Abstract
Status and emerging issues in the use of praziquantel for treatment of human trematode and cestode infections are briefly reviewed. Since praziquantel was first introduced as a broadspectrum anthelmintic in 1975, innumerable articles describing its successful use in the treatment of the majority of human-infecting trematodes and cestodes have been published. The target trematode and cestode diseases include schistosomiasis, clonorchiasis and opisthorchiasis, paragonimiasis, heterophyidiasis, echinostomiasis, fasciolopsiasis, neodiplostomiasis, gymnophalloidiasis, taeniases, diphyllobothriasis, hymenolepiasis, and cysticercosis. However, Fasciola hepatica and Fasciola gigantica infections are refractory to praziquantel, for which triclabendazole, an alternative drug, is necessary. In addition, larval cestode infections, particularly hydatid disease and sparganosis, are not successfully treated by praziquantel. The precise mechanism of action of praziquantel is still poorly understood. There are also emerging problems with praziquantel treatment, which include the appearance of drug resistance in the treatment of Schistosoma mansoni and possibly Schistosoma japonicum, along with allergic or hypersensitivity reactions against praziquantel treatment. To cope with and overcome these problems, combined use of drugs, i.e., praziquantel and other newly introduced compounds such as triclabendazole, artemisinins, and tribendimidine, is being tried.
The anthelmintic activity of pyrazinoisoquinoline derivatives was first discovered by E. Merck and Bayer AG, Germany, in 1972 [1]. Subsequently, in 1975, among a large number of related compounds, praziquantel, 2-cyclohexylcarbonyl (1,2,3,6,7,11b) hexahydro-4H-pyrazino (2,1-a) isoquinolin-4-one (MW 312.42), was developed as a new broad-spectrum anthelmintic against parasitic trematodes and cestodes [1]. Praziquantel is now produced by various manufacturers around the world, including Shinpoong Pharmaceutical Company (Seoul, Korea), and is used for human and animal platyhelminth infections on a large scale.
Numerous chemotherapeutic trials have been performed to evaluate the clinical use of praziquantel in the treatment of human trematode and cestode infections, and multiple papers reporting successful results have been published. It has been revealed that most of the human-infecting trematode infections, with the exception of fascioliasis (Fasciola hepatica or Fasciola gigantica infection), and most human cestode infections, except larval Echinococcus granulosus or Echinococcus multilocularis infection and sparganosis (caused by the larva of Spirometra erinacei), are treated successfully with recommended drug dosages and regimens, which differ by different types of trematodes and cestodes, in particular, according to the habitat in the host [2, 3].
Despite these numerous clinical reports, the basic pharmacological mechanisms of efficacy of praziquantel against helminth parasites remain poorly understood [4]. In addition, we are faced with several emerging problems that include the appearance of drug resistance in schistosomiasis [5] and possibly in clonorchiasis [6] and the occurrence of allergic and hypersensitivity reactions after praziquantel administration [7, 8]. In this context, the present paper aimed to briefly review the history of praziquantel development and clinical trials, as well as to highlight emerging problems and adverse reactions in the clinical use of praziquantel.
Praziquantel is rapidly taken up through the gut (in humans more than 80% of the orally administered dose is absorbed from the gastrointestinal tract) and reaches its maximal plasma concentration within 1-2 hours [2]. If a person was orally administered 20-50 mg/kg praziquantel, the peak plasma concentration would become 0.2-1.0 µg/mL [2]. The cerebrospinal fluid (CSF) concentration can be 1/7-1/5 of the plasma concentration [1]. Most of the praziquantel absorbed is metabolized in the liver by the cytochrome P450 system and becomes a hydroxylated polar metabolite form which has a lower protein binding capacity (lower helminthotoxic activity) than the unmetabolized form [1, 2]. The excretion of praziquantel occurs mainly through urine (60-80%) as well as bile and feces (15-35%) and is completed within 24 hours [1]. The elimination half-life of praziquantel in the human body is 1-2 hours [2], and after 24 hours, only a trace amount remains in the human body.
The efficacy of praziquantel on the blood, liver, and lung fluke infections is considered to be due to the polarized metabolite form, which constitutes the majority of the praziquantel in the plasma; this form has only slightly lower anthelmintic efficacy compared with its unmetabolized form [1, 2]. The efficacy of praziquantel against cerebral cysticercosis, in which the larval cestode is located in the brain parenchyme or ventricle, is probably due to the passing of the metabolized form of the drug through the blood-brain barrier, despite the drug's overall low concentration in the CSF (only 1/7-1/5 of the plasma concentration) [2].
The effects of praziquantel on helminth parasites have been studied in vitro and in vivo. In vitro studies were first performed on Schistosoma mansoni, Schistosoma japonicum, Dicrocoelium dendriticum, and F. hepatica from 1978-1981 [9-11]. These were followed by studies on Clonorchis sinensis, Metagonimus yokogawai, Opisthorchis viverrini, and Paragonimus westermani in 1983 [12]. The praziquantel concentrations tested were 0 (control), 1, 10, and 100 µg/mL, and the incubation times were 5, 15, 30, and 60 min [10-12]. The most prominent findings observed were rapid contraction of the worm musculature, which led to a loss of worm movement, and rapid bleb formation and vacuolization of the tegument followed by rupture of the blebs and vacuoles [9-12]. Most of these trematode species rapidly took up praziquantel, and vacuolization began to occur within a few minutes after contact with praziquantel [1]. Adult flukes of Fibricola seoulensis (now emended as Neodiplostomum seoulense) exposed in vitro to 0.1-100 µg/mL praziquantel solution for 5, 15, 30, and 60 min also revealed rapid contraction of the musculature and loss of movement with remarkable tegumental and subtegumental changes, in particular, bleb or blister formation followed by rupture and deformation of the tegumental integrity [13].
These in vitro findings induced by praziquantel were confirmed in vivo through studies on worms collected from experimental animals after treatment with praziquantel [11, 12, 14, 15]. Additionally, several unique findings which had not been noted by in vitro studies were reported. With regard to C. sinensis, a large ballon-shaped structural deformity occurred near the anterior end, which resulted in elongation of the distance between the oral and ventral suckers, in worms harvested from experimentally infected rats at day 4 post-treatment, and vacuoles were formed in deep parenchymal organs such as the excretory bladder [14]. Similarly, N. seoulense adults recovered in rats after treatment with praziquantel also showed severe vacuolization of not only the tegumental layer but also deeper parenchymal tissues, as well as narrowing of the intestines [15]. In P. westermani, there was some controversy regarding the in vitro effect of praziquantel. In an earlier study, only a small number of vacuoles were formed in the tegument within 60 min after incubation, suggesting a weak or slow action of praziquantel on this trematode [12]. This was speculated to be due to the extremely thick (18-22 µm) tegument with numerous fortifying fibrils [12]. However, in another study, significant tegumental damage was recognized, accompanied by elongation at the anterior end of the body and vacuolization of the tegument and subtegument at 60 min after exposure to a concentration of 0.1 µg/mL praziquantel [16]. It was further observed in the lung tissues of dogs infected with P. westermani that the worms with damaged tegument were invaded by host granulocytes [17] and eventually the parasite was successfully eliminated [12].
By contrast, no changes were found in the tegument of F. hepatica treated in vitro with praziquantel, possibly because F. hepatica possesses an exceptionally thick outer tegumental layer (up to 20 µm) with many more mitochondria than the other trematodes and its surface is much less elaborately shaped with only small surface pits [10].
The therapeutic efficacy of praziquantel in the treatment of cestode infections was first documented a little earlier than its efficacy on trematodes, in 1976-1977 [18, 19]. However, detailed in vitro effects on the morphological changes of worms were first studied in 1980 on Hymenolepis nana [20] and on Hymenolepis diminuta, Hymenolepis microstoma, E. multilocularis, and Taenia taeniaeformis in 1981 [21]. In H. nana tapeworms, tegumental vacuolization was exclusively observed in the neck region after 5 min incubation in a concentration of 1 µg/mL praziquantel [20]. The vacuolization led to disruption of the syncytial layer in the apical region of the tegument; however, the tegumental microtriches and the surface coat remained unaffected [20]. The same tegumental change was observed in the neck of the adults of the other 4 tapeworm species [21]. The tegument of Diphyllobothrium latum adults (obtained from experimentally infected hamsters) incubated in concentrations higher than 0.1 µg/mL for 4 hours was expanded and desquamated, and finally almost completely stripped off [22]. However, even in these specimens, the scolex and the neck region remained viable and mobile, suggesting the resistance of D. latum to praziquantel in vitro [22]. However, regardless of their in vitro susceptibility, human and animal infections with adult tapeworms were, with no exceptions, successfully treated in vivo with praziquantel. Those infections included H. nana, H. diminuta, H. microstoma, and D. latum [19, 22]. In H. nana and H. diminuta infection in mice and rats, respectively, within 10 min after praziquantel administration, the tapeworms were found apparently paralyzed, and in some cases, their tegument was distended and became dark in color, and in 30 min all the tapeworms were dislodged to the caecum [19]. In H. microstoma infection in mice, the adult worms were paralyzed and no longer attached to the wall of the bile duct from 8 min after the drug administration [19]. In D. latum infection in hamsters, the tapeworms were strongly contracted and were on their way out of the intestine within 30-35 min after the administration of the drug [22].
By contrast, the susceptibility of larval tapeworms appeared to be different by different species of tapeworms. The cysticercoid stages of H. nana, H. diminuta, and H. microstoma were all highly susceptible to praziquantel in infected mice or rats [19]. However, the plerocercoid larvae of D. latum showed no marked changes unless incubated in a very high concentration of 600 µg/mL or more for 24 hours [22]. The protoscolices of E. multilocularis from praziquantel-treated animals were damaged and were not infective to dogs; however, the germinative epithelium of the cyst was not destroyed, and a parasitological cure of the infected animals with hydatid cysts could not be achieved [23]. Therefore, no consideraton should be given to the use of praziquantel in the treatment of hydatid disease in humans [1]. On the other hand, praziquantel was effective against the metacestodes of Taenia species including T. solium and T. multiceps in animal hosts [1]. Praziquantel at a dose of 50 mg/kg/day for 10 days effectively killed cysticerci in porcine muscles, although the cysticerci in the cranial cavity were not killed by this dose [1]. The brain cysticerci in pigs could be killed by either a higher dose (100 mg/kg/day) or a higher duration of treatment (15 days × 50 mg/kg/day) [1].
The exact mechanism of action of praziquantel against trematodes and cestodes remains unclear, although there are some theories [24, 25]. A rapid influx of calcium ion (Ca2+) accompanied by morphological changes of the worm, which include rapid contraction of the musculature and tegumental bleb and vacuole formation, have been among the suggested mechanisms [1, 4]. The beta subunits of voltage-gated Ca2+ channels have been identified as potential molecular targets of praziquantel [26]. Another proposed mechanism is the blocking of the adenosine receptors of the worms by praziquantel, causing calcium influx in the drug's antischistosomal activity [27, 28]. Although not essential for eliciting in vitro effects, host immune cells such as granulocytes, histiocytes, and also antibodies were reported to highly contribute to the in vivo effects of praziquantel in the treatment of tissue-invading helminth infections [2, 28]. In S. mansoni, praziquantel increases the susceptibility of the parasite to be easily attacked by host antibodies by exposing two antigens (27 kDa and 200 kDa proteins) on the surface of the worm [28].
The anti-schistosome efficacy of praziquantel in human patients is generally satisfactory (Table 1), although it is effective mainly on adult fluke infections [1]. A single oral dose of 40 mg/kg, which is useful for mass treatment, is fairly effective, with cure rates of 85.7% for S. japonicum, 79.4-88.6% for S. mansoni, 83.0-88.9% for Schistosoma haematobium, and 75.0% for Schistosoma mekongi [1, 29, 30]. The cure rate can be increased to 99.5% by two doses of 40 mg/kg for S. japonicum [31] and to 80.8% by a single dose of 75 mg/kg for S. mekongi [30]. The rates were also increased to 97.0% and 97.6% by 3 × 20 mg/kg/day for S. mansoni and S. haematobium, respectively [1].
The efficacy of praziquantel for treatment of liver fluke infections (except for F. hepatica and F. gigantica) is similar to that for schistosome infections (Table 1). A single dose of 40 mg/kg is useful for mass treatment, with cure rates of 87.1% for C. sinensis, 90.0% for O. viverrini, and 97.0% for O. felineus [32-34]. Increasing the dose to 3 × 25 mg/kg/day for 1 day or 2 days can increase the cure rate for C. sinensis to 85.7-100% [35]. In O. viverrini infection, a single dose of 75 mg/kg can increase the cure rate to up to 96.6% [30], and a cure rate of 100% was obtained using a regimen of 3 × 25 mg/kg/day for 1 day [36]. However, with regard to F. hepatica and F. gigantica, both a single dose of 40 mg/kg and a regimen of 3 × 25 mg/kg/day for 7 days were not effective, with 0% cure rates [37, 38]. Therefore, another kind of anthelmintic, triclabendazole, has been used for treatment of fascioliasis [39].
For treatment of Paragonimus species (lung flukes) infections, a 2-day regimen with a daily dose of 3 × 25 mg/kg is generally better than a 1-day regimen with the same daily dose (Table 2). For P. westermani, increasing cure rates were reported when comparing 1-day (71.4%) to 2-day (89.5%) and 3-day regimens (100%) [40]. Regarding P. heterotremus, a 2-day regimen was satisfactory to obtain 90-100% cure rates [1], whereas 1-day treatment revealed less satisfactory results, with only a 76.9% cure rate [36]. P. uterobilaterialis and P. ecuadoriensis were more susceptible to praziquantel, showing cure rates of 97.6-100% (P. uterobilaterialis) and 100% (P. ecuadoriensis) with 1-2 day regimens with daily doses of 3 × 25 mg/kg [36, 41]. Because of unsatisfactory results with 1-day treatment with praziquantel, particularly on P. westermani and P. heterotremus, an alternative drug, triclabendazole, has been tried for treatment of human paragonimiasis [39].
Various species of intestinal flukes were also reported to be highly susceptible to praziquantel with 10-40 mg/kg in a single dose (Table 2). F. buski, the largest of all human-infecting intestinal flukes, may be successfully treated with 15-40 mg/kg in a single dose (100% cure rate) [42]. The worms recovered in the stool within 1 day of praziquantel treatment showed small to large blisters on the tegument, and several of them were seen to have ruptured [42]. Therefore, the susceptibility of F. buski to praziquantel is different from that of F. hepatica although the two species are morphologically close to each other. All of the smaller intestinal fluke species ever treated with praziquantel have been found to be highly susceptible to even lower doses, 10-20 mg/kg in a single dose (Table 2). The species tested include heterophyids (M. yokogawai, Heterophyes heterophyes, Heterophyes nocens, and Haplorchis taichui), neodiplostomum (N. seoulense), gymnophallid (Gymnophalloides seoi), and echinostomes (Echinostoma hortense and Acanthoparyphium tyosenense). Even in some species where cure rate was not reported, the drug efficacy seems to be satisfactory because numerous adult flukes were collected after treatment and purging [43-47].
All of the human-infecting adult tapeworm infections are successfully treated with 10-25 mg/kg praziquantel in a single dose (Table 3). T. solium or T. saginata (including T. asiatica) infections are highly susceptible to a low dose (10 mg/kg) of praziquantel with 96-100% cure rates [1, 48, 49 ]. D. latum infections are also successfully treated with 10-25 mg/kg praziquantel with 100% cure rates [22, 49]. However, H. nana infections generally need a higher dose (25 mg/kg) to obtain a satisfactory cure rate [1, 50-52]. This is because of the presence in each individual of concomitant infections with larval stages due to autoinfection, which are more or less resistant to praziquantel (as praziquantel is strong against adult helminths but not against larvae) [53]. To avoid recurrence of hymenolepiasis, a repeated treatment after 14 days is recommended.
Human cysticercosis, caused by the metacestode of T. solium, is the only larval cestode infection that can be successfully treated with praziquantel. A 7-day treatment with a daily dose of 3 × 25 mg/kg brought about highly satisfactory results, although a second treatment with the same regimen was needed in some cases [54]. Alternatively, a 15-day treatment with a daily dose of 50 mg/kg praziquantel in 3 divided doses was also effective for treatment of parenchymal brain cysticercosis [55]. However, several studies have reported better results with replacement of praziquantel with albendazole (7-day course) or a combination of albendazole and praziquantel for treatment of subarachnoid and ventricular cysticercosis [56, 57]. In the treatment of cerebral cysticercosis, administration of corticosteroids such as dexamethasone should accompany the anthelmintic treatment in order to reduce adverse reactions such as headache, vomiting, and neurological symptoms which can occur due to elevated incracranial pressure resulting from inflammatory reactions against antigens liberated from dying cysticerci worms [2]. It is well known that cerebral cysticercosis in the ventricle or subarachnoid space and ocular cysticercosis are refractory to praziquantel or other anthelmintic treatment [2, 57, 58], probably because of the blood-brain barrier or blood-ocular barrier which can interfere with diffusion of the drug into the tissue near the cysticerci. In these cases, surgical removal is the best treatment [57]. In racemose type cysticercosis in the brain, a long course (1 month) of albendazole or combined use of albendazole and praziquantel for 1 month is recommended because complete surgical excision of all cysts in the basal cistern is usually impracticable [57].
The therapeutic efficacy of praziquantel for human sparganosis has been controversial. A human case of subcutaneous sparganosis that was treated two distinct times at an interval of 1 month, with a regimen of 3 × 25 mg/kg × 5 days failed to be free from the infection; 3 spargana survived and were surgically removed 4 months later [59]. In an in vitro experiment, spargana incubated in a concentration of 10 µg/mL praziquantel for 30, 60, 120, and 240 min were severely destroyed throughout their whole body except the scolex and the neck, but when mice were orally infected with these spargana, the parasites appeared to have survived and were able to be successfully recovered (76-100%) from the mice 1 month later [60]. In contrast, patients with pleural or pericardial sparganosis were successfully treated with praziquantel; a regimen of 60-75 mg/kg/day for 3 days seemed to be effective in eliminating the infection [61-63]. It is presumed that praziquantel can significantly damage and destroy the plerocercoid body in vivo, and the lesion (i.e., granuloma size) caused by the worm may become reduced and the patient appears to be successfully treated. However, the spargana may regenerate if their scolex and neck, which show resistance against praziquantel, remain alive [60]. This controversy should be elucidated through further studies.
Human hydatid diseases due to the metacestode (hydatid cyst) of E. granulosus and E. multilocularis are not successfully treated with praziquantel alone [1]. Therapeutic efficacy can be achieved when praziquantel is used in combination with albendazole, particularly as a pre-operative procedure [64, 65]. The regimens for praziquantel and albendazole are 50 mg/kg/day for 1 month and 10-15 mg/kg/day for 1 month, respectively [65].
It is interesting to note that with the use of 60 mg/kg praziquantel (in divided doses) in a community where schistosomiasis (S. japonicum) and soil-transmitted helminthiases (hookworms, Ascaris lumbricoides, and Trichuris trichiura) were co-prevalent, the prevalence of not only schistosomiasis but also hookworm infections (not A. lumbricoides and T. trichiura infections) was decreased from 61.0% to 46.5% at 3 months after treatment [66]. Some activity of praziquantel against muscle proteins of hookworms but not of A. lumbricoides and T. trichiura was suggested [66]; however, this should be elucidated through further studies.
It has been questioned how long it will take for the tissue damage elicited by helminth infections to recover following treatment with praziquantel. In S. mansoni infection in mice, the eggs and worm granulomas in the liver were observed to have regressed to about a half in their original size at 5-12 weeks after praziquantel treatment [67]. However, contradictory results were also reported; eggs and hepatic granulomas were persistent for 1 year after treatment of S. japonicum and S. mansoni with praziquantel [68, 69]. These reports mean that the liver pathology in schistosomiasis already existing at the time of treatment does not resolve quickly and may require quite a long time for recovery. Similarly, in the liver fluke infection, C. sinensis for example, chronic bile duct pathology in the rabbit and in guinea pigs did not recover within 9-12 weeks after praziquantel treatment [70, 71]. On the other hand, in the lung fluke (Paragonimus iloktsuenensis) infection in rats, the lung damage was quickly restored with the disappearance of worms after 4 weeks of praziquantel treatment, although some eggs and collagenation of the lung tissue still remained [72]. Moreover, in an intestinal fluke (N. seoulensis) infection, the intestinal pathology was completely restored in 3 weeks after treatment with praziquantel [73]. In the case of cysticercosis (T. saginata) in cattle, some remnants of cysticerci remained visible at least 20 weeks after treatment with praziquantel [74].
Trials have been done to promote the anthelmintic efficacy of praziquantel. One example is the introduction of sustained-release praziquantel (SRP) tablets [75]. The purpose of this formulation was to compensate for the disadvantage of repeated medication doses to treat, for example, C. sinensis and P. westermani infection. Praziquantel 150 (SRP150) or 300 mg (SRP300) was combined with a high-molecular-weight-matrix, hydroxypropyl methylcellulose (HPMC), and led to be released slowly over 10 hours or more. The results for treatment of C. sinensis infection with 50 mg/kg SRP150 were quite comparable to those obtained with conventional praziquantel in 3 separate doses (30 mg/kg, 3 times) [75]. Another example is a long-acting prevention trial by means of the insertion of praziquantel (105 mg) implants into the subcutaneous tissue of the backs of mice [76]. The praziquantel-implanted mice were challenged repeatedly with S. japonicum cercariae, and the results were encouraging, with nearly no worms, pairing worms, or eggs detected within 2-3 weeks in the mice [76].
It is generally acknowledged that praziquantel is highly effective and safe with no serious adverse reactions. Common adverse reactions are usually mild and include abdominal pain, diarrhea, dizziness, sleepiness, and headache [77]. To avoid these reactions, it is recommended to administer praziquantel before sleep at night. However, in rare instances, praziquantel may cause allergic, anaphylactic, or hypersensitivity reactions in some individuals [7, 8, 78, 79]. A desensitization procedure was performed in a patient with paragonimiasis using small to increasing doses (30, 60, 100, 150, 300, 600, and 1,200 mg) of praziquantel at 90 min intervals, and the patient was then successfully treated with the standard dose of praziquantel (75 mg/kg daily for 3 consecutive days) [7]. In pregnant women, praziquantel treatment at a single dose of 40 mg/kg was found effective and safe for treatment of S. mansoni infection [80, 81].
Possible emergence of strains (or isolates) of S. mansoni and S. japonicum resistant against praziquantel has been documented in the laboratory [82-84]. It was first reported in 1994 that S. mansoni subjected to drug pressure may develop resistance to praziquantel over a course of a few subcurative multiple doses of praziquantel-treated passages in mice [85]. It was also possible to induce resistance of S. mansoni to praziquantel by successive drug treatment of the vector snail, Biomphalaria glabrata, infected with the cercariae [86]. With regard to S. japonicum, a strain from mainland China was able to develop resistance to praziquantel under continuous drug pressure in the laboratory [83, 84].
The presence of praziquantel-resistant field isolates is well known in S. mansoni [84]. Resistance has been repeatedly reported in many endemic foci of S. mansoni, notably in African countries, such as Egypt and Senegal [84, 87, 88]. However, no evidence of tolerance or resistance to praziquantel has been detected in endemic regions of S. japonicum in China [31, 84]. There is no knowledge about development of resistance to praziquantel in S. haematobium, although it was once reported that a repeated standard treatment with praziquantel was ineffective to clear the infection with S. haematobium in 2 patients [89].
In other trematode species, praziquantel resistance has never been documented [90]. One small trial in clonorchiasis patients in Vietnam reported an unusually low cure rate of only 29% following praziquantel treatment with 25 mg/kg daily for 3 days [6]. This low cure rate seems to have been due to the patients receiving a low dose of the medication compared with the standard dose (40 mg/kg in a single dose or 3 × 25 mg/kg/day for 1-2 days) rather than to drug resistance of C. sinensis worms. In cestode infections, a few cases not successfully treated with praziquantel were reported among beef tapeworm (T. saginata) infection cases [91]; however, there was no evidence of drug resistance of the parasite.
Praziquantel is a broad-spectrum, highly efficacious and safe, anthelmintic against trematode and cestode infections in humans and animals. The only limitations for its use in human infections include fascioliasis, hydatid disease, and sparganosis, in which triclabendazole, a combination of praziquantel and albendazole, and surgical removal of parasites, respectively, may be used as an alternative treatment for each infection. Emerging problems include the appearance of praziquantel-resistant strains or isolates in S. mansoni and S. japonicum in the laboratory or in the field. Occurrence in some patients of allergic, hypersensitivity, or anaphylactic reactions to treatment with praziquantel is another emerging problem.
Figures and Tables
Table 1
Recommended regimen and efficacy of praziquantel for treatment of human schistosome and liver fluke infections

Table 2
Recommended regimen and efficacy of praziquantel for treatment of human lung and intestinal fluke infections
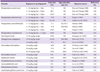
Table 3
Recommended regimen and efficacy of praziquantel for treatment of human adult and larval tapeworm infections

aAn experimental study (Sohn et al., 1993) reported failure to kill spargana treated in vitro in 10 µg/mL praziquantel solution for 4 hours.
bIC, in combination with albendazole (15 mg/kg/day × 28 days) as a preoperative measure.
References
2. Lee SH, Chai JY. Praziquantel in the treatment of trematode and cestode infections. J Korean Soc Chemother. 1985. 3:95–118.
3. Keiser J, Utzinger J. Chemotherapy for major foodborne trematodes: a review. Expert Opin Pharmacother. 2004. 5:1711–1726.

4. Chan JD, Zarowiecki M, Marchant JS. Ca(2+) channels and Praziquantel: A view from the free world. Parasitol Int. 2012. pii: S1383-5769(12)00161-4.

5. Wang W, Wang L, Liang YS. Susceptibility or resistance of praziquantel in human schistosomiasis: a review. Parasitol Res. 2012. 111:1871–1877.

6. Tinga N, De N, Vien HV, Chau L, Toan ND, Kager PA, Vries PJ. Little effect of praziquantel or artemisinin on clonorchiasis in Northern Vietnam. A pilot study. Trop Med Int Health. 1999. 4:814–818.

7. Kyung SY, Cho YK, Kim YJ, Park JW, Jeong SH, Lee JI, Sung YM, Lee SP. A paragonimiasis patient with allergic reaction to praziquantel and resistance to triclabendazole: successful treatment after desensitization to praziquantel. Korean J Parasitol. 2011. 49:73–77.

8. Lee JM, Lim HS, Hong ST. Hypersensitive reaction to praziquantel in a clonorchiasis patient. Korean J Parasitol. 2011. 49:273–275.

9. Pax R, Bennett JL, Fetterer R. A benzodiazepine derivative and praziquantel: effects on musculature of Schistosoma mansoni and Schistosoma japonicum. Naunyn Schmiedebergs Arch Pharmacol. 1978. 304:309–315.

10. Becker B, Mehlhorn H, Andrews P, Thomas H, Eckert J. Light and electron microscopic studies on the effect of praziquantel on Schistosoma mansoni, Dicrocoelium dendriticum, and Fasciola hepatica (Trematoda) in vitro. Z Parasitenkd. 1980. 63:113–128.

11. Mehlhorn H, Becker B, Andrews P, Thomas H, Frenkel JK. In vivo and in vitro experiments on the effects of praziquantel on Schistosoma mansoni. Arzneimittelforschung. 1981. 31:544–554.
12. Mehlhorn H, Kojima S, Rim HJ, Ruenwongsa P, Andrews P, Thomas H, Bunnag B. Ultrastructural investigations on the effects of praziquantel on human trematodes from Asia: Clonorchis sinensis, Metagonimus yokogawai, Opisthorchis viverrini, Paragonimus westermani and Schistosoma japonicum. Arzneimittelforschung. 1983. 33:91–98.
13. Lee SH. In vitro effects of praziquantel on Fibricola seoulensis. Seoul J Med. 1985. 26:41–52.
14. Rim HJ, Park HY, Kim SJ, Lee SH. Morphological observations on Clonorchis sinensis obtained from rats treated with praziquantel. Korean J Parasitol. 1980. 18:192–198.

15. Seo BS, Cha IJ, Chai JY, Hong SJ, Lee SH. Studies on intestinal trematodes in Korea XIX. Light and scanning electron microscopy of Fibricola seoulensis collected from albino rats treated with praziquantel. Korean J Parasitol. 1985. 23:47–57.

16. Lee SH, Park HJ, Hong SJ, Chai JY, Hong ST. In vitro effect of praziquantel on Paragonimus westermani by light and scanning electron microscopic observation. Korean J Parasitol. 1987. 25:24–36.

17. Chiu HS, Kim SJ, Rim HJ. Electron-microscopic studies on the effect of praziquantel to Paragonimus westermani. Korea Univ Med J. 1982. 19:617–630.
18. Hörchner F, Langnes A, Oguz T. Die Wirkung von Mebendazole und Praziquantel auf larvale Taenienstadien bei Maus, Kaninchen und Schwein. Tropenmed Parasitol. 1977. 28:44–50.
19. Thomas H, Gönnert R. The efficay of praziquantel against cestodes in animals. Z Parasitenkd. 1977. 52:117–127.
20. Becker B, Mehlhorn H, Andrews P, Thomas H. Scanning and transmission electron microscope studies on the efficacy of praziquantel on Hymenolepis nana (Cestoda) in vitro. Z Parasitenkd. 1980. 61:121–133.

21. Becker B, Mehlhorn H, Andrews P, Thomas H. Ultrastructural investigations on the effect of praziquantel on the tegument of five species of cestodes. Z Parasitenkd. 1981. 64:257–269.

22. Bylund G, Bång B, Wikgren K. Tests with a new compound (Praziquantel) against Diphyllobothrium latum. J Helminthol. 1977. 51:115–119.
23. Thomas H, Gönnert R. The efficacy of praziquantel against experimental cysticercosis and hydatidosis (author's transl). Z Parasitenkd. 1978. 55:165–179.
24. Geary TG, Woo K, McCarthy JS, Mackenzie CD, Horton J, Prichard RK, de Silva NR, Olliaro PL, Lazdins-Helds JK, Engels DA, Bundy DA. Unresolved issues in anthelmintic pharmacology for helminthiases of humans. Int J Parasitol. 2010. 40:1–13.

25. Vokřál I, Jirásko R, Jedličková V, Bártíková H, Skálová L, Lamka J, Holčapek M, Szotáková B. The inability of tapeworm Hymenolepis diminuta and fluke Dicrocoelium dendriticum to metabolize praziquantel. Vet Parasitol. 2012. 185:168–174.

26. Jeziorski MC, Greenberg RM. Voltage-gated calcium channel subunits from platyhelminths: potential role in praziquantel action. Int J Parasitol. 2006. 36:625–632.

27. Angelucci F, Basso A, Bellelli A, Brunori M, Pica Mattoccia L, Valle C. The anti-schistosomal drug praziquantel is an adenosine antagonist. Parasitology. 2007. 134:1215–1221.

28. Doenhoff MJ, Cioli D, Utzinger J. Praziquantel: mechanisms of action, resistance and new derivatives for schistosomiasis. Curr Opin Infect Dis. 2008. 21:659–667.

29. Coulibaly JT, N'gbesso YK, Knopp S, Keiser J, N'Goran EK, Utzinger J. Efficacy and safety of praziquantel in preschool-aged children in an area co-endemic for Schistosoma mansoni and S. haematobium. PLoS Negl Trop Dis. 2012. 6:e1917.

30. Lovis L, Mak TK, Phongluxa K, Ayé Soukhathammavong P, Vonghachack Y, Keiser J, Vounatsou P, Tanner M, Hatz C, Utzinger J, Odermatt P, Akkhavong K. Efficacy of praziquantel against Schistosoma mekongi and Opisthorchis viverrini: a randomized, single-blinded dose-comparison trial. PLoS Negl Trop Dis. 2012. 6:e1726.

31. Seto EY, Wong BK, Lu D, Zhong B. Human schistosomiasis resistance to praziquantel in China: should we be worried? Am J Trop Med Hyg. 2011. 85:74–82.

32. Lee SH. Large scale treatment of Clonorchis sinensis infections with praziquantel under field conditions. Arzneimittelforschung. 1984. 34:1227–1230.
33. Bunnag D, Harinasuta T. Studies on the chemotherapy of human opisthorchiasis: III. Minimum effective dose of praziquantel. Southeast Asian J Trop Med Public Health. 1981. 12:413–417.
34. Zavoĭkin VD, Zelia OP, Bronshteĭn AM, Sokerina OA, Iarotskiĭ LS, Firsova RA, Mikhaĭlov MM, Gerasimov IV. The procedure for the wide use of praziquantel in a complex of measures to control opisthorchiasis. 1. The tolerance and efficacy of different doses of biltricide during outpatient use in foci. Med Parazitol (Mosk). 1994. (3):24–27.
35. Rim HJ, Yoo KS. Chemotherapeutc effect of praziquantel (Embay 8440) in the treatment of clonorchiasis sinensis. Korea Univ Med J. 1979. 16:459–470.
36. Wegner DH. The profile of the trematodicidal compound praziquantel. Arzneimittelforschung. 1984. 34:1132–1136.
37. Farag HF, Ragab M, Salem A, Saden K. A short note on praziquantel in human fascioliasis. J Trop Med Hyg. 1986. 89:79–80.
38. Farid Z, Kamal M, Mansour N. Praziquantel and Fasciola hepatica infection. Trans R Soc Trop Med Hyg. 1989. 83:813.

39. Keiser J, Engels D, Büscher G, Utzinger J. Triclabendazole for the treatment of fascioliasis and paragonimiasis. Expert Opin Investig Drugs. 2005. 14:1513–1526.

40. Rim HJ, Chang YS. Chemotherapeutic effect of niclofolan and praziquantel in the treatment of paragonimiasis. Korea Univ Med J. 1980. 17:113–128.
41. Udonsi JK. Clinical field trials of praziquantel in pulmonary paragonimiasis due to Paragonimus uterobilateralis in endemic populations of the Igwun Basin, Nigeria. Trop Med Parasitol. 1989. 40:65–68.
42. Bunnag D, Radomyos P, Harinasuta T. Field trial on the treatment of fasciolopsiasis with praziquantel. Southeast Asian J Trop Med Public Health. 1983. 14:216–219.
43. Hong ST, Cho TK, Hong SJ, Chai JY, Lee SH, Seo BS. Fifteen human cases of Fibricola seoulensis infection in Korea. Korean J Parasitol. 1984. 22:61–65.

44. Lee SK, Chung NS, Ko IH, Sohn WM, Hong ST, Chai JY, Lee SH. An epidemiological survey of Echinostoma hortense infection in Chongsong-gun, Kyongbuk Province. Korean J Parasitol. 1988. 26:199–206.

45. Lee SH, Chai JY, Lee HJ, Hong ST, Yu JR, Sohn WM, Kho WG, Choi MH, Lim YJ. High prevalence of Gymnophalloides seoi infection in a village on a southwestern island of the Republic of Korea. Am J Trop Med Hyg. 1994. 51:281–285.

46. Chai JY, Nam HK, Kook J, Lee SH. The first discovery of an endemic focus of Heterophyes nocens (Heterophyidae) infection in Korea. Korean J Parasitol. 1994. 32:157–161.

47. Chai JY, Han ET, Park YK, Guk SM, Lee SH. Acanthoparyphium tyosenense: the discovery of human infection and identification of its source. J Parasitol. 2001. 87:794–800.

48. Rim HJ, Park SB, Lee JS, Joo KH. Therapeutic effects of praziquantel (Embay 8440) against Taenia solium infection. Korean J Parasitol. 1979. 17:67–72.

49. Chai JY, Sohn WM, Hong SJ, Lee SH, Seo BS. Anthelmintic effect of praziquantel (Cestocide@) in the treatment of Taenia saginata and Diphyllobothrium latum infection. J Korean Soc Chemother. 1985. 3:181–184.
50. Schenone H, Galdames M, Rivadeneira A, Morales E, Hoffmann MT, Asalgado N, Meneses G, Mora MV, Cabrera G. Treatment of Hymenolepis nana infection in children by a single oral dose of praziquantel (Embay 8440). Bol Chil Parasitol. 1977. 32:11–13.
51. Rim HJ, Park CY, Lee JS, Joo KH, Lyu KS. Therapeutic effects of praziquantel (Embay 8440) against Hymenolepis nana infection. Korean J Parasitol. 1978. 16:82–87.

52. Schenone H. Praziquantel in the treatment of Hymenolepis nana infection in children. Am J Trop Med Hyg. 1980. 29:320–321.

53. Rim HH. Treatment of Hymenolepis nana infection. Postgrad Dr Asia. 1981. 67–72.
54. Park CY, Joo KH, Rim HJ. Clinical observation on the chemotherapy of cerebral cysticercosis. Korea Univ Med J. 1982. 19:595–616.
55. Sotelo J, Escobedo F, Rodriguez-Carbajal J, Torres B, Rubio-Donnadieu F. Therapy of parenchymal brain cysticercosis with praziquantel. New Eng J Med. 1984. 310:1001–1007.

56. del Brutto OH, Sotelo J. Albendazole therapy for subarachnoid and ventricular cysticercosis. Case report. J Neurosurg. 1990. 72:816–817.
57. Takayanagui OM, Odashima NS, Bonato PS, Lima JE, Lanchote VL. Medical management of neurocysticercosis. Expert Opin Pharmacother. 2011. 12:2845–2856.

58. Santos R, Chavarria M, Aguirre AE. Failure of medical treatment in two cases of intraocular cysticerscosis. Am J Ophthalmol. 1984. 97:249–250.
59. Chai JY, Yu JR, Lee SH, Kim SI, Cho SY. Ineffectiveness of praziquantel treatment for human sparganosis: a case report. Seoul J Med. 1988. 29:397–399.
60. Sohn WM, Hong ST, Chai JY, Lee SH. Infectivity of the sparganum treated by praziquantel, gamma-irradiation and mechanical cutting. Korean J Parasitol. 1993. 31:135–139.

61. Tanaka S, Maruyama H, Ishiwata K, Nawa Y. A case of pleural sparganosis. Parasitol Int. 1997. 46:73–75.
62. Ishii H, Mukae H, Inoue Y, Kadota JI, Kohno S, Uchiyama F, Nawa Y. A rare case of eosinophilic pleuritis due to sparganosis. Intern Med. 2001. 40:783–785.

63. Lee JH, Kim GH, Kim SM, Lee SY, Lee WY, Bae JW, Shin KS, Hwang KK, Kim DW, Cho MC. A case of sparganosis that presented as a recurrent pericardial effusion. Korean Circ J. 2011. 41:38–42.

64. Haralabidis S, Diakou A, Frydas S, Papadopoulos E, Mylonas A, Patsias A, Roilides E, Giannoulis E. Long-term evaluation of patients with hydatidosis treated with albendazole and praziquantel. Int J Immunopathol Pharmacol. 2008. 21:429–435.

65. Tekin R, Kara AF, Tekin RC, Cimen D. Cardiac hydatid cyst case recovered with medical treatment. Anadolu Kardiyol Derg. 2011. 11:650–651.

66. Shaw JG, Aggarwal N, Acosta LP, Jiz MA, Wu HW, Leenstra T, Coutinho HM, Olveda RM, Kurtis JD, McGarvey ST, Friedman JF. Reduction in hookworm infection after praziquantel treatment among children and young adults in Leyte, the Philippines. Am J Trop Med Hyg. 2010. 83:416–421.

67. Mehlhorn H, Frenkel JK, Andrews P, Thomas H. Light and electron microscopic studies on Schistosoma mansoni granulomas of mouse livers following treatment with praziquantel. Tropenmed Parasitol. 1982. 33:229–239.
68. Cheever AW, Deb S. Persistence of hepatic fibrosis and tissue eggs following treatment of Schistosoma japonicum infected mice. Am J Trop Med Hyg. 1989. 40:620–628.

69. Cheever AW, Macedonia JG, Deb S, Cheever EA, Mosimann JE. Persistence of eggs and hepatic fibrosis after treatment of Schistosoma mansoni-infected mice. Am J Trop Med Hyg. 1992. 46:752–758.

70. Lee SH, Chai JY, Yang EC, Yun CK, Hong ST, Lee JB. Observation of liver pathology after praziquantel treatment in experimental Clonorchis sinensis infection in guinea pigs. Seoul J Med. 1988. 29:253–262.
71. Lee SH, Hong ST, Kim CS, Sohn WM, Chai JY, Lee YS. Histopathological changes of the liver after praziquantel treatment in Clonorchis sinensis infected rabbits. Korean J Parasitol. 1987. 25:110–122.

72. Lee SH, Kim SY, Han YC, Lee YS, Hong ST, Sohn WM, Chai JY. Effect of praziquantel treatment on pulmonary lesions of rats infected with Paragonimus iloktsuenensis. Korean J Parasitol. 1989. 27:119–130.

73. Lee SH, Kim BI, Hong ST, Sohn WM, Chai JY. Observation of mucosal pathology after praziquantel treatment in experimental Fibricola seoulensis infection in rats. Korean J Parasitol. 1989. 27:35–40.

74. Gustowska L, Pawlowski Z. Histopathological and histoenzymatic studies on experimental Taenia saginata cysticercosis. Vet Parasitol. 1981. 8:211–218.

75. Hong ST, Lee SH, Lee SJ, Kho WG, Lee M, Chung BS, Seo M, Choi MH. Sustained-release praziquantel tablet: pharmacokinetics and the treatment of clonorchiasis in beagle dogs. Parasitol Res. 2003. 91:316–320.

76. Lei L, Cheng L, Hou J, Guo S, Zhu C, Shi Y, Jiang Y, Lin J. Prevention of Schistosoma japonicum infection in mice with long-acting praziquantel implants. Exp Parasitol. 2012. 131:442–447.

77. Rim HJ. The current pathobiology and chemotherapy of clonorchiasis. Korean J Parasitol. 1986. 24:Suppl. 1–141.

78. Huang SW. A clinical approach to a patient with praziquantel hypersensitivity. J Allergy Clin Immunol. 1992. 90:867.

79. Shen C, Choi MH, Bae YM, Yu G, Wang S, Hong ST. A case of anaphylactic reaction to praziquantel treatment. Am J Trop Med Hyg. 2007. 76:603–605.

80. Adam I, Elwasila ET, Homeida M. Is praziquantel therapy safe during pregnancy? Trans R Soc Trop Med Hyg. 2004. 98:540–543.

81. Adam I, Elwasila E, Homeida M. Praziquantel for the treatment of schistosomiasis mansoni during pregnancy? Ann Trop Med Parasitol. 2005. 99:37–40.

82. Liang YS, Coles GC, Dai JR, Zhu YC, Doenhoff MJ. Adult worm tegumental damage and egg-granulomas in praziquantel-resistant and -susceptible Schistosoma mansoni treated in vivo. J Helminthol. 2002. 76:327–333.

83. Liang YS, Wang W, Dai JR, Li HJ, Tao YH, Zhang JF, Li W, Zhu YC, Coles GC, Doenhoff MJ. Susceptibility to praziquantel of male and female cercariae of praziquantel-resistant and susceptible isolates of Schistosoma mansoni. J Helminthol. 2010. 84:202–207.

84. Wang W, Wang L, Liang YS. Susceptibility or resistance of praziquantel in human schistosomiasis: a review. Parasitol Res. 2012. 111:1871–1877.

85. Fallon PG, Doenhoff MJ. Drug-resistant schistosomiasis: resistance to praziquantel and oxamniquine induced in Schistosoma mansoni in mice is drug specific. Am J Trop Med Hyg. 1994. 51:83–88.

86. Couto FF, Coelho PM, Araújo N, Kusel JR, Katz N, Jannotti-Passos LK, Mattos AC. Schistosoma mansoni: a method for inducing resistance to praziquantel using infected Biomphalaria glabrata snails. Mem Inst Oswaldo Cruz. 2011. 106:153–157.

87. Fallon PG, Sturrock RF, Niang CM, Doenhoff MJ. Short report: diminished susceptibility to praziquantel in a Senegal isolate of Schistosoma mansoni. Am J Trop Med Hyg. 1995. 53:61–62.

88. Ismail M, Metwally A, Parghaly A, Bruce J, Tao LF, Bennett JL. Characterization of isolates of Schistosoma mansoni from Egyptian villages that tolerate high doses of praziquantel. Am J Trop Med Hyg. 1996. 55:214–218.

89. Alonso D, Muñoz J, Gascón J, Valls ME, Corachan M. Failure of standard treatment with praziquantel in two returned travelers with Schistosoma haematobium infection. Am J Trop Med Hyg. 2006. 74:342–344.

90. Keiser J, Utzinger J. The drugs we have and the drugs we need against major helminth infections. Adv Parasitol. 2010. 73:197–230.

91. Lateef M, Zargar SA, Khan AR, Nazir M, Shoukat A. Successful treatment of niclosamide- and praziquantel-resistant beef tapeworm infections with nitazoxanide. Int J Infect Dis. 2008. 12:80–82.

92. Rim HJ, Chu DS, Lee JS, Joo KH, Won CY. Anthelmintic effects of various drugs against metagonimiasis. Korean J Parasitol. 1978. 16:117–122.

93. Lee SH, Chai JY, Hong SJ, Jun YS, Seo BS. Anthelminti effect of praziquantel (Distocide®) against Metagonimus yokogawai infection. J Korean Soc Chemother. 1984. 2:167–171.
94. el-Hawy AM, Safwat M, el-Nasr SS, Abdel Rahman MM. The cure rates of patients infected with heterophyiasis and treated with praziquantel versus niclosamide. J Egypt Soc Parasitol. 1988. 18:437–442.
95. Ata AA, el-Khashab MN, Mourad AA, Soliman HM. The effect of praziquantel on Heterophyes heterophyes, Hymenolepis nana and Fasciola sp. infections. J Egypt Soc Parasitol. 1988. 18:243–246.
96. Pungpak S, Radomyos P, Radomyos B, Schelp FP, Jongsulsuntigul P, Bunnag D. Treatment of Opisthorchis viverrini and intestinal fluke infections with Praziquantel. Southeast Asian J Trop Med Public Health. 1998. 29:246–249.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download