Abstract
Although, erythema nodosum is a common skin manifestation associated with syphilis, nodular vasculitis is a rare feature. Here, we describe a case of a 22-year-old, human immunedeficiency virus negative, non-immunocompromised man who developed recurrent oral and scrotal ulcers with nodular lesions of the lower extremitie. Behçet's disease was initially suspected, however, his serologic test for syphilis was positive, and he was thus diagnosed with secondary syphilis, with a skin biopsy showing nodular vasculitis. The patient was treated with benzathine penicillin, and the skin lesions disappeared after treatment.
Syphilis is a chronic systemic condition, and its incidence has been increasing recently in association with human immunodeficiency virus (HIV) coinfection. According to the Korean Centers for Disease Control and Prevention (KCDC), the average annual incidence of registered early syphilis is approximately 1/100,000 on Jeju Island. The clinical features of secondary syphilis, often described as "the great imitator". Skin lesions commonly mimic those of other diseases, such as malignancy, sarcoidosis, inflammatory bowel disease, and Behçet's disease (BD) [1-8]. Although cutaneous manifestations related to secondary syphilis are well-recognized, nodular vasculitis is extremely rare. Histopathology of Nodular vasculitis are an affliction of the hypodermic vessels, and of a migratory thrombophlebitis, and betray subjacent venous alterations [9]. These lesions should be distinguished from erythema nodosum, polyarteritis nodosa, tuberculosis, and deep fungal infection. We report an interesting case of secondary syphilis in a non-HIV patient presenting with uncommon clinical features resembling BD and histopathological features of nodular vasculitis.
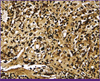
A 22-year-old man visited the Department of Rheumatology with several months history of recurrent oral ulcers, genital erosions (Fig. 1A) and crops of hyperpigmented tender nodules located on both shins (Fig. 1B). The initial diagnosis was BD, which led to the initiation of steroid therapy. After 1 week, the nodular skin lesions on both shins had slightly improved, but the genital erosions and oral ulcers were aggravated and fever developed. To evaluate the patients for other diseases, the serum rapid plasma reagin (RPR) test was performed, and the result was positive. The patient had no history of medication before the appearance of the skin lesions. He did, however, have a history of heterosexual intercourse with multiple partners without the use of a condom. Laboratory profiling revealed a white blood cell count of 7,900/mm3, a hemoglobin level of 16.3 g/dL, a platelet level of 313,000/mm3, and a high sensitivity C-reactive protein level of 7.57 mg/dL. Hepatitis B, hepatitis C, and HIV serology were negative. The immunoglobulin (Ig) M-fluorescent treponemal antibody absorption test (FTA-ABS), the IgG-FTA-ABS, and the Treponema pallidum hemagglutination assay were all reactive. Spirochetes were also identified in a scrotal specimen using the Warthin-Starry stain (Fig. 2). The results of skin biopsies from his shins were concordant with nodular vasculitis (Fig. 3). After the diagnosis of secondary syphilis was made, intramuscular benzathine penicillin G was immediately initiated at a dosage of 2.4 MU once per week for 3 weeks. After the initiation of penicillin treatment, his signs and symptoms, including skin lesions, gradually improved. All lesions had resolved after 3 months. Non treponemal titer was also decreased from 2.6 RPR unit (R.U) to 1.5 R.U.
According to the KCDC, the yearly reported number of syphilis cases has increased 2-fold from 586 in the year of 2003 to 1,424 in the year of 2007. This may be related to increased incidence of HIV infection: cases of coinfection with syphilis and HIV have been reported in Korea. Therefore, syphilis may become a more common clinical challenge [10].
The diagnosis of syphilis depends upon clinical features, the observation of the organisms by dark-field examination, the use of serologic tests, and the application of other new tests such as immunofluorescent staining and polymerase chain reaction assays [11, 12]. However, the variable clinical courses, diverse manifestations, and various histological patterns of syphilis provide clinicians with diagnostic challenges.
The most common mucocutaneous manifestation of secondary syphilis is a generalized non-pruritic symmetric maculopapular eruption that is purple, pink, or coppery-brown, usually involving the palms and soles. Cutaneous manifestations of syphilis can also present as polymorphous features that include macular, maculopapular, nodular, nodulo-ulcerative, pustular, and follicular lesions, mucositis, alopecia, and alteration of nails [13].
Nodular vasculitis and erythema induratum are uncommon types of lobular panniculitis that have overlapping clinical and histological features. In general, nodular vasculitis is commonly associated with tuberculosis, but is also associated with other nontuberculous infections and noninfectious conditions. Nontuberculous infectious agents that can cause nodular vasculitis include Nocardia, Pseudomonas, Fusarium, hepatitis B virus and hepatitis C virus. Noninfectious disease and agents associated with the condition include hypothyroidism, chronic lymphocytic leukemia, rheumatoid arthritis, Crohn's disease, and drugs such as propylthiouracil [14]. The pathology of nodular vasculitis suggests type III and type IV hypersensitivity reactions [15], and they present as recurrent erythematous tender violaceous nodules and plaques on the posterior lower leg. The lesions are occasionally accompanied by leg edema. The nodules usually evolve ulcerations, depressed scars, atrophy, and hyperpigmentation. The histological findings show diffuse lobular granulomatous panniculitis with primary neutrophilic vasculitis and thrombosis affecting nearby small to medium-sized arteries and veins [14].
In our case, the patient presented with multiple tender erythematous subcutaneous nodules on both shins, painless well-marginated oral ulcers, and painful pruritic well-defined elliptical crusted genital erosions. Although such oral ulcers and genital erosions are not typical aphthous ulcers, the patients was initially diagnosed with BD because the skin lesions mimicked the symptoms of erythema nodosum, which is frequently associated with BD. No other skin lesions were apparent except for the nodules on both shins and the orogenital erosions. There were no characteristic findings of secondary syphilis, such as papulosquamous lesions of the palmoplantar areas or trunk. Finally, his shins lesions were found to be nodular vasculitis, a rare cutaneous manifestation of secondary syphilis. It maybe that the orogenital ulcerative lesions were chancre or mucosal lesions often found in secondary syphilis. To the best of our knowledge, this is first reported case of nodular vasculitis as a manifestation of secondary syphilis. The classic histopathologic findings of secondary syphilis are plasma cell infiltrates and vascular changes, including endarteritis obliterans. However, these characteristics are absent in about 25% of all cases [16]. Ackerman classified the histologic patterns of secondary syphilis as follows: (1) superficial perivascular dermatitis with epidermal hyperplasia; (2) superficial/deep perivascular dermatitis; (3) dense diffuse dermatitis with granulomatous infiltrates [17]. Our case could be considered as representative of the third subtype. Compared with traditional cases of secondary syphilis, our patients had fewer plasma cell infiltrates, Instead, histopathologic findings such as lobular granulomatous inflammation, thrombosis and fibrinoid necrosis of septal blood suggested nodular vasculitis in our case. It should be emphasized that nodular vasculitis is different from nodular syphilis. Although nodular syphilis is a unique variant of secondary syphilis, it is usually found on the face, palms, soles, or upper trunk. The lesions of nodular syphilis characteristically show central regression, centrifugal spreading, and lamellar crusts, findings that were absent in this case. Moreover, the histopathologic findings of our patient as mentioned above also suggest nodular vasculitis. Because our patient was at a relatively early stage of disease, the surface alterations of atrophy, depression and scars on his shins were not been found.
In conclusion, syphilis has become a major health problem, and its diverse characteristics lead to diagnostic difficulties. Thus, it is important to consider this disease in patients with atypical systemic manifestation who are at risk of sexually transmitted disease. The initial incorrect treatment and consequent failure in our patient prompted suspicion of syphilis and once the appropriate diagnosis was made, suitable treatment was given. As a result, the patient was responded well and did not sequelae.
Figures and Tables
 | Figure 1(A) Multiple elliptical crusted erosions are found on the scrotum. (B) Crops of hyperpigmented tender nodules are located on both shins. |
References
1. Skowron G, Wang X, Gupta E. Infectious syphilis: the return of the great imitator to Rhode Island. Med Health R I. 2012; 95:245–248.
2. Breznik V, Potočnik M, Miljković J. Papulonodular secondary syphilis in a 52-year-old non-HIV heterosexual patient. Acta Dermatovenerol Alp Panonica Adriat. 2010; 19:27–30.
3. Moon HS, Park K, Lee JH, Son SJ. A nodular syphilid presenting as a pseudolymphoma: mimicking a cutaneous marginal zone B-cell lymphoma. Am J Dermatopathol. 2009; 31:846–848.

4. ul Bari A, Raza N. Secondary syphilis clinically mimicking pseudolymphoma of the face. Dermatol Online J. 2006; 12:20.
5. Roett MA, Mayor MT, Uduhiri KA. Diagnosis and management of genital ulcers. Am Fam Physician. 2012; 85:254–262.
6. Meljanac N, Dippel E, Zouboulis CC. Superimposed primary chancre in a patient with Adamantiades-Behcet's disease. Sex Transm Infect. 1999; 75:124–125.

7. Vasconcelos P, Borges-Costa J, Loreto H, Marques S. Secondary syphilis mimicking inflammatory bowel disease. Sex Transm Infect. 2013; 89:98–99.

9. Kint A. Non-venolymphatic cellulitis. Phlebologie. 1981; 34:543–550.
10. Kim J, Kim WH, Cho C, Kim J, Kim GY, Nam MH, Kim JS, Bae SY, Cho Y. Evaluation of automated architect syphilis TP as a diagnostic laboratory screening test for syphilis. Korean J Lab Med. 2008; 28:475–482.

11. Liu H, Rodes B, Chen CY, Steiner B. New tests for syphilis: rational design of a PCR method for detection of Treponema pallidum in clinical specimens using unique regions of the DNA polymerase I gene. J Clin Microbiol. 2001; 39:1941–1946.

12. Chen CY, Chi KH, George RW, Cox DL, Srivastava A, Rui Silva M, Carneiro F, Lauwers GY, Ballard RC. Diagnosis of gastric syphilis by direct immunofluorescence staining and real-time PCR testing. J Clin Microbiol. 2006; 44:3452–3456.

13. Dourmishev LA, Dourmishev AL. Syphilis: uncommon presentations in adults. Clin Dermatol. 2005; 23:555–564.

14. Gilchrist H, Patterson JW. Erythema nodosum and erythema induratum (nodular vasculitis): diagnosis and management. Dermatol Ther. 2010; 23:320–327.

15. Schneider JW, Jordaan HF. The histopathologic spectrum of erythema induratum of Bazin. Am J Dermatopathol. 1997; 19:323–333.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download