Abstract
Brain abscesses can be highly lethal if appropriate treatment is not administered, and reports of such an abscess caused by Enterococcus avium are very rare. Here,we report a case of a 48-year-old man presenting with chronic otitis media. He initially presented with a headache and right otalgia. An otoscopic evaluation performed on the day of admission showed exudation of fresh pus from the right ear. Brain magnetic resonance imaging demonstrated a hypodense area in the right temporoparietal lobe, suggestive of a brain abscess. A culturing of the ear discharge and brain abscess aspirate proved of E. avium infection. Following stereotactic aspiration of the brain abscess and proper antimicrobial treatment, the patient recovered completely. In this report, we also review and discuss the available medical literature on previous cases of E. avium infection associated with brain abscess.
Brain abscesses results from a focal suppurative process within the brain parenchyma, and brain abscesses account for 1-8% of all intracranial space-occupying lesions [1]. Brain abscesses remain a potentially fatal infection despite the availability of improved diagnostic imaging modalities and recent advancements in the management of brain abscess, with a 8-25% mortality rate [1, 2].
Enterococci are indigenous to the normal intestinal flora of humans, and most clinical infections are caused by either Enterococcus faecalis or E. faecium [3]. E. avium, formerly known as "group Q streptococcus", is one of the 23 known Enterococcus species and is pathogenic to humans [4, 5]. However, E. avium is rarely associated with brain abscess. Here, we report of a patient presenting with a brain abscess, from which E. avium was isolated as the only pathogen. Additionally, we identified and reviewed the English language articles on similar previous cases published between 1967 and 2012, using the following keywords: "brain abscess", "group Q streptococcus", and "Enterococcus avium".
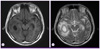
A 48-year-old man with a 13-day history of headache and right otalgia was admitted to our tertiary medical center. He was diagnosed with type 2 diabetes mellitus 3 years earlier and was thereafter treated with oral hypoglycemic agents up until the current presentation. The patient had chronic suppurative otitis media for several years. Physical examination showed that his verbal output was reduced and his neurologic status was 11 on the Glasgow Coma Scale. The patient's temperature was 36.8℃, blood pressure was 140/100 mmHg, and pulse was 80 beats/min. Otoscopic evaluation revealed the exudation of fresh pus from the right ear. Laboratory studies revealed an elevated leukocyte count of 18,500/mm3 and an elevated C-reactive protein level of 18.9 mg/dL. Serological tests were negative for human immunodeficiency virus (HIV), hepatitis B, and hepatitis C. Brain magnetic resonance imaging (MRI) showed the presence of a 3.5-cm, rim-like enhancing lesion in the right temporoparietal lobe with perilesional edema (Fig. 1). Obliteration of the right mastoid air cells with sclerotic changes was noted, and its communication to the right mastoid was suspected. The patient underwent stereotactic aspiration of the brain abscess and treated with parenteral antibiotics, including ceftriaxone (2 g every 12 hours) and metronidazole (500 mg every 6 hours). Elective surgery was scheduled, but a follow-up computed tomography (CT) scan showed significant decreases in the extent of brain abscess due to abscess drainage through the communication site of the right ear. Therefore, the scheduled surgery was cancelled.
On day 6 of hospitalization, E. avium was isolate from ear discharge and aspirates of brain abscess culture. Species identification and antimicrobial susceptibilities of E. avium were determined using the MicroScan Pos Breakpoint Combo Panel Type 28 (Siemens, CA, USA). Ampicillin (2 g every 4 hours) was subsequently administered to the patient. Antibiotic susceptibility testing of the isolates showed that the pathogen was susceptible to penicillin, ampicillin, imipenem, glycopeptides, fluoroquinolones, and high level of aminoglycosides. Parenteral antibiotic therapy consisting of ceftriaxone, metronidazole, and ampicillin was continued for 4 weeks. After parenteral antibiotic therapy, the patient's neurologic deficits improved, and he was discharged in a stable condition with oral antibiotics. Oral antibiotic therapy comprising amoxicillin (500 mg every 8 hour) and levofloxacin (750 mg every 24 hours) was continued for 8 weeks. Compared the images of the initial MRI and the follow-up CT performed 1 month later, the abscess seemed to be completely resolved. Three months after diagnosis, the patient was full recovered without any residual neurologic deficits.
Enterococci are generally regarded as the normal intestinal flora [6]. Over the past 2 decades, however, enterococci have been identified as one group of pathogens responsible for several nosocomial infections; E. faecalis and E. faecium account for up to 90% of the responsible clinical isolates [6, 7]. In a previous study, streptococci were identified as the most common bacteria identified in cultures in patients with brain abscesses, with E. faecalis and E. faecium accounting for only 5% of all isolates [1, 8]. E. avium is rarely reported as a pathogen in humans. Thus far, only 6 cases of brain abscesses caused E. avium have been reported, including those reported in the present study [9-13]. The main characteristics of these cases are summarized in Table 1. To the best of our knowledge, this case report is the first to report a brain abscess caused by E. avium in Korea.
The pathogenic mechanism of brain abscess formation involves either contiguous spread from the focus of infection, hematogenous dissemination to the brain from a distant focus, or head trauma. In most cases, the brain abscess was occured due to contiguous spread from the middle ear, mastoid cells, or paranasal sinuses. Carpenter et al. reported that more than 40% of brain abscesses in adult patients are otogenic in origin [14]. In their study, abscesses were located in the temporal lobe (54% of patients), cerebellum (44%), or both locations (2%). In our case review of brain abscess due to E. avium (Table 1), we found that 5 of 6 patients presented with chronic otitis media, and only 1 patient, who was previously diagnosed with astrocytoma, did not present with otitis media [10]. These findings suggest that brain abscesses caused by E. avium infection are predominantly otogenic in origin. Treatment of brain abscess is.done by.a team approach; adequate abscess drainage and appropriate antimicrobial therapy are most important for proper treatment. In patients with bacterial brain abscess, intravenous antimicrobials have has traditionally been administered for 6.8 weeks [15]. Shorter courses (3.4 weeks) of parenteral therapy may be adequate for patients who have undergone surgical excision of the abscess. In the present case, follow-up CT showed a significant decrease in the extent of brain abscess, owing to abscess drainage through the communication site. Thus, parenteral antibiotic therapy was continued for 4 weeks. Attending physicians need to consider E. avium infection in such cases, so that effective therapy can be initiated as soon as possible.
In 1984, Collins et al. successfully proposed the renaming of "Streptococcus avium" to "Enterococcus avium" due to the findings of various DNA-DNA and DNA-ribosomal RNA studies [5]. Although E. faecalis and E. faecium are the 2 most common species responsible for enterococcal infections, our findings and other reports demonstrate an emerging trend of E. avium infection in humans. Only a few clinical manifestations caused by E. avium have been reported thus far, including bacteremia, endocarditis, osteomyelitis, and splenic abscess [4, 16-18]. Majority of these patients additionally presented with immunocompromising conditions or serious systemic disease. However, only 1 patient with E. avium brain abscess was in an immunocompromised state at diagnosis (Table 1, Case 2). Virulence traits are believed to permeate Enterococcus species to various degrees, thereby enhancing their disease-causing abilities [19]. However, factors that influence the virulence potential of E. avium are not well understood. Recently, Na et al. [4] suggested that E. avium seems to be more virulent than E. gallinarum and E. casseliflavus, but less virulent than E. faecium. Further studies are needed to define the pathogenesis and virulence of E. avium.
Although E. avium is not commonly associated with brain abscesses, it should be considered as an etiological agent in the future, especially in patients diagnosed with chronic otitis media.
Figures and Tables
Figure 1
MRI scan of the brain shows a 3.5-cm, round, rim-like enhancing lesion in the right temporoparietal lobe with perilesional edema. (A) Axial T1-weighted MRI shows a thin, ring-like, hyperintense lesion in the right temporoparietal region, which was presumed to be due to the paramagnetic effects of the abscess capsule. (B) T2-weighted axial MRI shows the hypointense rim of the abscess with a large area of high signal intensity, which is consistent with edema.
References
1. Prasad KN, Mishra AM, Gupta D, Husain N, Husain M, Gupta RK. Analysis of microbialetiology and mortality in patients with brain abscess. J Infect. 2006; 53:221–227.

2. Hakan T, Ceran N, Erdem I, Berkman MZ, Göktaş P. Bacterial brain abscesses: an evaluation of 96 cases. J Infect. 2006; 52:359–366.

3. Koch S, Hufnagel M, Theilacker C, Huebner J. Enterococcal infections: host response, therapeutic, and prophylactic possibilities. Vaccine. 2004; 22:822–830.

4. Na S, Park HJ, Park KH, Cho OH, Chong YP, Kim SH, Lee SO, Sung H, Kim MN, Jeong JY, Kim YS, Woo JH, Choi SH. Enterococcus avium bacteremia: a 12-yearclinicalexperience with 53patients. Eur J Clin Microbiol Infect Dis. 2012; 31:303–310.

5. Patel R, Keating MR, Cockerill FR 3rd, Steckelberg JM. Bacteremia due to Enterococcus avium. Clin Infect Dis. 1993; 17:1006–1011.

6. Prakash VP, Rao SR, Parija SC. Emergence of unusual species of enterococci causing infections, South India. BMC Infect Dis. 2005; 5:14.

8. Tattevin P, Bruneel F, Clair B, Lellouche F, de Broucker T, Chevret S, Bédos JP, Wolff M, Régnier B. Bacterial brain abscesses: a retrospective study of 94 patients admitted to an intensive care unit (1980 to 1999). Am J Med. 2003; 115:143–146.

9. Mohanty S, Dhawan B, Kapil A, Das BK, Pandey P, Gupta A. Brain abscess due to Enterococcus avium. Am J Med Sci. 2005; 329:161–162.
10. Osoba AO, Kutub H, Waliuddin A, Sharab MO. Enterococcus avium. An unusual cause of cerebral abscess. Neurosciences (Riyadh). 2005; 10:297–300.
11. Mohanty S, Kapil A, Das BK, Dhawan B. Enterococcus avium cerebellar abscess. Neurol India. 2006; 54:108–109.
12. Pehlivan Y, Toy MA, Karaoglan I, Namiduru M, Buyukhatipoglu H. Enterococcus avium cerebral abscess. Intern Med. 2007; 46:1280.
13. Escribano JA, Solivera J, Vidal E, Rivin E, Lozano J. Otogenic cerebellar abscess by Enterococcus avium, a very rare infectious agent. J Neurol Surg A Cent Eur Neurosurg. 2013; 02. 20. [Epub ahead of print].
14. Carpenter J, Stapleton S, Holliman R. Retrospective analysis of 49 cases of brain abscess and review of the literature. Eur J Clin Microbiol Infect Dis. 2007; 26:1–11.

15. Mandell , Bennett , Dolin . Principles and Practice of Infectious Diseases. 7th ed. PA: Elsevier;2010. p. 1274.
16. Mirzoyev Z, Anavekar N, Wilson F, Uslan D, Baddour L, Mookadam F. Enterococcus avium endocarditis. Scand J Infect Dis. 2004; 36:876–878.
17. Cottagnoud P, Rossi M. Enterococcus avium osteomyelitis. Clin Microbiol Infect. 1998; 4:290.
18. Farnsworth TA. Enterococcus avium splenic abscess: a rare bird. Lancet Infect Dis. 2002; 2:765.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download