Abstract
Background
Even after pneumococcal vaccination introduction, Streptococcus pneumoniae (pneumoccocus) is still an important cause of respiratory and invasive severe infection. Pneumococcus is resided in nasal mucosa and local or systemic infection begins with the nasal mucosa damage. We studied the indirect effect of pneumococcal conjugate vaccine (PCV) on pneumococcal nasopharyngeal carriage rates, serotypes and antimicrobial susceptibility between vaccinate and non-vaccinated children.
Materials and Methods
From January 2010 to October 2010, 379 healthy children under 5 years old from three university hospitals were recruited. Fully vaccinated children over 3 time doses of PCV and children with no vaccination history of PCV were enrolled, and nasopharyngeal aspirations were obtained from these children. Serotypes using multibead serotyping assay with multiplex PCR and antimicrobial susceptibility was analyzed. Antimicrobial susceptibilities were determined by the CLIS guideline.
Results
Two hundred seventy six children were received pneumococcal vaccination while 103 were not. 137 pneumococci were isolated from nasopharyngeal aspiration specimens. Nasal carriage rate was significantly low in vaccinated group (P-value; 0.001). Nasopharyngeal carriage rate was 28.6% (79/276) in vaccinate group and 56.3% (58/103) in non-vaccinated group. Among those vaccinated group, 13.0% (36/276) of the serotypes were vaccine or vaccine related type with the most common type 19F. In contrast, 31.1% (32/103) of the serotypes in non vaccinated group were vaccine or vaccine related type with the most common type 6A. The resistant rate of penicillin was 90.5%. For antimicrobial susceptibility, amoxicillin and amoxicillin/clavulanate showed high susceptibility (73.0%), but 19F and 19A serotypes were all resistant against amoxicillin.
Conclusions
High nasopharyngeal carriage rate in non vaccinated group corresponded to the result of past study. However, 19F and 19A still came up as problematic serotypes with a high carriage rate and antimicrobial resistance in both vaccinated and non vaccinated groups. Also, this study showed that the resistance rate of primary oral antimicrobial agents was increased in compared to past. For solving these problems, the selective antimicrobial use with establishment of high dose amoxicillin/clavulanate regimen and active PCV immunization should be needed. Furthermore, pneumococcal carriage and serotype study concerning with antimicrobial susceptibility should be conducted in the future in 10 or 13-valent PCV received children.
Streptococcus pneumoniae is the most common causative agent for acute respiratory infections or central nervous system infections such as pneumonia, otitis media, and sinusitis and severe invasive infections such as sepsis, meningitis in children less than 5 years of age [1-4]. The prevalence of antimicrobial resistant Streptococcus pneumoniae is increasing all over the world, so it is a serious problem clinically [5-12]. Especially, this bacterium has characteristic polymorphisms, so there are limits to controlling infection through antimicrobial agents; therefore recently, there have been attempts to basically prevent infection and control tolerance through vaccinations [13]. Additionally, this bacterium clinically resides in the nasal cavity of young infants, and local or systemic infection is caused when nasal damage occurs. Thus, basic epidemiological studies should be conducted regionally to examine the carriage rate and serotype of this bacteria residing in the nasal cavity of young children, and research verifying the efficacy of oral antimicrobial agents for Streptococcus pneumoniae separated from the nasal cavity should also be conducted. Recently in Korea, a pneumococcal conjugate vaccine has been introduced since 2003, and this vaccine is given while children are still infants to fundamentally prevent local and severe infections caused by Streptococcus pneumoniae [14]. According to some studies, there are domestic research results showing the reduced antimicrobial tolerance of residing Streptococcus pneumoniae in vaccinated cases compared to non-vaccinated cases [14]. However in vaccinated cases, there are results where Streptococcus pneumoniae reside as serotypes, which are not included in the vaccine, and problems of new serotypes with high tolerance have been posed; thus, clinical epidemiological research such as those above should be continuously conducted in young children [15-18]. Through Streptococcus pneumoniae serotypes isolated through such studies and antimicrobial sensitivity results, information should be continuously provided to primary care physicians to help them choose the most effective oral antimicrobials [19-21]. In addition, Korea has the highest tolerance rate of penicillin for this bacterium in the world, so this kind of epidemiological study is necessary.
In this aspect, the authors examined the nasal cavity carriage rate and serotype distribution of Streptococcus pneumoniae in relation to the pneumococcal conjugate vaccine vaccination rate for Streptococcus pneumoniae isolated from the nasal cavity of healthy Korean children under the age of 5 years. At the same time, research on the sensitivity of oral antimicrobials commonly used as primary treatment in Korea was conducted to indirectly evaluate the effectiveness of the pneumococcal conjugate vaccine, and to evaluate the choice of the primary antimicrobial agent being effective against acute respiratory infection by Streptococcus pneumoniae.
The research was conducted on 379 healthy children under the age of 5 who visited the pediatric clinic of Catholic University of Korea Seoul St. Mary's Hospital, Jeju National University Hospital, and Ewha Womans University Mokdong Hospital from January to October of 2010, or children who attended kindergarten in the area near the research institute who had not been exposed to antibiotics for 2 weeks prior to their visit. The demographic data and vaccination history for the pneumococcal conjugate vaccine were taken for all children participating in the study. Those with a vaccination history for pneumococcal conjugate vaccine (PCV) was defined as receiving the vaccine 3 or more times. All received PCV 7.
Nasopharyngeal secretions were collected using a nasopharyngeal mucus extractor from the above mentioned 379 healthy children under 5 years of age, and as a result, 137 Streptococcus pneumoniae isolates were cultivated. These strains were sent for serotype identification to the Center for Vaccine Evaluation and Study Medical Research Institute at Ewha Womans University, which is a Streptococcus pneumoniae serotype test accredited institution in the Asia-Pacific area. The serotypes of the isolated Streptococcus pneumoniae were categorized by the Quellung response using the antiserum antibody.
Microplates were made with Mueller-Hinton broth (MHB, BBL, Cat. No. 43118, USA) with 5% lysed horse blood, and the identified Streptococcus pneumoniae were stored in a freezer at -70℃ as glycerol stocks until use. The MIC of the oral antibiotics such as penicillin, amoxicillin, amoxicillin/clavulanate, cefaclor, cefdinir, and clarithromycin were measured with the broth microdilution method according to the 2010 standards of Clinical and Laboratory Standards Institute (CLSI). The non-meningitis standard was applied to penicillin [22]. The MIC50, MIC90 and ratio of sensitive strain for each antibiotic was investigated, and S. pneumoniae ATCC 49619 was used as the standard strain.
A comparison of the nasal carriage rate and serotypes and antimicrobial resistance in the vaccinated group and non-vaccinated group was conducted with Fisher's exact test or Chi-square test using SPSS version 11.5 software package (Chicago, IL, USA), and the results were considered to be statistically significant when the P-value was less than 0.05.
Among 379 subjects, 188 were male children. From the 276 subjects who had a vaccination history for receiving the pneumococcal conjugate vaccine and the 103 subjects with no history of vaccination, 137 strains of S. pneumoniae were isolated from within the nasal cavity. All subjects with a vaccination history were verified to be vaccinated with the pneumococcal conjugate vaccine 7 (vaccine serotype; 4, 6B, 9V, 14, 18C, 19F, 23F).
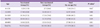
The nasopharyngeal pneumococcal carriage rate in the PCV vaccinated group was 28.6%, while it was 56.3% in the non-vaccinated group; thus, the carriage rate was statistically significantly higher in the non-vaccinated group. Additionally, the carriage rate of S. pneumoniae according to age was the highest in the 24-35 month group and was the lowest in the under 12 month group. Comparing the carriage rate according to age between the vaccinated group and non-vaccinated group, the non-vaccinated group had a significantly higher carriage rate for the 12-23, 24-35, and 48-60 month groups (Table 1).
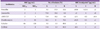
All subjects were vaccinated with PCV (vaccine serotype; 4, 6B, 9V, 14, 18C, 19F, 23F). The PCV 10 serotype includes 1, 4, 5, 6B, 7F, 9V, 14, 18C, 19F, and 23F and the PCV 13 includes 1, 3, 4, 5, 6A, 6B, 7F, 9V, 14, 18C, 19A, 19F, and 23F. After stopping the 7 vaccine, the 10 and 13 vaccines are currently distributed in Korea. In the vaccinated group, the serotypes included in the vaccine were isolated in order of highest isolation rate 19F, 23F, 19A, 6B, and 6A. From the vaccine related serotypes, 6D was the most highly isolated one showing approximately a 13% of vaccine serotype and related serotype carriage rate. In the non-vaccinated group, the vaccine serotypes were isolated in order of 6A, 23F, 19F, 6B, 3, and 19A, there was a difference with the vaccinated group. However, 6D was also the most highly isolated serotype in the non-vaccinated group as a vaccine related serotype. Approximately a 31% of vaccine serotype and vaccine related serotype carriage rate was observed in non-vaccinated group. The carriage rate was significantly higher compared to the vaccinated group. On the other hand, the non-vaccine-serotype was isolated in the order of 34, 23A, 11A/E, 35B, and 15B in the vaccinated group and the carriage rate was 9.8%. In the nonvaccinated group, isolation was in the order of 34, 23A, and 15B, and the carriage rate was 12.6%. Again, the carriage rate was significantly higher in the non-vaccinated group. Additionally, carriage rate of non-typeable or non-capsule serotypes in the non-vaccinated group was approximately 12.6% while the vaccinated group was approximately 5.6%, so the carriage rate of non-typable and non-capsule serotype was higher in the nonvaccinated group (Table 2).
These results show that in contrast to the past, the carriage rates of 6D for the vaccine related serotype and 34 for the nonvaccine type were markedly increased in both the vaccinated group and non-vaccinated group. In addition, it was reconfirmed that 19F, 23F, and 19A were still residing at high ratios in the nasal cavity of healthy children as in the past.
For the 68 strains of the vaccine and vaccine related serotypes, antimicrobial susceptibility of amoxicillin was 57.4%; intermediate tolerance was 27.9%, and high tolerance was 14.7%. Especially, 19F and 19A all had a tolerance of intermediate or higher, so it was confirmed that vaccination and antibiotic use for these serotypes was a very serious problem in Korea. These strains especially had a high carriage rate in cases where there had been no pneumococcal conjugate vaccine vaccination, and even cases with vaccination showed high carriage rates. However, the 40 non-vaccine serotypes showed amoxicillin susceptibility of 92.5%, intermediate tolerance of 5.0%, and high tolerance of 2.5%, which were entirely different results to the vaccine serotypes. Non-capsular type and non-categorized serotypes had similar results (Table 3).
The sensitivity of S. pneumoniae to oral penicillin was very low at 9.6%, while the intermediate tolerance and high tolerance showed very high results at 37.9% and 52.6%, respectively. MIC50 and MIC90 were both high at 2 µg/mL. The susceptibility of S. pneumoniae to amoxicillin was 73.0%, intermediate tolerance 18.2%, and high tolerance 8.8%, while the distribution of MIC50 was 2 µg/mL and MIC90 4 µg/mL. For amoxicillin/clavulanate, the susceptibility and tolerance of S. pneumoniae was identical to amoxicillin where the susceptibility of the pneumococcus was 73.0%, intermediate tolerance 18.2%, and high tolerance 8.8%, while the MIC50 and MIC90 also showed the same results. Regarding cefaclor, the susceptibility of S. pneumoniae was very low with 9.5%; the intermediate tolerance was 1.5%, while the high tolerance was very high at 89.0%. Additionally, the MIC50 and MIC90 were very high at 64 µg/mL and 128 µg/mL, respectively. The susceptibility of S. pneumoniae for cefdinir was very low at 14.6% and intermediate tolerance 1.5%, while the high tolerance was very high at 83.9%. Additionally, the MIC50 and MIC90 were very high at 4 µg/mL and 8 µg/mL, respectively. The susceptibility of S. pneumoniae for clarithromycin was also very low at 16.1% and the intermediate tolerance 5.8%, while the high tolerance was very high at 78.1%. The MIC50 and MIC90 was 4 µg/mL and 16 µg/mL, respectively (Table 4).
S. pneumoniae forms clusters within the naval cavity of young children and is the main causative agent for respiratory infections and severe invasive infections in infants and young children. It has a high tolerance for antibiotics and is difficult to control [23]. Korea has a high tolerance for S. pneumoniae and has introduced the pneumococcal conjugate vaccine as recommended vaccination since 2003. Epidemiologically, the carriage rate of S. pneumoniae is higher in children than adults and can be different according to region, country, and environment. Regarding season, the carriage rate is higher in the nasal cavity in the summer compared to the winter. Nasopharyngeal clustering of S. pneumoniae is possible from 4 days after birth and on average, occurs starting at 6 months after birth and shows the highest carriage rate before reaching the age to enter school [24]. The S. pneumoniae residing in the nasal cavity is spread to others by droplet infection. Currently, young children in Korea stay in confined spaces such as kindergartens or childcare centers before entering school, and due to this environmental factor, there can be a high pneumococcal carriage rate and a fast spread of tolerance in children under 5 years of age, especially those between 25 to 48 months [18]. The subjects participating in this research were healthy children under 5 years of age, and those who had a history of receiving the pneumococcal conjugate vaccine were all confirmed to have received the PCV 7 three or more times. The research results show that the nasal carriage rate of pneumococcus in the vaccinated group had a vaccine serotype carriage rate of 13.0%, non-vaccine serotype carriage rate of 9.8%, and uncategorized serotype carriage rate of 5.6%, which was lower than the carriage rates of 31.1%, 12.6%, and 12.6% in the non-vaccinated group (Table 2). These results coincide with local and international research results that report that vaccination with pneumococcal conjugate vaccine can effectively reduce the nasopharyngeal carriage rate of S. pneumoniae [13, 14, 25]. Especially in children under 12 months who have no community life, the carriage rate was low in both the vaccinated group and non-vaccinated group and there were no differences in the carriage rate between the two groups. However, in the age where children were sent to childcare or kindergarten, the carriage rates were both higher than the under 12 month age group, and especially in the 12-23, 24-35, and 48-60 month age groups, the carriage rate was significantly different between the vaccinated group and non-vaccinated group. The non-vaccinated group had the highest carriage rate in the 24-35 month age group, so the results show the importance of vaccination to reduce the carriage rate of S. pneumoniae.
According to the complex polysaccharide structure of S. pneumoniae, there are currently 93 serotypes known immunologically, and the serotype distribution is different according to region [25]. The pneumococcal complex polysaccharides antigen is a T-lymphocyte independent antigen; therefore, when administered to those under 2 years or less, vaccine converted to T-lymphocyte dependent antigen through combining with a carrier protein should be administered based on the epidemiological study of serotype according to region and age. Currently the 7, 10, and 13 valent PCV are in use according to the number of included serotypes. There is need for research regarding the distribution of pneumococcal serotypes and resistance for each region to evaluate accurately the effectiveness of the vaccine. For the analysis of the serotype carriage rate in this study (Table 2), the carriage rate for the vaccine type and vaccine related serotype was 13.0% in the vaccinated group and 31.1% in the non-vaccinated group so there was a significant difference between the groups. Additionally, in the non-vaccine type and uncategorized type, the vaccinated group showed a significantly lower carriage rate compared to the non-vaccinated group (Table 2). In the vaccinated group, a total of 43 non-vaccine and uncategorized types were isolated (43/79; 56.3%), while the vaccine and vaccine related types were less isolated with 36 (36/79; 45.6%). However in the non-vaccinated group, a total of 26 non vaccine and uncategorized types were isolated (26/58; 44.8%) while vaccine and related types were isolated more with 32 (32/56; 55.2%). This was similar to overseas research which studied the large influence of vaccination on the carriage rate of vaccine and related types [25]. On the other hand, the 6D serotype, which was first found in Fijian children in 2009, is spreading fast and being reported in several areas including Fiji, South Korea, China, Japan, Hong Kong, Denmark, Poland, Australia, and Peru. It has been mentioned as an important serotype in new vaccine research [22, 25, 26], and also in our study, it was found in 5 children in the vaccinated group (1.8%) and in 7 children in the non-vaccinated group (6.8%) showing the second highest carriage rate after 6A (8.7%). These results are higher than the 2011 domestic Streptococcus pneumoniae serotype epidemiological study [14], indicating that the carriage rate of 6D has increased. Regarding 6D, there is a study reporting that from the 3 sequence types (ST 189, 282, ST 3171), ST282 had high penicillin tolerance [21], but in this study, it was fortunately confirmed that all 3 sequence types have susceptibility to amoxicillin. In the non-vaccine type, the 34 serotype was isolated in 9 cases in the vaccinated group (3.3%) and in 4 cases in the non-vaccinated group (3.9%) showing the highest carriage rate in both groups, but again, it showed nearly no tolerance to amoxicillin. However, the 6D and 34 serotypes are not included in the currently distributed 7, 10, and 13 vaccines; therefore epidemiological research on this should be continued. Especially, cross protection from the 10 and 13 vaccines should be examined.
In young children, it is easy to be infected with antibiotic tolerant, Streptococcus pneumoniae.
Communal life in childcare centers and kindergartens result in the rapid spread of environmentally high multidrug resistant S. pneumoniae. Especially penicillin-resistant S. pneumonia (PRSP) has rapidly increased in Korea since 2000, and Korea has the highest penicillin tolerance in the world [20]. However fortunately, recent domestic antibiotic research shows a susceptibility to amoxicillin of around 80%, and a susceptibility to amoxicillin/clavulanate of around 90%. Additionally, there are few high tolerant strains, so in regions where penicillin tolerance in S. pneumoniae is high like in Korea, the use of these drugs is recommended as first-line oral antimicrobials [1, 3, 14, 19]. On the other hand, cephalosporin affiliated antibiotics mostly had a high tolerance rate, so it was confirmed that they were unsuitable as primary antimicrobials [19, 28]. In our study, the susceptibility of amoxicillin for each serotype showed reduced results overall. In other words, the tolerance rate for the vaccine and vaccine related types was high at 42.6% (intermediate 27.9%, and high 12.4%). Especially for the vaccine type 19F and 19A serotypes, amoxicillin showed a tolerance of intermediate or higher; therefore, it was confirmed to be a serious problem (Table 3). As mentioned above, the carriage rate of 19F and 19A was high in both the non-vaccinated group and the group vaccinated with the PCV 7 (Table 2). However, the tolerance for non-vaccine serotypes was markedly low at 7.5% (intermediate 5%, and high 2.5%). In the overall oral anti microbial susceptibility analysis results, amoxicillin and amoxicillin/clavulanate had high susceptibility at 73%, while penicillin, clarithromycin, cefaclor, and cefdinir had low susceptibility at 9.5%, 16.1%, 9.5%, and 14.6%, respectively (Table 4). Especially clarithromycin showed tolerance in all vaccine serotypes, so caution should be taken when used as a primary antibiotic for a Streptococcus pneumoniae infection. As can be seen, amoxicillin and amoxicillin/clavulanate are the primary antibiotics used for acute respiratory infections caused by pneumococci in young children. However, this research suggests that the choice of antibiotics is limited when primary treatment fails, and problems can arise domestically in choosing antibiotics for 19F and 19A which show tolerance for amoxicillin.
The first limitation of this research concerns the limited seasons spent collecting specimens. The carriage rate of S. pneumoniae in Korea varies according to the month of the year. According to domestic epidemiological study conducted in the past, the highest carriage rate was found from December through February whereas May through July had the lowest carriage rate [18]. Our research is limited in that it was not conducted during the winter season when the carriage rate is highest. Second, regarding the research subjects, the research was concentrated in the region of Seoul and Jeju, and there were only a small number of subjects in the non-vaccinated group. Research overcoming such problems would be conducted all year long in a wider range of areas with more subjects. In addition, the vaccine type had been changed to 10 and 13 at the same time, so the research was unable to compare which type of vaccine had more of an effect on the carriage rate of the new serotypes.
In conclusion, our research results conf irmed that vaccination with pneumococcal conjugate vaccine reduced the pneumococcal carriage rate in the nasal cavity. However, Korea still has a high carriage rate for the 19F and 19A serotypes in both the vaccinated and non-vaccinated groups, so there is need for research and countermeasures to solve the high antibiotic tolerance of these bacteria. In addition, continuous research is required regarding the marked increase in the carriage rate of the 34 and 6D serotypes. To fundamentally solve such problems, selective use of antibiotics and increasing vaccination rates are needed. Furthermore, standards for high-dose antimicrobial treatment using amoxicillin and amoxicillin-clavulanate should be established in the future. Moreover, epidemiological research regarding antimicrobial susceptibility by pneumococcal serotype and nasal carriage rate must be conducted in children who are vaccinated with the 10 and 13 pneumococcal conjugate vaccines.
Figures and Tables
Table 3
Serotype distributions and amoxicillin susceptibility of 137 Streptococcus pneumoniae isolates

References
1. Holmes SJ, Morrow AL, Pickering LK. Child-care practices: effects of social change on the epidemiology of infectious diseases and antibiotic resistance. Epidemiol Rev. 1996. 18:10–28.

2. Kim SM, Hur JK, Lee KY, Shin YK, Park SE, Ma SH, Min AY, Kang JH. Epidemiological study of pneumococcal nasal carriage and serotypes among Korean children. Korean J Pediatr. 2004. 47:611–616.
3. Kim KH, Lee JE, Whang IT, Ryu KH, Hong YM, Kim GH, Lee K, Kang ES, Hong KS. Serogroup and antimicrobial resistance of Streptococcus pneumoniae isolated from oropharynx in children attending day care center. J Korean Pediatr Soc. 2002. 45:346–353.
4. Lee JA, Kim NH, Kim DH, Park KW, Kim YK, Kim KH, Park JY, Choi EH, Lee HJ. Serotypes and penicillin susceptibility of Streptococcus pneumoniae isolated from clinical specimens and healthy carriers of Korean children. J Korean Pediatr Soc. 2003. 46:846–853.
5. Mastro TD, Nomani NK, Ishaq Z, Ghafoor A, Shaukat NF, Esko E, Leinonen M, Henrichsen J, Breiman RF, Schwartz B. Use of nasopharyngeal isolates of Streptococcus pneumoniae and Haemophilus influenzae from children in Pakistan for surveillance for antimicrobial resistance. Pediatr Infect Dis J. 1993. 12:824–830.

6. Klugman KP, Koornhof HJ. Drug resistance patterns and serogroups or serotypes of pneumococcal isolates from cerebrospinal fluid or blood, 1979-1986. J Infect Dis. 1988. 158:956–964.

7. Soh SW, Poh CL, Lin RV. Serotype distribution and antimicrobial resistance of Streptococcus pneumoniae isolates from pediatric patients in Singapore. Antimicrob Agents Chemother. 2000. 44:2193–2196.

8. Charpentier E, Tuomanen E. Mechanisms of antibiotic resistance and tolerance in Streptococcus pneumoniae. Microbes Infect. 2000. 2:1855–1864.

9. Trends in the antimicrobial susceptibility of bacterial respiratory tract pathogens--findings of the Alexander Project 1992-1996. J Chemother. 1999. 11:Suppl 1. 5–21.
10. Finch R. Bacterial resistance-the clinical challenge. Clin Microbiol Infect. 2002. 8:Suppl 3. 21–32. discussion 33-5.

11. Cunha BA. Penicillin resistance in pneumococcal pneumonia. Antibiotics with low resistance potential are effective and pose less risk. Postgrad Med. 2003. 113:42–44. 47–48. 52–54.
12. Yu J, Carvalho Mda G, Beall B, Nahm MH. A rapid pneumococcal serotyping system based on monoclonal antibodies and PCR. J Med Microbiol. 2008. 57:171–178.

13. Huang SS, Hinrichsen VL, Stevenson AE, Rifas-Shiman SL, Kleinman K, Pelton SI, Lipsitch M, Hanage WP, Lee GM, Finkelstein JA. Continued impact of pneumococcal conjugate vaccine on carriage in young children. Pediatrics. 2009. 124:e1–e11.

14. Kim KH, Hong JY, Lee H, Kwak GY, Nam CH, Lee SY, Oh E, Yu J, Nahm MH, Kang JH. Nasopharyngeal pneumococcal carriage of children attending day care centers in Korea: comparison between children immunized with 7-valent pneumococcal conjugate vaccine and non-immunized. J Korean Med Sci. 2011. 26:184–190.

15. Craig WA. Pharmacokinetic/pharmacodynamic parameters: rationale for antibacterial dosing of mice and men. Clin Infect Dis. 1998. 26:1–10. quiz 11-2.

16. Jacobs MR. Optimization of antimicrobial therapy using pharmacokinetic and pharmacodynamic parameters. Clin Microbiol Infect. 2001. 7:589–596.

17. Drusano GL, Craig WA. Relevance of pharmacokinetics and pharmacodynamics in the selection of antibiotics for respiratory tract infections. J Chemother. 1997. 9:Suppl 3. 38–44.
18. Park JY, Kim JH. Pharyngeal colonization rate of penicillin-resistant Streptococcus pneumoniae among day care center children in Seoul, Korea. Korean J Infect Dis. 1999. 31:122–128.
19. Kang JH, Kim SM, Kim JH, Kyun HJ, Lee KY, Shin YK, Park SE, Ma SH, Hong YJ. Penicillin resistant distribution and in vitro susceptibility of oral antibiotics against Streptococcus pneumonia, isolated from pediatric patients with community-acquired respiratory infections in Korea. Korean J Pediatr. 2005. 48:40–47.
20. Kang JH, Lee SY, Kim JH, Hur JK, Lee KY. In vitro antimicrobial activity of cefditoren and other oral antibiotics against Streptococcus pneumoniae, isolated from children with community acquired respiratory tract infections. Jpn J Antibiot. 2010. 63:11–17.
21. Ko KS, Baek JY, Song JH. Multidrug-resistant Streptococcus pneumoniae serotype 6D clones in South Korea. J Clin Microbiol. 2011. 50:818–822.

22. Clinical and Laboratory Standards Institute. Streptococcus pneumoniae. Performance standards for antimicrobial susceptibility testing; twentieth informational supplement. Document M100-S20. 2010. 30. Wayne, PA: Clinical and Laboratory Standards Institute;88–91.
23. Brandileone MC, Di Fabio JL, Vieira VS, Zanella RC, Casagrande ST, Pignatari AC, Tomasz A. Geographic distribution of penicillin resistance of Streptococcus pneumoniae in Brazil: genetic relatedness. Microb Drug Resist. 1998. 4:209–217.
24. Gray BM, Converse GM 3rd, Dillon HC Jr. Epidemiologic studies of Streptococcus pneumoniae infants: acquisition, carriage, and infection during the first 24 months of life. J infect Dis. 1980. 142:923–933.

25. Dagan R, Melamed R, Muallem M, Piglansky L, Yagupsky P. Nasopharyngeal colonization in southern Israel with antibiotic-resistant pneumococci during the first 2 years of life: relation to serotypes likely to be included in pneumococcal conjugate vaccines. J infect Dis. 1996. 174:1352–1355.

26. Jin P, Kong F, Xiao M, Oftadeh S, Zhou F, Liu C, Russell F, Gilbert GL. First report of putative Streptococcus pneumoniae serotype 6D among nasopharyngeal isolates from Fijian children. J Infect Dis. 2009. 200:1375–1380.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download