Abstract
Background
The purpose of this study was to compare the outcome of carbapenem versus non-carbapenem antimicrobial therapy for pediatric urinary tract infections (UTIs) caused by extended-spectrum β-lactamase (ESBL) producing Enterobacteriaceae.
Materials and Methods
From 2006 to 2011, 42 episodes of UTI caused by ESBL-producing Enterobacteriaceae were diagnosed at Seoul National University Children's Hospital. Patients were grouped according to the antimicrobials they received into a carbapenem group and a non-carbapenem group. Medical records were retrospectively reviewed to assess treatment outcome, time to defervescence after initiation of treatment, and relapse rate.
Results
There were 36 children with 42 episodes of UTI caused by ESBL-producing Enterobacteriaceae. Twenty-seven cases (64%) had an underlying urologic disease, 28 (67%) cases were caused by Escherichia coli, and 14 (33%) cases were caused by Klebsiella pneumoniae. Four (10%) cases were treated with carbapenem, 23 cases (55%) were treated with non-carbapenem, and 15 (36%) cases were treated by switching from a carbapenem to a non-carbapenem and vice versa. There was no treatment failure at the time of antimicrobial discontinuation. Between the carbapenem and the non-carbapenem treatment groups, there were no significant differences in bacterial etiology (P = 0.59), time to defervescence after the initiation of antimicrobials (P = 0.28), and relapse rate (P = 0.50). In vitro susceptibility to non-carbapenem antimicrobials did not affect the time to defervescence after the initiation of antimicrobial treatment, and the relapse rate in the non-carbapenem group.
Conclusions
This study found no significant difference in the treatment outcome between pediatric patients treated with carbapenem and those treated with non-carbapenem antimicrobials for UTI caused by ESBL-producing Enterobacteriaceae. Therefore, the initially administered non-carbapenem can be maintained in UTI patients showing clinical improvement.
The most common causes of pediatric urinary tract infections are Enterobacteriaceae such as Escherichia coli and Klebsiella pneumoniae [1]. In general, broad-spectrum cephalosporin antimicrobials are administered empirically. However, with the increased use of antimicrobials, resistant strains are emerging. In 1983, extended-spectrum β-lactamases (ESBL) producing K. pneumoniae was first described [2], and subsequently in 1987, ESBL-producing E. coli was reported [3]. Since then, ESBL-producing bacteria have been increasing worldwide [4, 5].
ESBL are plasmid-mediated enzymes that show resistance to broad-spectrum cephalosporins and monobactams including the newer β-lactam antimicrobials [6]. Currently, the treatment of choice against these resistant strains is carbapenem, and it is thought that there is no alternative treatment. However, clinically, there have been reports of successfully treated UTI caused by ESBL-producing bacteria with a non-carbapenem [7, 8]. A recent study showed that cephamycins are stable against the hydrolytic activity of ESBL by comparing the treatment outcome of UTI caused by ESBL-producing bacteria in cefmetazole treated patients and carbapenem treated patients. The results showed no significant difference in the treatment outcome [9].
So far, many studies have assessed the risk factors of UTI caused by ESBL-producing Enterobacteriaceae [10-14], but only a few studies have compared the treatment outcome of patients administered with a carbapenem versus a non-carbapenem [15]. Even fewer studies have analyzed the relapse rate, especially in pediatric patients. Recently, the increase in the emergence of carbapenem resistant bacteria has brought an awareness of the need to minimize the use of carbapenem [16]. Therefore, the aim of this study was to compare the treatment outcome and relapse rate in pediatric patients treated with a carbapenem and those treated with a non-carbapenem for UTI caused by ESBL-producing Enterobacteriaceae.
This study was carried out at a tertiary university children's hospital (Seoul National University Children's Hospital) with 350 beds. The subjects in this study were pediatric patients diagnosed with UTI caused by ESBL-producing Enterobacteriaceae during a six-year period, from January 2006 to December 2011.
A retrospective analysis of the electronic medical record (EMR) was carried out to obtain information on the subject's gender, age, underlying urologic disease, prior antimicrobials use, history of urinary tract infection, type of antimicrobials, time to defervescence after the start of antimicrobials, urine culture and pyuria negative conversion, and relapse after initial treatment success.
If carbapenem was the only antimicrobial administered during each episode of UTI, patients were considered to have received carbapenem, and if non-carbapenem was the only antimicrobial administered, patients were considered to have received non-carbapenem. If the antimicrobials administered were switched from carbapenem to non-carbapenem and vice versa during one episode of UTI, patients were considered to have received switch therapy; dividing the patients into three treatment groups.
Additionally, risk factors for UTI caused by ESBL-producing Enterobacteriaceae, proposed by prior studies, such as prior antimicrobials use, history of admission, etc., were compared in each treatment group.
Patients were included in this study if (1) the child was ≤ 18 years old, (2) the axillary body temperature measured in-hospital was > 38℃, (2) colony-counts of bacteria in the urine culture was greater than 105/mL, and (4) pyuria was greater than 10 white blood cells (WBCs) per high power field (HPF). Patients fulfilling all four of these criteria were regarded to have urinary tract infection. Immunocompromised patients and patients who had other symptoms of co-infection that could explain fever were excluded.
Time to defervescence was defined as the time from the start of antimicrobials until the axillary body temperature fell below 38℃ and remained below 38℃. Treatment success was defined at the end of the antimicrobial treatment when all three of the following criteria were satisfied: (1) resolution of fever, (2) negative urine culture, and (3) clearance of pyuria.
Sepsis was defined as the isolation of the same microorganism from blood and uribe. Relapse was defined as the same ESBL-producing bacteria were cultured upon recurred cases. Patients diagnosed with congenital immune deficiency, patients receiving immunosuppressants such as chemotherapy or steroids, and those with neutropenia (absolute neutrophil count < 1000/mm3) were considered immunocompromised. A patient was considered to have vesicoureteral reflux when reflux was confirmed through voiding cystourethrography.
Urine sample collection was obtained through urinary catheterization, suprapubic puncture, and clean catch method. This study was accredited by the Board of Ethics at Seoul National University Hospital (IRB 1209-078-427).
The antimicrobial susceptibility testing was performed by the disc diffusion test as recommended by the Clinical and Laboratory Standards Institute (CLSI) guidelines [17]. The following antimicrobial agents were tested: amikacin, aztreonam, cefepime, cefotaxime, cefotetan, ceftazidime, cefuroxime, cephalothin, ciprofloxacin, gentamicin, imipenem, piperacillin-tazobactam, and tobramycin.
ESBL production confirmatory tests with ceftazidime and cefotaxime were performed by the double-disc synergy test, according to CLSI guidelines [17]. A minimum of 5-mm increase in the zone of diameter of third generation cephalosporins, tested in combination with clavulanic acid versus its zone when tested alone was accepted as an indication of ESBL production [18, 19].
Continuous data were presented as mean [standard deviation (SD)] if data were determined to be normally distributed or median [interquartile range (IQR)] for nonparametric data.
The Chi-square test or Fisher's exact test was used to compare categorical variables and the Mann-Whitney U test or Kruskal-Wallis test was used to assess differences in continuous variables. All P-values were two-tailed and P-values of less than 0.05 were considered statistically significant. SPSS (version 19) software was used for analysis.
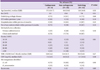
During the study period, ESBL-producing Enterobacteriaceae were cultured from 1,193 urine samples, and of these, 42 episodes in 36 patients without any underlying disease or co-infection to explain fever fit the criteria of UTI. The median age of the patients during the febrile period was 8.4 (39.5) months and 24 male patients (57%) were included in the study. In 27 (64%) cases, 32 different underlying diseases were found, the most common being vesicoureteral reflux (11 cases), hydronephrosis (7 cases), and neurogenic bladder (5 cases). Other underlying diseases included 9 cases of congenital anomaly such as cloacal anomaly. There were 7 cases (17%) of pyuria with WBC 10-19/HPF, 3 cases (7%) with WBC 20-29/HPF, 5 cases (12%) with WBC 30-49/HPF, 11 cases (26%) with WBC 50-99/HPF, 16 cases (38%) with WBC ≥ 100/HPF, and 64% of the cases had pyuria with a WBC count ≥ 50/HPF. A total of 28 cases (67%) were culture positive for E. coli, and in 14 cases (33%) K. pneumoniae was cultured. There were two cases (5%) of UTI accompanied by bacteremia (Table 1).
The following carbapenems were administered: Imipenem in 11 cases (13%), meropenem in 6 cases (7%), and ertapenem in 3 cases (4%). The non-carbapenems used were as follows: cefotaxime in 28 cases (33%), piperacillin-tazobactam in 20 cases (24%), and amikacin in 7 cases (8%).
Four cases (10%) were treated with carbapenem, 23 cases (55%) were treated with non-carbapenem, and 15 cases were treated by switching from one antimicrobial to another. The patients in each treatment group were compared for age (P = 0.52), gender (P = 0.51), underlying urologic disease (P = 0.68), a history of UTI within 1 year (P = 0.10), a history of hospital admission within 6 months (P = 0.22), and a history of antimicrobial administration within 6 months (P = 0.43). There was no statistically significant difference in all these characteristics among the treatment groups (Table 2).
Of the total 42 cases, the median time to defervescence after the initiation of an antimicrobial treatment was 22.9 (20) hours, and upon completion of antimicrobial therapy, there was a 100% treatment success for all 42 cases. In the case of the switching group, because the efficacy of each antimicrobial was hard to assess, only the carbapenem group and the non-carbapenem group were included in the analysis of the treatment outcome and relapse of UTI.
The median age of the carbapenem and non-carbapenem groups was 37.5 (81.7) months, and 8.8 (33.8) months (P = 0.54), respectively. Upon completion of the antimicrobial therapy, both treatment groups showed 100% treatment success, and the median time to defervescence after the initiation of an antimicrobial treatment was 18.0 (6.2) hours for the carbapenem group, and 25.3 (19.7) hours for the non-carbapenem group; showing no statistically significant difference between the two groups (P = 0.28). Patients who received carbapenem did not have relapsed UTI. Among the patients that received non-carbapenem, there was one case (4%) of relapse (Table 3).
In order to see if there was any difference in the treatment outcome based on the in vitro results for susceptibility to the non-carbapenems that were used, the time to defervescence after the initiation of the antimicrobial treatment and the relapse rate were compared between UTIs caused by sensitive strains versus those caused by resistant strains. Only the non-carbapenem group was analyzed because the duration of carbapenem use varied in the switching group.
Of the 23 cases in the non-carbapenem group, 19 cases (83%) were treated with a non-carbapenem to which the cultured bacteria were susceptible.
Four cases (17%) were treated with a non-carbapenem to which cultured bacteria demonstrated resistance through in vitro tests. Contradicting the susceptibility test results, all four of these cases showed complete resolution of symptoms following treatment with a non-carbapenem. The median time to defervescence after the initiation of an antimicrobial treatment was 24.1 (19) hours for the susceptible group, and 35.3 (20.5) hours for the resistant group; showing no statistically significant difference between the two groups (P = 0.40).
On the other hand, of the 19 cases susceptible to non-carbapenems, there was one case (5%) of relapsed UTI, which was statistical insignificant (P = 0.83).
ESBL-producing Enterobacteriaceae is increasingly recognized as the cause of UTIs, and the first choice of treatment for this infection is carbapenem [20]. Considering the increase in the use of carbapenem, there is a great concern about the emergence of carbapenem resistant strains [21-25], especially due to the fact that there are no treatment alternatives for carbapenem resistant strains. This study analyzed 42 episodes of pediatric UTI caused by ESBL-producing Enterobacteriaceae and found no difference in the treatment outcome between patients treated with carbapenem and those treated with non-carbapenem antimicrobials.
There is no established treatment guideline for UTI caused by ESBL-producing Enterobacteriaceae. So far, especially in pediatric patients, there are limited studies comparing the treatment outcome of patients treated with a carbapenem and those treated with a non-carbapenem.
However, when non-carbapenem is used to treat UTI caused by ESBL-producing Enterobacteriaceae, successful treatment outcom could be observed [8, 9]. This can be explained by the higher concentration of antimicrobials, which are excreted into the urinary tract.
In this study, the patients were divided into three groups depending on the type of antimicrobial treatments; carbapenem, non-carbapenem, and switching group. There was a possibility for selection bias in the group that received carbapenem as the initial antimicrobial choice, because generally, patients that have a prior history of UTI caused by ESBL-producing Enterobacteriaceae are given a carbapenem upon relapse. In order to examine such possibility, each treatment group was analyzed and compared for prior history of UTI, prior use of antibiotics, prior admission history, and underlying disease. The results showed no significant difference between the groups. Of the 42 cases included in this study, there were 6 cases of relapsed UTI, and of these, 5 cases were caused by the same bacteria as the initial infection, and there was only one case of relapsed UTI with a different species that produced ESBL. Of the 6 cases of relapsed UTI, only two were treated initially with a carbapenem, and the other four were treated initially with a non-carbapenem regardless of their history of prior UTI caused by ESBL-producing bacteria.
The results showed no significant difference in the treatment outcome, time to defervescence after the initiation of antimicrobials, and relapse rate between the groups that received a carbapenem and those that received a non-carbapenem. As mentioned before, this was most likely because, as the antimicrobial is excreted into the urinary system, a relatively high concentration is maintained. Therefore, although a non-carbapenem was administered to the resistant strains, the relatively high concentration may have led to treatment success, contradicting the antimicrobial susceptibility test results. Combined sepsis may also influence the treatment outcome; therefore, we analyzed this aspect for each group.
When dividing the groups depending on antimicrobial susceptibility, there was no statistically significant difference between the resistant and susceptible groups; although in the non-carbapenem susceptible group, there was one case of relapse. This patient had vesicoureteral reflux and hydronephrosis as underlying diseases, and during the study period, had a relapse of UTI caused by the same ESBL-producing bacteria. This patient also had another episode of UTI caused by a different ESBL-producing bacterium during the study period. Of the two episodes of UTI, the first was initially treated with a non-carbapenem, and the second was treated by switching from a non-carbapenem to a carbapenem. Relapse occurred when using both non-carbapenem and carbapenem antimicrobials, but because the efficacy of the carbapenem in the switching therapy group was hard to evaluate, the relapse was difficult to analyze.
Of the 42 cases of UTI, only two cases were combined with bacteremia; one case was treated with a non-carbapenem, and the other was treated by switching the antimicrobials from non-carbapenem to carbapenem. Both cases had no relapse of UTI. However, the current standard of therapy for ESBL-producing Enterobacteriaceae bacteremia is a carbapenem, whether or not the bacteremia is combined with UTI [26-28].
In this study, the methods of urine sample collection included urinary catheterization, suprapubic puncture, and clean catch method. By diagnosing UTI with our definition and using the exclusion criteria, cases of urine collection by suprapubic puncture were eliminated. In all 42 cases of UTI, urine samples were collected through urinary catheterization and clean catch method.
The small sample size, urine collection by the clean catch method, lack of analysis of the treatment outcome according to ESBL enzymes and minimal inhibitory concentration (MIC) of each antimicrobial, and retrospective analysis are limitations of this study. There is no consensus on the antimicrobial treatment policy for UTI caused by ESBL-producing Enterobacteriaceae. In fact, 19 children in the current study were treated with carbapenem as a monotherapy or as a switch therapy; and whether or not carbapenem is essential needs further investigation. Few studies have so far compared the efficacy of carbapenem and non-carbapenem treatment for pediatric UTI caused by ESBL-producing bacteria; the current data may prove to be useful for further research.
In conclusion, there was no significant difference in the treatment outcome of pediatric UTI caused by ESBL-producing Enterobacteriaceae between patients treated with carbapenem and those treated with non-carbapenem antimicrobials. Considering the importance of pediatric UTI and the increasing emergence of resistant strains, a prospective study with a large sample size is needed.
Figures and Tables
Acknowledgment
This work was supported by the Research Settlement Fund for the new faculty of Seoul National University 2012.
References
1. Zorc JJ, Kiddoo DA, Shaw KN. Diagnosis and management of pediatric urinary tract infections. Clin Microbiol Rev. 2005; 18:417–422.

2. Knothe H, Shah P, Krcmery V, Antal M, Mitsuhashi S. Transferable resistance to cefotaxime, cefoxitin, cefamandole and cefuroxime in clinical isolates of Klebsiella pneumoniae and Serratia marcescens. Infection. 1983; 11:315–317.

3. Bauernfeind A, Hörl G. Novel R-factor borne beta-lactamase of Escherichia coli confering resistance to cephalosporins. Infection. 1987; 15:257–259.

4. Lee J, Pai H, Kim YK, Kim NH, Eun BW, Kang HJ, Park KH, Choi EH, Shin HY, Kim EC, Lee HJ, Ahn HS. Control of extended-spectrum beta-lactamase-producing Escherichia coli and Klebsiella pneumoniae in a children's hospital by changing antimicrobial agent usage policy. J Antimicrob Chemother. 2007; 60:629–637.

5. Briongos-Figuero LS, Gómez-Traveso T, Bachiller-Luque P, Domínguez-Gil González M, Gómez-Nieto A, Palacios-Martín T, González-Sagrado M, Dueñas-Laita A, Pérez-Castrillón JL. Epidemiology, risk factors and comorbidity for urinary tract infections caused by extended-spectrum beta-lactamase (ESBL)-producing enterobacteria. Int J Clin Pract. 2012; 66:891–896.

6. Yamasaki K, Komatsu M, Abe N, Fukuda S, Miyamoto Y, Higuchi T, Ono T, Nishio H, Sueyoshi N, Kida K, Satoh K, Toyokawa M, Nishi I, Sakamoto M, Akagi M, Nakai I, Kofuku T, Orita T, Wada Y, Jikimoto T, Kinoshita S, Miyamoto K, Hirai I, Yamamoto Y. Laboratory surveillance for prospective plasmid-mediated AmpC beta-lactamases in the Kinki region of Japan. J Clin Microbiol. 2010; 48:3267–3273.

7. Titelman E, Iversen A, Kalin M, Giske CG. Efficacy of pivmecillinam for treatment of lower urinary tract infection caused by extended-spectrum beta-lactamase-producing Escherichia coli and Klebsiella pneumoniae. Microb Drug Resist. 2012; 18:189–192.

8. Neuner EA, Sekeres J, Hall GS, van Duin D. Experience with fosfomycin for treatment of urinary tract infections due to multidrug-resistant organisms. Antimicrob Agents Chemother. 2012; 56:5744–5748.

9. Doi A, Shimada T, Harada S, Iwata K, Kamiya T. The efficacy of cefmetazole against pyelonephritis caused by extended-spectrum beta-lactamase-producing Enterobacteriaceae. Int J Infect Dis. 2012; 17:e159–e163.

10. Tinelli M, Cataldo MA, Mantengoli E, Cadeddu C, Cunietti E, Luzzaro F, Rossolini GM, Tacconelli E. Epidemiology and genetic characteristics of extended-spectrum beta-lactamase-producing Gram-negative bacteria causing urinary tract infections in long-term care facilities. J Antimicrob Chemother. 2012; 67:2982–2987.

11. Kizilca O, Siraneci R, Yilmaz A, Hatipoglu N, Ozturk E, Kiyak A, Ozkok D. Risk factors for community-acquired urinary tract infection caused by ESBL-producing bacteria in children. Pediatr Int. 2012; 54:858–862.

12. Azap OK, Arslan H, Serefhanoğlu K, Colakoğlu S, Erdoğan H, Timurkaynak F, Senger SS. Risk factors for extended-spectrum beta-lactamase positivity in uropathogenic Escherichia coli isolated from community-acquired urinary tract infections. Clin Microbiol Infect. 2010; 16:147–151.

13. Topaloglu R, Er I, Dogan BG, Bilginer Y, Ozaltin F, Besbas N, Ozen S, Bakkaloglu A, Gur D. Risk factors in community-acquired urinary tract infections caused by ESBL-producing bacteria in children. Pediatr Nephrol. 2010; 25:919–925.

14. Kim NH, Lee JA, Kim YK, Choi EH, Ha IS, Lee HJ, Choi Y. Risk factors of urinary tract infections due to extended-spectrum beta-lactamase producing Escherichia coli in children. Korean J Pediatr. 2004; 47:164–169.
15. Lee CH, Su LH, Tang YF, Liu JW. Treatment of ESBL-producing Klebsiella pneumoniae bacteraemia with carbapenems or flomoxef: a retrospective study and laboratory analysis of the isolates. J Antimicrob Chemother. 2006; 58:1074–1077.

16. Apisarnthanarak A, Hsu LY, Khawcharoenporn T, Mundy LM. Carbapenem-resistant Gram-negative bacteria: how to prioritize infection prevention and control interventions in resource-limited settings? Expert Rev Anti Infect Ther. 2013; 11:147–157.

17. Clinical and Laboratory Standards Institute. CLSI document M100-S19. Performance standards for antimicrobial susceptibility testing; 19th Informational Supplement. Wayne, PA: Clinical and Laboratory Standards Institute;2009.
18. Jarlier V, Nicolas MH, Fournier G, Philippon A. Extended broad-spectrum beta-lactamases conferring transferable resistance to newer beta-lactam agents in Enterobacteriaceae: hospital prevalence and susceptibility patterns. Rev Infect Dis. 1988; 10:867–878.

19. Thomson KS, Sanders CC. Detection of extended-spectrum beta-lactamases in members of the family Enterobacteriaceae: comparison of the double-disk and three-dimensional tests. Antimicrob Agents Chemother. 1992; 36:1877–1882.

20. Dalgic N, Sancar M, Bayraktar B, Dincer E, Pelit S. Ertapenem for the treatment of urinary tract infections caused by extended-spectrum beta-lactamase-producing bacteria in children. Scand J Infect Dis. 2011; 43:339–343.

21. Nordmann P, Naas T, Poirel L. Global spread of Carbapenemase-producing Enterobacteriaceae. Emerg Infect Dis. 2011; 17:1791–1798.
22. Héritier C, Poirel L, Lambert T, Nordmann P. Contribution of acquired carbapenem-hydrolyzing oxacillinases to carbapenem resistance in Acinetobacter baumannii. Antimicrob Agents Chemother. 2005; 49:3198–3202.

23. Poirel L, Nordmann P. Carbapenem resistance in Acinetobacter baumannii: mechanisms and epidemiology. Clin Microbiol Infect. 2006; 12:826–836.

24. Pai H, Kim J, Kim J, Lee JH, Choe KW, Gotoh N. Carbapenem resistance mechanisms in Pseudomonas aeruginosa clinical isolates. Antimicrob Agents Chemother. 2001; 45:480–484.

25. Shilo S, Assous MV, Lachish T, Kopuit P, Bdolah-Abram T, Yinnon AM, Wiener-Well Y. Risk factors for bacteriuria with carbapenem-resistant Klebsiella pneumoniae and its impact on mortality: a case-control study. Infection. 2013; 41:503–509.

26. Jacoby GA, Munoz-Price LS. The new beta-lactamases. N Engl J Med. 2005; 352:380–391.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download