With regards to clinical data, for 98 patients with S. maltophilia infections, mostly in the respiratory tract, who were treated with either TMP-SMX or a fluoroquinolone alone, the in-hospital mortality rates were 20% and 25% for those who received TMP-SXT and fluoroquinolone, respectively, and the microbiological cure rates were 65% and 62%, respectively [93]. At least two more retrospective studies evaluating the efficacy of levofloxacin and TMP-SMX in the treatment of S. maltophilia bacteremia reported comparable 30-day mortality rates [94, 95]. In a recent series of 45 patients, the efficacy of tigecycline treatment in nosocomial S. maltophilia infections was compared with TMP-SMX [96]. Pneumonia was the most common cause of infection (51.1%), followed by surgical site infection, and bacteremia. For therapy, 57.8% received TMP-SMX and 42.2% received tigecycline within 24 hours after the culture results. Clinical improvement was observed for 69.2% in the TMP-SMX group and 68.4% in the tigecycline group on day 14. The 30-day mortality rates were 30.8% and 21.1% in the TMP-SMX and tigecycline groups, respectively. This showed that tigecycline could also be considered an alternative treatment option against nosocomial S. maltophilia infection.
Carbapenem resistant gram-negative bacteria are spreading rapidly in the healthcare environments posing a substantial public health threat worldwide. They primarily affect the chronically or acutely ill populations, and infections due to these organisms are generally associated with high mortality. Despite the scope of the problem, there is a major gap in knowledge as to how these infections can be managed optimally, with most studies relying on small numbers of patients and retrospective study designs. However, there are encouraging signs. An increasing number of controlled randomized trials are being conducted and results released to address antimicrobial therapy, especially for infections due to K. pneumoniae and A. baumannii, where carbapenem resistance has become endemic in many locales. Nonetheless, high-quality evidence is still lacking in many scenarios encountered in clinical practice. It therefore remains crucial for clinicians to determine, for each case of carbapenem-resistant gram-negative bacteria, whether the patient is truly presenting with infection or merely colonized with the organism, and carefully consider the therapeutic approach based on the condition of the patient, antimicrobial susceptibility and available clinical data.
Figures and Tables
Acknowledgment
The effort of Y.D. was supported in part by research grants from the National Institutes of Health (R21AI107302 and R01AI104895).
References
1. Akova M, Daikos GL, Tzouvelekis L, Carmeli Y. Interventional strategies and current clinical experience with carbapenemase-producing Gram-negative bacteria. Clin Microbiol Infect. 2012; 18:439–448.

2. Queenan AM, Bush K. Carbapenemases: the versatile β-lactamases. Clin Microbiol Rev. 2007; 20:440.

3. Schwaber MJ, Carmeli Y. Carbapenem-resistant Enterobacteriaceae: a potential threat. JAMA. 2008; 300:2911–2913.
4. Bratu S, Mooty M, Nichani S, Landman D, Gullans C, Pettinato B, Karumudi U, Tolaney P, Quale J. Emergence of KPC-possessing Klebsiella pneumoniae in Brooklyn, New York: epidemiology and recommendations for detection. Antimicrob Agents Chemother. 2005; 49:3018–3020.

5. Kanj SS, Kanafani ZA. Current concepts in antimicrobial therapy against resistant gram-negative organisms: extended-spectrum β-lactamase-producing Enterobacteriaceae, carbapenem-resistant Enterobacteriaceae, and multidrug-resistant Pseudomonas aeruginosa. Mayo Clin Proc. 2011; 86:250–259.

6. Peleg AY, Seifert H, Paterson DL. Acinetobacter baumannii: emergence of a successful pathogen. Clin Microbiol Rev. 2008; 21:538–582.

7. Lemos EV, de la Hoz FP, Einarson TR, McGhan WF, Quevedo E, Castañeda C, Kawai K. Carbapenem resistance and mortality in patients with Acinetobacter baumannii infection: systematic review and meta-analysis. Clin Microbiol Infect. 2014; 20:416–423.

8. Queenan AM, Pillar CM, Deane J, Sahm DF, Lynch AS, Flamm RK, Peterson J, Davies TA. Multidrug resistance among Acinetobacter spp. in the USA and activity profile of key agents: results from CAPITAL Surveillance 2010. Diagn Microbiol Infect Dis. 2012; 73:267–270.

9. Garnacho-Montero J, Ortiz-Leyba C, Jiménez-Jiménez FJ, Barrero-Almodóvar AE, García-Garmendia JL, Bernabeu-WittelI M, Gallego-Lara SL, Madrazo-Osuna J. Treatment of multidrug-resistant Acinetobacter baumannii ventilator-associated pneumonia (VAP) with intravenous colistin: a comparison with imipenem-susceptible VAP. Clin Infect Dis. 2003; 36:1111–1118.

10. Oliveira MS, Prado GV, Costa SF, Grinbaum RS, Levin AS. Ampicillin/sulbactam compared with polymyxins for the treatment of infections caused by carbapenem-resistant Acinetobacter spp. J Antimicrob Chemother. 2008; 61:1369–1375.

11. Garonzik SM, Li J, Thamlikitkul V, Paterson DL, Shoham S, Jacob J, Silveira FP, Forrest A, Nation RL. Population pharmacokinetics of colistin methanesulfonate and formed colistin in critically ill patients from a multicenter study provide dosing suggestions for various categories of patients. Antimicrob Agents Chemother. 2011; 55:3284–3294.

12. Kuo SC, Lee YT, Yang SP, Chen CP, Chen TL, Hsieh SL, Siu LK, Fung CP. Eradication of multidrug-resistant Acinetobacter baumannii from the respiratory tract with inhaled colistin methanesulfonate: a matched case-control study. Clin Microbiol Infect. 2012; 18:870–876.

13. Rattanaumpawan P, Lorsutthitham J, Ungprasert P, Angkasekwinai N, Thamlikitkul V. Randomized controlled trial of nebulized colistimethate sodium as adjunctive therapy of ventilator-associated pneumonia caused by Gram-negative bacteria. J Antimicrob Chemother. 2010; 65:2645–2649.

14. Swenson JM, Killgore GE, Tenover FC. Antimicrobial susceptibility testing of Acinetobacter spp. by NCCLS broth microdilution and disk diffusion methods. J Clin Microbiol. 2004; 42:5102–5108.

15. Reddy T, Chopra T, Marchaim D, Pogue JM, Alangaden G, Salimnia H, Boikov D, Navon-Venezia S, Akins R, Selman P, Dhar S, Kaye KS. Trends in antimicrobial resistance of Acinetobacter baumannii isolates from a metropolitan Detroit health system. Antimicrob Agents Chemother. 2010; 54:2235–2238.

16. Betrosian AP, Frantzeskaki F, Xanthaki A, Douzinas EE. Efficacy and safety of high-dose ampicillin/sulbactam vs. colistin as monotherapy for the treatment of multidrug resistant Acinetobacter baumannii ventilator-associated pneumonia. J Infect. 2008; 56:432–436.

17. Muralidharan G, Micalizzi M, Speth J, Raible D, Troy S. Pharmacokinetics of tigecycline after single and multiple doses in healthy subjects. Antimicrob Agents Chemother. 2005; 49:220–229.

18. Kim NH, Hwang JH, Song KH, Choe PG, Kim ES, Park SW, Kim HB, Kim NJ, Park WB, Oh MD. Tigecycline in carbapenem-resistant Acinetobacter baumannii bacteraemia: susceptibility and clinical outcome. Scand J Infect Dis. 2013; 45:315–319.

19. Lee YT, Tsao SM, Hsueh PR. Clinical outcomes of tigecycline alone or in combination with other antimicrobial agents for the treatment of patients with healthcare-associated multidrug-resistant Acinetobacter baumannii infections. Eur J Clin Microbiol Infect Dis. 2013; 32:1211–1220.

20. Ramirez J, Dartois N, Gandjini H, Yan JL, Korth-Bradley J, McGovern PC. Randomized phase 2 trial to evaluate the clinical efficacy of two high-dosage tigecycline regimens versus imipenem-cilastatin for treatment of hospital-acquired pneumonia. Antimicrob Agents Chemother. 2013; 57:1756–1762.

21. Denys GA, Callister SM, Dowzicky MJ. Antimicrobial susceptibility among gram-negative isolates collected in the USA between 2005 and 2011 as part of the Tigecycline Evaluation and Surveillance Trial (T.E.S.T.). Ann Clin Microbiol Antimicrob. 2013; 12:24.

22. Griffith ME, Yun HC, Horvath LL, Murray CK. Minocycline therapy for traumatic wound infections caused by the multidrug-resistant Acinetobacter baumannii-Acinetobacter calcoaceticus complex. Infect Dis Clin Pract. 2008; 16:16–19.

23. Wood GC, Hanes SD, Boucher BA, Croce MA, Fabian TC. Tetracyclines for treating multidrug-resistant Acinetobacter baumannii ventilator-associated pneumonia. Intensive Care Med. 2003; 29:2072–2076.

24. Aydemir H, Akduman D, Piskin N, Comert F, Horuz E, Terzi A, Kokturk F, Ornek T, Celebi G. Colistin vs. the combination of colistin and rifampicin for the treatment of carbapenem-resistant Acinetobacter baumannii ventilator-associated pneumonia. Epidemiol Infect. 2013; 141:1214–1222.

25. Durante-Mangoni E, Signoriello G, Andini R, Mattei A, De Cristoforo M, Murino P, Bassetti M, Malacarne P, Petrosillo N, Galdieri N, Mocavero P, Corcione A, Viscoli C, Zarrilli R, Gallo C, Utili R. Colistin and rifampicin compared with colistin alone for the treatment of serious infections due to extensively drug-resistant Acinetobacter baumannii: a multicenter, randomized clinical trial. Clin Infect Dis. 2013; 57:349–358.

26. Santimaleeworagun W, Wongpoowarak P, Chayakul P, Pattharachayakul S, Tansakul P, Garey KW. In vitro activity of colistin or sulbactam in combination with fosfomycin or imipenem against clinical isolates of carbapenem-resistant Acinetobacter baumannii producing OXA-23 carbapenemases. Southeast Asian J Trop Med Public Health. 2011; 42:890–900.
27. Sirijatuphat R, Thamlikitkul V. Colistin versus colistin plus fosfomycin for treatment of carbapenem-resistant Acinetobacter baumannii infections : A preliminary study. Antimicrob Agents Chemother. 2014; 58:5598–5601.

28. Batirel A, Balkan II, Karabay O, Agalar C, Akalin S, Alici O, Alp E, Altay FA, Altin N, Arslan F, Aslan T, Bekiroglu N, Cesur S, Celik AD, Dogan M, Durdu B, Duygu F, Engin A, Engin DO, Gonen I, Guclu E, Guven T, Hatipoglu CA, Hosoglu S, Karahocagil MK, Kilic AU, Ormen B, Ozdemir D, Ozer S, Oztoprak N, Sezak N, Turhan V, Turker N, Yilmaz H. Comparison of colistin-carbapenem, colistin-sulbactam, and colistin plus other antibacterial agents for the treatment of extremely drug-resistant Acinetobacter baumannii bloodstream infections. Eur J Clin Microbiol Infect Dis. 2014; 33:1311–1322.

29. Shields RK, Clancy CJ, Gillis LM, Kwak EJ, Silveira FP, Massih RC, Eschenauer GA, Potoski BA, Nguyen MH. Epidemiology, clinical characteristics and outcomes of extensively drug-resistant Acinetobacter baumannii infections among solid organ transplant recipients. PLoS One. 2012; 7:e52349.
30. Sutcliffe JA, O'Brien W, Fyfe C, Grossman TH. Antibacterial activity of eravacycline (TP-434), a novel fluorocycline, against hospital and community pathogens. Antimicrob Agents Chemother. 2013; 57:5548–5558.

31. Solomkin JS, Ramesh MK, Cesnauskas G, Novikovs N, Stefanova P, Sutcliffe JA, Walpole SM, Horn PT. Phase 2, randomized, double-blind study of the efficacy and safety of two dose regimens of eravacycline versus ertapenem for adult community-acquired complicated intra-abdominal infections. Antimicrob Agents Chemother. 2014; 58:1847–1854.

32. Morrow BJ, Pillar CM, Deane J, Sahm DF, Lynch AS, Flamm RK, Peterson J, Davies TA. Activities of carbapenem and comparator agents against contemporary US Pseudomonas aeruginosa isolates from the CAPITAL surveillance program. Diagn Microbiol Infect Dis. 2013; 75:412–416.

33. Linden PK, Kusne S, Coley K, Fontes P, Kramer DJ, Paterson D. Use of parenteral colistin for the treatment of serious infection due to antimicrobial-resistant Pseudomonas aeruginosa. Clin Infect Dis. 2003; 37:e154–e160.
34. Falagas ME, Rafailidis PI, Ioannidou E, Alexiou VG, Matthaiou DK, Karageorgopoulos DE, Kapaskelis A, Nikita D, Michalopoulos A. Colistin therapy for microbiologically documented multidrug-resistant Gram-negative bacterial infections: a retrospective cohort study of 258 patients. Int J Antimicrob Agents. 2010; 35:194–199.

35. Hachem RY, Chemaly RF, Ahmar CA, Jiang Y, Boktour MR, Rjaili GA, Bodey GP, Raad II. Colistin is effective in treatment of infections caused by multidrug-resistant Pseudomonas aeruginosa in cancer patients. Antimicrob Agents Chemother. 2007; 51:1905–1911.

36. Kwa AL, Loh C, Low JG, Kurup A, Tam VH. Nebulized colistin in the treatment of pneumonia due to multidrug-resistant Acinetobacter baumannii and Pseudomonas aeruginosa. Clin Infect Dis. 2005; 41:754–757.

37. Lu Q, Luo R, Bodin L, Yang J, Zahr N, Aubry A, Golmard JL, Rouby JJ. Nebulized Antibiotics Study Group. Efficacy of high-dose nebulized colistin in ventilator-associated pneumonia caused by multidrug-resistant Pseudomonas aeruginosa and Acinetobacter baumannii. Anesthesiology. 2012; 117:1335–1347.

38. Neuner EA, Sekeres J, Hall GS, van Duin D. Experience with fosfomycin for treatment of urinary tract infections due to multidrug-resistant organisms. Antimicrob Agents Chemother. 2012; 56:5744–5748.

39. Dinh A, Salomon J, Bru JP, Bernard L. Fosfomycin: efficacy against infections caused by multidrug-resistant bacteria. Scand J Infect Dis. 2012; 44:182–189.

40. Pontikis K, Karaiskos I, Bastani S, Dimopoulos G, Kalogirou M, Katsiari M, Oikonomou A, Poulakou G, Roilides E, Giamarellou H. Outcomes of critically ill intensive care unit patients treated with fosfomycin for infections due to pandrug-resistant and extensively drug-resistant carbapenemase-producing Gram-negative bacteria. Int J Antimicrob Agents. 2014; 43:52–59.

41. Apisarnthanarak A, Mundy LM. Carbapenem-resistant Pseudomonas aeruginosa pneumonia with intermediate minimum inhibitory concentrations to doripenem: combination therapy with high-dose, 4-h infusion of doripenem plus fosfomycin versus intravenous colistin plus fosfomycin. Int J Antimicrob Agents. 2012; 39:271–272.

42. Takeda S, Nakai T, Wakai Y, Ikeda F, Hatano K. In vitro and in vivo activities of a new cephalosporin, FR264205, against Pseudomonas aeruginosa. Antimicrob Agents Chemother. 2007; 51:826–830.

43. Mushtaq S, Warner M, Livermore DM. In vitro activity of ceftazidime+NXL104 against Pseudomonas aeruginosa and other non-fermenters. J Antimicrob Chemother. 2010; 65:2376–2381.

44. Sievert DM, Ricks P, Edwards JR, Schneider A, Patel J, Srinivasan A, Kallen A, Limbago B, Fridkin S. National Healthcare Safety Network (NHSN) Team and Participating NHSN Facilities. Antimicrobial-resistant pathogens associated with healthcare-associated infections: summary of data reported to the National Healthcare Safety Network at the Centers for Disease Control and Prevention, 2009-2010. Infect Control Hosp Epidemiol. 2013; 34:1–14.

45. Bratu S, Tolaney P, Karumudi U, Quale J, Mooty M, Nichani S, Landman D. Carbapenemase-producing Klebsiella pneumoniae in Brooklyn, NY: molecular epidemiology and in vitro activity of polymyxin B and other agents. J Antimicrob Chemother. 2005; 56:128–132.

46. Castanheira M, Sader HS, Deshpande LM, Fritsche TR, Jones RN. Antimicrobial activities of tigecycline and other broad-spectrum antimicrobials tested against serine carbapenemase-and metallo-β-lactamase-producing Enterobacteriaceae: report from the SENTRY Antimicrobial Surveillance Program. Antimicrob Agents Chemother. 2008; 52:570–573.

47. Satlin MJ, Calfee DP, Chen L, Fauntleroy KA, Wilson SJ, Jenkins SG, Feldman EJ, Roboz GJ, Shore TB, Helfgott DC, Soave R, Kreiswirth BN, Walsh TJ. Emergence of carbapenem-resistant Enterobacteriaceae as causes of bloodstream infections in patients with hematologic malignancies. Leuk Lymphoma. 2013; 54:799–806.

48. Pena I, Picazo JJ, Rodríguez-Avial C, Rodríguez-Avial I. Carbapenemase-producing Enterobacteriaceae in a tertiary hospital in Madrid, Spain: high percentage of colistin resistance among VIM-1-producing Klebsiella pneumoniae ST11 isolates. Int J Antimicrob Agents. 2014; 43:460–464.

49. Poulakou G, Kontopidou FV, Paramythiotou E, Kompoti M, Katsiari M, Mainas E, Nicolaou C, Yphantis D, Antoniadou A, Trikka-Graphakos E, Roussou Z, Clouva P, Maguina N, Kanellakopoulou K, Armaganidis A, Giamarellou H. Tigecycline in the treatment of infections from multi-drug resistant gram-negative pathogens. J Infect. 2009; 58:273–284.

50. Kelesidis T, Karageorgopoulos DE, Kelesidis I, Falagas ME. Tigecycline for the treatment of multidrug-resistant Enterobacteriaceae: a systematic review of the evidence from microbiological and clinical studies. J Antimicrob Chemother. 2008; 62:895–904.

51. Cobo J, Morosini MI, Pintado V, Tato M, Samaranch N, Baquero F, Cantón R. Use of tigecycline for the treatment of prolonged bacteremia due to a multiresistant VIM-1 and SHV-12 β-lactamase-producing Klebsiella pneumoniae epidemic clone. Diagn Microbiol Infect Dis. 2008; 60:319–322.

52. Nordmann P, Cuzon G, Naas T. The real threat of Klebsiella pneumoniae carbapenemase-producing bacteria. Lancet Infect Dis. 2009; 9:228–236.

53. Bogdanovich T, Adams-Haduch JM, Tian GB, Nguyen MH, Kwak EJ, Muto CA, Doi Y. Colistin-resistant, Klebsiella pneumoniae carbapenemase (KPC)-producing Klebsiella pneumoniae belonging to the international epidemic clone ST258. Clin Infect Dis. 2011; 53:373–376.

54. Arnold RS, Thom KA, Sharma S, Phillips M, Johnson JK, Morgan DJ. Emergence of Klebsiella pneumoniae carbapenemase-producing bacteria. South Med J. 2011; 104:40–45.
55. Souli M, Kontopidou FV, Papadomichelakis E, Galani I, Armaganidis A, Giamarellou H. Clinical experience of serious infections caused by Enterobacteriaceae producing VIM-1 metallo-β-lactamase in a Greek University Hospital. Clin Infect Dis. 2008; 46:847–854.

56. Souli M, Galani I, Antoniadou A, Papadomichelakis E, Poulakou G, Panagea T, Vourli S, Zerva L, Armaganidis A, Kanellakopoulou K, Giamarellou H. An outbreak of infection due to β-lactamase Klebsiella pneumoniae carbapenemase 2-producing K. pneumoniae in a Greek university hospital: molecular characterization, epidemiology, and outcomes. Clin Infect Dis. 2010; 50:364–373.

57. Daikos GL, Petrikkos P, Psichogiou M, Kosmidis C, Vryonis E, Skoutelis A, Georgousi K, Tzouvelekis LS, Tassios PT, Bamia C, Petrikkos G. Prospective observational study of the impact of VIM-1 metallo-β-lactamase on the outcome of patients with Klebsiella pneumoniae bloodstream infections. Antimicrob Agents Chemother. 2009; 53:1868–1873.

58. Kontopidou F, Giamarellou H, Katerelos P, Maragos A, Kioumis I, Trikka-Graphakos E, Valakis C, Maltezou HC. Group for the Study of KPC-producing Klebsiella pneumoniae infections in intensive care units. Infections caused by carbapenem-resistant Klebsiella pneumoniae among patients in intensive care units in Greece: a multi-centre study on clinical outcome and therapeutic options. Clin Microbiol Infect. 2014; 20:O117–O123.
59. Hirsch EB, Tam VH. Detection and treatment options for Klebsiella pneumoniae carbapenemases (KPCs): an emerging cause of multidrug-resistant infection. J Antimicrob Chemother. 2010; 65:1119–1125.

60. Daikos GL, Markogiannakis A. Carbapenemase-producing Klebsiella pneumoniae: (when) might we still consider treating with carbapenems? Clin Microbiol Infect. 2011; 17:1135–1141.

61. Clancy CJ, Chen L, Shields RK, Zhao Y, Cheng S, Chavda KD, Hao B, Hong JH, Doi Y, Kwak EJ, Silveira FP, Abdel-Massih R, Bogdanovich T, Humar A, Perlin DS, Kreiswirth BN, Hong Nguyen M. Epidemiology and molecular characterization of bacteremia due to carbapenem-resistant Klebsiella pneumoniae in transplant recipients. Am J Transplant. 2013; 13:2619–2633.

62. Endimiani A, Patel G, Hujer KM, Swaminathan M, Perez F, Rice LB, Jacobs MR, Bonomo RA. In vitro activity of fosfomycin against blaKPC-containing Klebsiella pneumoniae isolates, including those nonsusceptible to tigecycline and/or colistin. Antimicrob Agents Chemother. 2010; 54:526–529.

63. Michalopoulos A, Virtzili S, Rafailidis P, Chalevelakis G, Damala M, Falagas ME. Intravenous fosfomycin for the treatment of nosocomial infections caused by carbapenem-resistant Klebsiella pneumoniae in critically ill patients: a prospective evaluation. Clin Microbiol Infect. 2010; 16:184–186.

64. Karageorgopoulos DE, Miriagou V, Tzouvelekis LS, Spyridopoulou K, Daikos GL. Emergence of resistance to fosfomycin used as adjunct therapy in KPC Klebsiella pneumoniae bacteraemia: report of three cases. J Antimicrob Chemother. 2012; 67:2777–2779.

66. Adams-Haduch JM, Potoski BA, Sidjabat HE, Paterson DL, Doi Y. Activity of temocillin against KPC-producing Klebsiella pneumoniae and Escherichia coli. Antimicrob Agents Chemother. 2009; 53:2700–2701.

67. Bulik CC, Nicolau DP. In vivo efficacy of simulated human dosing regimens of prolonged-infusion doripenem against carbapenemase-producing Klebsiella pneumoniae. Antimicrob Agents Chemother. 2010; 54:4112–4115.

68. Ho VP, Jenkins SG, Afaneh CI, Turbendian HK, Nicolau DP, Barie PS. Use of meropenem by continuous infusion to treat a patient with a blaKPC-2-positive Klebsiella pneumoniae blood stream infection. Surg Infect (Larchmt). 2011; 12:325–327.

69. Tzouvelekis LS, Markogiannakis A, Piperaki E, Souli M, Daikos GL. Treating infections caused by carbapenemase-producing Enterobacteriaceae. Clin Microbiol Infect. 2014; [Epub ahead of print].
70. Qureshi ZA, Paterson DL, Potoski BA, Kilayko MC, Sandovsky G, Sordillo E, Polsky B, Adams-Haduch JM, Doi Y. Treatment outcome of bacteremia due to KPC-producing Klebsiella pneumoniae: superiority of combination antimicrobial regimens. Antimicrob Agents Chemother. 2012; 56:2108–2113.

71. Zarkotou O, Pournaras S, Tselioti P, Dragoumanos V, Pitiriga V, Ranellou K, Prekates A, Themeli-Digalaki K, Tsakris A. Predictors of mortality in patients with bloodstream infections caused by KPC-producing Klebsiella pneumoniae and impact of appropriate antimicrobial treatment. Clin Microbiol Infect. 2011; 17:1798–1803.

72. Tumbarello M, Viale P, Viscoli C, Trecarichi EM, Tumietto F, Marchese A, Spanu T, Ambretti S, Ginocchio F, Cristini F, Losito AR, Tedeschi S, Cauda R, Bassetti M. Predictors of mortality in bloodstream infections caused by Klebsiella pneumoniae carbapenemase-producing K. pneumoniae: importance of combination therapy. Clin Infect Dis. 2012; 55:943–950.

73. Daikos GL, Tsaousi S, Tzouvelekis LS, Anyfantis I, Psichogiou M, Argyropoulou A, Stefanou I, Sypsa V, Miriagou V, Nepka M, Georgiadou S, Markogiannakis A, Goukos D, Skoutelis A. Carbapenemase-producing Klebsiella pneumoniae bloodstream infections: lowering mortality by antibiotic combination schemes and the role of carbapenems. Antimicrob Agents Chemother. 2014; 58:2322–2328.

74. Lagacé-Wiens P, Walkty A, Karlowsky JA. Ceftazidime-avibactam: an evidence-based review of its pharmacology and potential use in the treatment of Gram-negative bacterial infections. Core Evid. 2014; 9:13–25.
75. Ehmann DE, Jahic H, Ross PL, Gu RF, Hu J, Durand-Réville TF, Lahiri S, Thresher J, Livchak S, Gao N, Palmer T, Walkup GK, Fisher SL. Kinetics of avibactam inhibition against Class A, C, and D β-lactamases. J Biol Chem. 2013; 288:27960–27971.

76. Mushtaq S, Warner M, Williams G, Critchley I, Livermore DM. Activity of chequerboard combinations of ceftaroline and NXL104 versus β-lactamase-producing Enterobacteriaceae. J Antimicrob Chemother. 2010; 65:1428–1432.

77. Stachyra T, Levasseur P, Péchereau MC, Girard AM, Claudon M, Miossec C, Black MT. In vitro activity of the β-lactamase inhibitor NXL104 against KPC-2 carbapenemase and Enterobacteriaceae expressing KPC carbapenemases. J Antimicrob Chemother. 2009; 64:326–329.

78. Endimiani A, Hujer KM, Hujer AM, Armstrong ES, Choudhary Y, Aggen JB, Bonomo RA. ACHN-490, a neoglycoside with potent in vitro activity against multidrug-resistant Klebsiella pneumoniae isolates. Antimicrob Agents Chemother. 2009; 53:4504–4507.

79. Nordmann P, Poirel L. Emerging carbapenemases in Gram-negative aerobes. Clin Microbiol Infect. 2002; 8:321–331.

80. Kim YA, Qureshi ZA, Adams-Haduch JM, Park YS, Shutt KA, Doi Y. Features of infections due to Klebsiella pneumoniae carbapenemase-producing Escherichia coli: emergence of sequence type 131. Clin Infect Dis. 2012; 55:224–231.

81. Landman D, Urban C, Bäcker M, Kelly P, Shah N, Babu E, Bratu S, Quale J. Susceptibility profiles, molecular epidemiology, and detection of KPC-producing Escherichia coli isolates from the New York City vicinity. J Clin Microbiol. 2010; 48:4604–4607.

82. O'Hara JA, Hu F, Ahn C, Nelson J, Rivera JI, Pasculle AW, Doi Y. Molecular epidemiology of KPC-producing Escherichia coli: Occurrence of ST131-fimH30 subclone harboring pKpQIL-like IncFIIk plasmid. Antimicrob Agents Chemother. 2014; 58:4234–4237.
83. Zhanel GG, Denisuik A, Vashisht S, Yachison C, Adam HJ, Hoban DJ. Pharmacodynamic activity of ertapenem versus genotypically characterized extended-spectrum β-lactamase (ESBL)-, KPC- or NDM-producing Escherichia coli with reduced susceptibility or resistance to ertapenem using an in vitro model. J Antimicrob Chemother. 2014; 69:2448–2452.

84. Kaase M, Szabados F, Anders A, Gatermann SG. Fosfomycin susceptibility in carbapenem-resistant Enterobacteriaceae from Germany. J Clin Microbiol. 2014; 52:1893–1897.

85. Novak A, Goic-Barisic I, Tambic Andrasevic A, Butic I, Radic M, Jelic M, Rubic Z, Tonkic M. Monoclonal outbreak of VIM-1-carbapenemase-producing Enterobacter cloacae in intensive care unit, University Hospital Centre Split, Croatia. Microb Drug Resist. 2014; [Epub ahead of print].
86. Lee Y, Choi H, Yum JH, Kang G, Bae IK, Jeong SH, Lee K. Molecular mechanisms of carbapenem resistance in Enterobacter cloacae clinical isolates from Korea and clinical outcome. Ann Clin Lab Sci. 2012; 42:281–286.
87. Ahn C, Syed A, Hu F, O'Hara JA, Rivera JI, Doi Y. Microbiological features of KPC-producing Enterobacter isolates identified in a U.S. hospital system. Diagn Microbiol Infect Dis. 2014; 80:154–158.

88. Nicodemo AC, Paez JI. Antimicrobial therapy for Stenotrophomonas maltophilia infections. Eur J Clin Microbiol Infect Dis. 2007; 26:229–237.

89. Lai CH, Chi CY, Chen HP, Chen TL, Lai CJ, Fung CP, Yu KW, Wong WW, Liu CY. Clinical characteristics and prognostic factors of patients with Stenotrophomonas maltophilia bacteremia. J Microbiol Immunol Infect. 2004; 37:350–358.
90. Senol E, DesJardin J, Stark PC, Barefoot L, Snydman DR. Attributable mortality of Stenotrophomonas maltophilia bacteremia. Clin Infect Dis. 2002; 34:1653–1656.

91. Nseir S, Di Pompeo C, Brisson H, Dewavrin F, Tissier S, Diarra M, Boulo M, Durocher A. Intensive care unit-acquired Stenotrophomonas maltophilia: incidence, risk factors, and outcome. Crit Care. 2006; 10:R143.
92. Brooke JS. Stenotrophomonas maltophilia: an emerging global opportunistic pathogen. Clin Microbiol Rev. 2012; 25:2–41.

93. Wang YL, Scipione MR, Dubrovskaya Y, Papadopoulos J. Monotherapy with fluoroquinolone or trimethoprim-sulfamethoxazole for treatment of Stenotrophomonas maltophilia infections. Antimicrob Agents Chemother. 2014; 58:176–182.

94. Cho SY, Kang CI, Kim J, Ha YE, Chung DR, Lee NY, Peck KR, Song JH. Can levofloxacin be a useful alternative to trimethoprim-sulfamethoxazole for treating Stenotrophomonas maltophilia bacteremia? Antimicrob Agents Chemother. 2014; 58:581–583.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download