Abstract
Background
Methicillin-resistant Staphylococcus aureus (MRSA) has become a one of the most important causes of nosocomial infections, and use of vancomycin for the treatment of MRSA infection has increased. Unfortunately, vancomycin-resistant enterococcus have been reported, as well as vancomycin-resistant S. aureus. Arbekacin is an antibacterial agent and belongs to the aminoglycoside family of antibiotics. It was introduced to treat MRSA infection. We studied the clinical and bacteriological efficacy and safety of arbekacin compared to vancomycin in the treatment of infections caused by MRSA.
Materials and Methods
This was a retrospective case-control study of patients who were admitted to tertiary Hospital from January 1st, 2009 to December 31st, 2010, and received the antibiotics arbekacin or vancomycin. All the skin and soft tissue MRSA infected patients who received arbekacin or vancomycin were enrolled during the study period. The bacteriological efficacy response (BER) was classified with improved and failure. The improved BER was defined as no growth of MRSA, where failure was defined as growth of MRSA, culture at the end of therapy or during treatment. Clinical efficacy response (CER) was classified as improved and failure. Improved CER was defined as resolution or reduction of the majority of signs and symptoms related to the original infection. Failure was defined as no resolution and no reduction of majority of the signs and symptoms, or worsening of one or more signs and symptoms, or new symptoms or signs associated with the original infection or a new infection.
Results
Totally, 122 patients (63/99 in arbekacin, 59/168 in vancomycin group) with skin and soft tissue infection who recieved arbekacin or vancomcyin at least 4 days were enrolled and analysed. The bacteriological efficacy response [improved, arbekacin vs vancomycin; 73.0% (46/63), 95% confidence interval (CI) 60.3 to 83.4% vs 83.1% (49/59), 95% CI 71.0 to 91.6%] and clinical efficacy response [improved, arbekacin vs vancomycin; 67.2% (41/61), 95% CI 52.0 to 76.7% vs 78.0% (46/59), 95% CI 65.3 to 87.7%] were similar between the two groups (P=0.264, 0.265). The complication rate was significantly higher in the vancomycin group [29/59(49.2%), 95% CI 35.9 to 62.5%] than arbekacin [10/63(15.9%), 95% CI 8.4 to 29.0%] (P<0.001).
Skin and soft tissue infections (SSTIs) are one of the most common clinical diseases acquired from the community and nosocomially. These types of infections involve acute wounds, such as surgical site infections, diabetic foot ulcers, traumatic infections, and chronic infections, such as abscesses and bedsores [1, 2].
SSTIs are generally classified according to the depth of the lesions and are classified as superficial SSTIs, which include erysipelas, cellulitis, simple abscesses, furunculus, and wound infections, where complicated SSTIs involve necrotizing fascitis, myopathies, gas gangrene, with the latter conditions needing surgical intervention or systemic antimicrobial therapy [3]. Staphylococcus aureus (S. aureus ) is one of the most common pathogens of SSTIs. It is also amongsts the resistant strain types known as methicillin-resistant S. aureus (MRSA), which is increasing trend, with recent statistics reporting that amongst the S. aureus isolated in tertiary hospitals of Korea, about 60-70% are identified as MRSA [4-7].
As MRSA have been classified as one of the most important nosocomial pathogen, the use of glycopeptide antibiotics, such as vancomycin, which is considered as a standard therapy to MRSA infections, have been increased greatly.
With the emergence of strains that have a reduced susceptibility to vancomycin [8, 9], the introduction of a new class of antibiotics is required in order to substitute glycopeptide antibiotics.
Arbekacin is an aminoglycoside antibiotic, which is approved for use in MRSA infections, have pharmacodynamic advantages, such as concentration-dependant bactericidal activities, along with a prolonged post antibiotic effect relative to vancomycin [10].
There are reports that no single isolate with Arbekacin MIC among MRSA strains isolated in Korea was greater than 4 µg/mL, yet clinical data are still lacking [11, 12].
Therefore, the authors evaluated the efficacy and safety of arbekacin in comparison to vancomycin for the treatment of SSTIs caused by MRSA.
This study was conducted as a case-control, retrospective observational study at Chonbuk National University Hospital, a 1,100-bed tertiary care hospital, in Jeonju, Korea. All patients admitted to the hospital who received arbekacin or vancomycin from January, 2009 to December, 2010 for treatment of SSTI caused by MRSA were enrolled. Patients who have been administered for longer than 4 days were included in the study as study subjects, and those who had concomitant administration of arbekacin and vancomycin were excluded from this study. Clinical data were collected from electronic medical records, concerning age, sex, clinical diagnosis, microbial identification with antibiotic susceptibility, concomitant antibiotics, duration of antibiotics treatment and adverse reactions.
The efficacy was analyzed in the bacteriological efficacy response (BER) and the clinical effi cacy response (CER), and the improvements or failures were classifi ed with reference to the published studies. Improved BER was defi ned as no growth of MRSA in cultures obtained from the original site of infection, or a clinical status of the cure made a repeat culture unnecessary, failure was defi ned as the growth of MRSA during the treatment or even at the end of the treatment.
Improvements in the CER were defined as the resolution or reduction of a majority of the signs and symptoms related to the original infection, and failure was defined as no resolution or the reduction of a majority of the signs and symptoms related to the original infection, the exacerbation of the signs and symptoms, or the development of new symptoms due to a new infection or the original infection [13].
Amongst the study subjects, 2 patients who transferred to another hospital during the treatment were excluded from the analysis.
The patients were classified according to the following underlying diseases; cancer, cerebral diseases, diabetes mellitus, pulmonary diseases, and cardiovascular diseases. Among cancers, there were cases of gastric cancer, colorectal cancer, lung cancer, breast cancer, liver cancer, esophageal cancer, biliary cancer, and leukemia. Cerebral infarctions, cerebral hemorrhages, epidural abscesses, and traumatic brain injury patients were included in the category of cerebral diseases. Pulmonary diseases included chronic obstructive pulmonary disease and asthma, and cardiovascular diseases included hypertension and heart failure, myocardial infarction.
Community-acquired MRSA were defined as patients who had positive results from specimens collected within 48 hours of hospital admissions and also no previous history of hospital visits. Bacteremia was defined as the isolation of MRSA in the blood.
The safety assessment was evaluated by analyzing the results of complete blood count and blood chemistry tests regarding signs and symptoms that indicated abnormality related to medication used during the therapy and the contents stated in electronic medical records. Nephrotoxicity was defined as at least a 50% reduction in glomerular filtration rate (GFR) using the abbreviated modifed diet in renal disease (MDRD) equation, which was GFR (mL/min/1.73 m2) = 186 Pcr-1.154 × age-0.203 × (1.212 if black) × (0.742 if female) [14]. Hepatotoxicity was defined as an elevation in aspartate aminotransferase/alanine aminotransferase (AST/ALT) levels more than two times baseline values during treatment. Leukopenia was defined as a continuous decrease lower than 4.8×103/µL in the number of white blood cells found in complete blood cell counts during treatment. Skin rash and drug fever, due to the medications, were assessed based on the contents of the written electronic medical records.
Categorical variables were compared using the Chi-square test or Fisher's exact test. Continuous variables were tested for normal distribution and compared using the unpaired t-test if data were determined to be normally distributed or using the Mann-Whitney U test for nonparametric data. Chi-square test, Fisher's exact test and t-test were analyzed by using SPSS 19.0 (IBM Corp., NY, USA), and the P-value lower than 0.05 (twotailed) was defined as statistically significant.
During the study period, there were a total of 99 patients who received arbekacin for longer than 4 days, and from these, 63 SSTI patients were included in the study subject population. In addition, there were a total of 168 patients who received vancomycin for longer than 4 days, but only 59 SSTI patients were selected as the final study subjects, with a total of 122 patients being analyzed (Table 1).
The mean (standard deviation, SD) age of the study population was 51.2 (16.3) years old for the arbekacin group, and 57.9 (14.6) years old for the vancomycin group, where the age of the vancomycin group was statistically higher than the arbekacin group (P=0.018).
The mean duration of action for arbekacin and vancomycin was 17.0 and 19.0, respectively, where there was no significant difference between two groups (P=0.482).
Polymicrobial infections occurred in 55.6% (35/63) of the arbekacin group and 28.8% (17/59) of the vancomycin group, and more than 1 comorbid underlying disease was present in 54% (34/63) of the arbekacin group and 74.6% (44/59) of the vancomycin group (P=0.029).
There was no statistical difference in the arbekacin group and the vacomycin group when comprised of patients with bacteremia (P=0.121, arbekacin vs vancomycin, 6.3% vs. 16.9%). Also, there was no difference between the groups with patients who had community acquired S. aureus infections (P=0.154, arbekacin vs vancomycin, 3.2% vs. 10.2%).
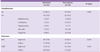
The prevalence of the following adverse reactions of more than once; nephrotoxicity, hepatotoxicity, leukopenia, skin rash, drug fever, etc., were 15.9% (10/63) in the arbekacin group, but 49.2% (29/59) in the vancomycin group, with the incidence rate for adverse reactions in the arbekacin group being statistically and significantly low (P<0.001, Table 2).
Nephrotoxicity, hepatotoxicity, leukopenia, and skin rash occurred with both drugs, but the occurrence of drug fever was only observed in the vancomycin group.
The number of cases of antibiotic change due to the incidence of adverse reactions were 2 cases in the arbekacin group and 11 cases in the vancomycin group (data not shown).
For the treatment outcomes, the BER in the arbekacin group was 73.0% (95% CI 60.3 to 83.4%) and 83.1% (95% CI 71.0 to 91.6%) in the vancomycin group, where the BER with vancomycin was 10.1% higher, but there were no differences observed between the groups (P=0.264), and the CER in the arbekacin group was 67.2% (95% CI 52.0 to 76.7%), and 78.0% (95% CI 65.3 to 87.7%) in the vancomycin group, which was higher in the vancomycin group, but there were no statistical differences observed as well (P=0.265).
The prevalence of skin and soft tissue infections (SSTI) is due to various pathogens, and Moet et al. reported that among the bacteria isolated from North America, South America, and Europe in 1998-2004, 44.6% of them were identified as S. aureus, while also including P. aeruginosa, Enterococcus species, E. coli, which were reported as other common bacterial isolates.
The resistance trends of the pathogens of skin and soft tissue infections presented the general increase of MRSA, VRE, ESBL producing E. coli and Klebsiella species and among these, the increase of MRSA was significant in 1998, with it consisting 26.2% of all S. aureus isolates, however in 2004, it reached 47.4% [5].
The rate of methicillin resistance from S. aureus in tertiary hospitals of Korea is 60-70%, which is higher than the reports from previous studies [6, 7], while with the increase in use of vancomycin for the treatment of MRSA, there is an increasing trend in vancomycin resistant isolates, such as VISA and VRSA.
There is a limit to the choices of antibiotics with the increase in multi-drug resistant bacteria within the hospital, so an increase in the mortality rate due to the emergence of bacterial pathogens which cannot be treated with antibiotics can be a problem.
As a characteristic of the concentration dependent bactericidal activity, arbekacin has pharmacodynamic advantages, such as a prolonged post-antibiotic effect in comparison to vancomycin, and it has been reported to have high in vitro susceptibility to MRSA isolates in Korea. This characteristic is in turn being noticed as a new antibiotic function, where arbekacin may replace glycopeptide antibiotics, such as vancomycin [10-12].
However, the comparative clinical efficacy and safety study between arbekacin and vancomycin are very limited, so the authors have conducted a retrospective study in order to evaluate the efficacy and safety of arbekacin and vancomycin in MRSA infections [15].
Although age and sex matching were done, when comparing arbekacin and vancomycin, there was a difference in the clinical indication distribution, so for a more accurate comparison, the clinical efficacy and safety were compared in the limited areas of the skin and soft tissue.
As a result of this study, arbekacin treatment in MRSA skin and soft tissue infections showed very similar efficacy results to vancomycin, where adverse reactions were more frequently observed in the vancomycin group than the arbekacin group.
Therefore, arbekacin can be considered to be an appropriate drug of choice instead of vancomycin for MRSA skin and soft tissue infections. Furthermore, the reduction in the use of vancomycin for hospital infections and the lowering of the incidence rate of vancomycin resistant isolates, such as VRE and VISA, can be expected in the clinical setting.
In diabetic foot ulcer patients, the infection caused by MRSA can lead to shock and lower limb amputation due to bacteremia and sepsis, while it also directly increases the mortality rate [16]. Vancomycin is still used as the primary drug of choice for the treatment of MRSA infections, but there have been reports about isolates with a lowered sensitivity to vancomycin [17], and also, the emergence of vancomycin resistant Staphylococcus aurues in the clinical setting [18].
Although the VRSA infection rate is very low, the problem of antibiotic resistance is a common problem faced worldwide, which has been classified by WHO as being a serious risk to the public health.
Therefore, not only the careful use of vancomycin but also the development of alternative treatments for MRSA infections is needed.
Arbekacin is a derivative of aminoglycoside dibekacin, and it has been reported with a good in vitro activity against MRSA [19, 20].
In Europe and Japan, there have been reports that most MRSA are sensitive to arbekacin [21], with a clinical report reporting that the effect of arbekacin is comparable to vancomycin for the treatment of MRSA infections [22, 23].
Lee et al. reported that an arbekacin based combination therapy can substitute glycopeptide antibiotics for the treatment of MRSA or hetero-VISA infections, and the study concluded that there was no difference in the clinical efficacy between arbekacin and vancomycin [20].
This study can also be evidence that arbekacin can be a drug of choice for the substitution of glycopeptide antibiotics.
Vancomycin has adverse reactions, such as local thrombophlebitis, fever, leukopenia, skin rash, and nephrotoxicity [24], so it requires the continuous therapeutic drug monitoring of the blood, and due to the adverse reactions and tissue hypersensitivity, intramuscular injections are impossible when an intraveous injections are carried out.
Also, ear toxicity and severe allergic reactions are other well known adverse reactions [25]. Arbekacin also has adverse reactions, such as renal toxicity and ear toxicity, which are similar to other aminoglycoside [19]. Through this study, the authors confirmed the incidence rate of the adverse reactions as being statistically low in the arbekacin group.
However, in this study, due to the low number of subjects, the strength of the tests on the comparison of antibiotic efficacy was 0.265, which is considered to be low, (when the significance level is 0.05, n1 = 63, n2 = 59, p1 = 0.73, p2 = 0.831), by using the comparison of the 2 ratios, for a probability of 80% to detect a 10.1% difference in the efficacy under a significance level of 5%, it was calculated that a total of 526 patients needed to be recruited, with 263 patients in each group.
Although the clinical efficacy between arbekacin and vancomycin did not show a statistical difference, the conclusion that arbekacin is non-inferior in comparison to vancomycin cannot be made.
However, this study has sufficient significance as a preliminary study in conducting a prospective randomized case control study in the future, or as an observatory study which can support clinical decisions with a lack of data for that situation.
For other limitations, in the case of continuous MRSA growth, despite treatment with vancomycin in the MRSA SSTI patients, the antibiotics recommended in the MRSA treatment guidelines; linezolid, daptomycin, and quinupristin-dalfopristin, should be considered first before the introduction of arbekacin [26].
In conclusion, arbekacin showed similar clinical efficacy and excellence in safety in comparison to vancomycin. The authors consider arbekacin to be a reasonable substitute for vancomycin as a primary choice of antibiotic for the treatment of MRSA SSTIs. However, small number of subjects was major limitations in this study. In a near future, well-designed studies are required in order to evaluate the clinical efficacy between arbekacin and vancomycin.
Figures and Tables
Table 1
General characteristics of the study population
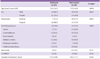
CA-MRSA, community acquired methicillin resistant Staphylococcus aureus.
Age data normally distributed was presented as mean (SD) and analyzed with the independent t-test.
Duration of treatment data not normally distributed was presented as median (range) and analyzed with the Mann-Whitney U test.
All other data were presented as number (%) and analyzed with the Chi-square test excepta.
bAnalyzed with Fisher's exact test.
References
1. Nichols RL, Florman S. Clinical presentations of soft-tissue infections and surgical site infections. Clin Infect Dis. 2001. 33:Suppl 2. S84–S93.

2. Wilson SE. Clinical trial results with linezolid, an oxazolidinone, in the treatment of soft tissue and postoperative gram-positive infections. Surg Infect (Larchmt). 2001. 2:25–35.

3. Nichols RL. Optimal treatment of complicated skin and skin structure infections. J Antimicrob Chemother. 1999. 44:Suppl A. 19–23.

4. Kirby JT, Mutnick AH, Jones RN, Biedenbach DJ, Pfaller MA. Geographic variations in garenoxacin (BMS284756) activity tested against pathogens associated with skin and soft tissue infections: report from the SENTRY Antimicrobial Surveillance Program (2000). Diagn Microbiol Infect Dis. 2002. 43:303–309.

5. Moet GJ, Jones RN, Biedenbach DJ, Stilwell MG, Fritsche TR. Contemporary causes of skin and soft tissue infections in North America, Latin America, and Europe: report from the SENTRY Antimicrobial Surveillance Program (1998-2004). Diagn Microbiol Infect Dis. 2007. 57:7–13.

6. Chung GT, Cha JG, Han SY, Jang HS, Lee KM, Yoo JI, Yoo JS, Kim HB, Eun SH, Kim BS, Park O, Lee YS. Nationwide surveillance study of vancomycin intermediate Staphylococcus aureus strains in Korean hospitals from 2001 to 2006. J Microbiol Biotechnol. 2010. 20:637–642.
7. Lee K, Lee MA, Lee CH, Lee J, Roh KH, Kim S, Kim JJ, Koh E, Yong D, Chong Y. KONSAR Group. Increase of ceftazidime- and fluoroquinolone-resistant Klebsiella pneumoniae and imipenem-resistant Acinetobacter spp. in Korea: analysis of KONSAR study data from 2005 and 2007. Yonsei Med J. 2010. 51:901–911.

8. Hiramatsu K, Hanaki H, Ino T, Yabuta K, Oguri T, Tenover FC. Methicillin-resistant Staphylococcus aureus clinical strain with reduced vancomycin susceptibility. J Antimicrob Chemother. 1997. 40:135–136.

9. Walsh TR, Howe RA. The prevalence and mechanisms of vancomycin resistance in Staphylococcus aureus. Annu Rev Microbiol. 2002. 56:657–675.

10. Watanabe T, Ohashi K, Matsui K, Kubota T. Comparative studies of the bactericidal, morphological and post-antibiotic effects of arbekacin and vancomycin against methicillin-resistant Staphylococcus aureus. J Antimicrob Chemother. 1997. 39:471–476.

11. Lee J, Kim CK, Roh KH, Lee H, Yum JH, Yong D, Lee K, Chong Y. In vitro activity of arbekacin against clinical isolates of Staphylococcus species and Gram-negative Bacilli. Korean J Lab Med. 2007. 27:292–297.

12. Wie SH, Kang JH, Huh DH, Lee DG, Kim SI, Kim YR, Choi JH, Kim JH, Yoo JH, Hur JK, Shin WS, Kang MW. Antimicrobial activities of arbekacin against clinical isolates of Staphylococcus aureus and coagulase-negative Staphylococcus species. Korean J Infect Dis. 2001. 33:254–260.
13. Kim TH, Choo EJ, Lee MS, Kim NJ, Woo JH, Ryu J, Chang MS, Yum YK. Clinical efficacy and safety with arbekacin for methicillin-resistant Staphylococcus aureus (MRSA) infections. Korean J Med. 2003. 65:239–244.
14. Manjunath G, Sarnak MJ, Levey AS. Prediction equations to estimate glomerular filtration rate: an update. Curr Opin Nephrol Hypertens. 2001. 10:785–792.

15. Hwang JH, Lee JH, Moon MK, Kim JS, Won KS, Lee CS. The usefulness of arbekacin compared to vancomycin. Eur J Clin Microbiol Infect Dis. 2012. 31:1663–1666.

16. Holmberg SD, Solomon SL, Blake PA. Health and economic impacts of antimicrobial resistance. Rev Infect Dis. 1987. 9:1065–1078.

17. Wang G, Hindler JF, Ward KW, Bruckner DA. Increased vancomycin MICs for Staphylococcus aureus clinical isolates from a university hospital during a 5-year period. J Clin Microbiol. 2006. 44:3883–3886.

18. Sievert DM, Rudrik JT, Patel JB, McDonald LC, Wilkins MJ, Hageman JC. Vancomycin-resistant Staphylococcus aureus in the United States, 2002-2006. Clin Infect Dis. 2008. 46:668–674.

19. Sato R, Tanigawara Y, Kaku M, Aikawa N, Shimizu K. Pharmacokinetic-pharmacodynamic relationship of arbekacin for treatment of patients infected with methicillin-resistant Staphylococcus aureus. Antimicrob Agents Chemother. 2006. 50:3763–3769.

20. Lee DG, Chun HS, Yim DS, Choi SM, Choi JH, Yoo JH, Shin WS, Kang MW. Efficacies of vancomycin, arbekacin, and gentamicin alone or in combination against methicillin-resistant Staphylococcus aureus in an in vitro infective endocarditis model. Antimicrob Agents Chemother. 2003. 47:3768–3773.

21. Hamilton-Miller JM, Shah S. Activity of the semi-synthetic kanamycin B derivative, arbekacin against methicillin-resistant Staphylococcus aureus. J Antimicrob Chemother. 1995. 35:865–868.

22. Suzuki K. Efficacy and safety of arbekacin for staphylococcal infection in the NICU. Pediatr Int. 2003. 45:301–306.

24. Lodise TP, Patel N, Lomaestro BM, Rodvold KA, Drusano GL. Relationship between initial vancomycin concentration-time profile and nephrotoxicity among hospitalized patients. Clin Infect Dis. 2009. 49:507–514.

25. Ryu JS, Woo JH, Kim KW, Kim TH, Kim YH. Efficacy of teicoplanin in gram-positive bacterial infection. Korean J Infect Dis. 1992. 24:183–189.
26. Liu C, Bayer A, Cosgrove SE, Daum RS, Fridkin SK, Gorwitz RJ, Kaplan SL, Karchmer AW, Levine DP, Murray BE, J Rybak M, Talan DA, Chambers HF. Clinical practice guidelines by the infectious diseases society of america for the treatment of methicillin-resistant Staphylococcus aureus infections in adults and children: executive summary. Clin Infect Dis. 2011. 52:285–292.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download