Abstract
Background
Staphylococcus aureus bacteremia (SAB) is the Staphylococcal infections in blood, one of the most common and fatal bacterial infectious diseases worldwide in adults as well as children or neonates. Recently, some studies have yielded inconsistent findings about the association between methicillin-resistance and mortality in patients with SAB. We performed a meta-analysis to assess the impact of methicillin-resistance on mortality in children or neonates with S. aureus bacteremia.
Materials and Methods
We searched using electronic databases such as Ovid-Medline, EMBASE-Medline, and Cochrane Library, as well as five local databases for published studies during the period of 1 January 2000 to 15 September 2011. Two reviewers independently selected articles in accordance with predetermined criteria and extracted prespecified data based on standardized forms. All cohort studies, which compared in-hospital mortality or SAB-related mortality in children and neonates with methicillin-resistant S. aureus (MRSA) infection to those with methicillin-susceptible S. aureus (MSSA), were included. We conducted meta-analysis using the fixed-effect model to obtain pooled estimates of effect.
Results
Of 2,841 screened studies, seven cohort studies were finally selected for analysis. In children or neonates, MRSA bacteremia was associated with a higher mortality compared with MSSA bacteremia (pooled odds ratio [OR] 2.33, P = 0.0008, 95% confidence interval [CI] 1.42 to 3.82, I2 = 0%). Four studies reported SAB-related mortality, the pooled OR of these studies was 2.03 (P = 0.29, 95% CI 0.55 to 7.53, I2 = 0%). A significant increase in mortality associated with methicillin resistance was found in the subgroup analyses of the studies with only neonates (OR: 2.66, 95% CI: 1.46 to 4.85, P = 0.001), prospectively design ones (OR: 3.20, 95% CI: 1.66 to 6.15, P = 0.0005,), the larger studies (OR: 2.89, 95% CI: 1.62 to 5.16, P = 0.0003) and the higher quality studies (OR: 2.76, 95% CI: 1.50 to 5.06, P = 0.001).
Conclusions
MRSA bacteremia is associated with increased mortality compared with MSSA bacteremia in children or neonates. Due to limited studies for mortality in children or neonates with SAB, further research is needed to evaluate the impact of methicillin resistance on mortality in those populations.
Staphylococcus aureus is one of the major causative organisms for community- and hospital-acquired infections as causing invasive diseases, not only in adults but also in neonates and children [1]. Methicillin-resistant S. aureus (MRSA) bacteremia is resistant to beta-lactam antibiotics, limiting the use of antibiotics for treatment, and it is known to cause fetal infections throughout the world.
As well as multidrug-resistant enteric bacteria, MRSA is known to spread healthcare settings rapidly under the in appropriate infection control and cause hospital-acquired infections [2]. Since the late 1990s, MRSA has been increasing in not only hospital-acquired S. aureus infections but also community-acquired infections [3]. For that reason, there has recently been a high level of interest in the development of infection control plans to address this threat.
Compared with methicillin-susceptible S. aureus (MSSA), MRSA is known to cause higher morbidity and mortality and longer hospital stays [4, 5]. These findings, however, were mostly investigated in studies with adult subjects; two meta-analyses with adult subjects reported that MRSA bacteremia significantly increases mortality relative to MSSA bacteremia [6, 7]. Despite increase of bacteremia due to MRSA in neonates and children [8-11], results in those were not consistent across studies [12-15]. In addition, advancements in the treatment for S. aureus bacteremia (SAB) have been made over the past decade, including the development of effective antibiotics and various changes in medical environments, such as the strengthening of hospital infection control systems. Therefore, to better reflect actual circumstances in the current medical environment, we performed a systematic review and meta-analysis to assess the impact of methicillin-resistance on mortality in children and neonates with SAB based on published studies since 2000 that report mortality rates associated with both MRSA and MSSA bacteremia.
We searched for all studies comparing MSSA bacteremia and MRSA bacteremia in terms of their impact on mortality published between January 2000 and September 2011 through Ovid-MEDLINE, EMBASE, and Cochrane library databases in addition to the following 5 local databases: KoreaMed, National Assembly Library (NANET), Korean Studies Information Service System (KISS), Korean Medical Database (KMBASE), and Korea Institute of Science and Technology Information (KISTI) providing information on Korean medical published research. We used the search filter recommended by the Scottish Intercollegiate Guidelines Network (SIGN) to efficiently identify the cohort study design suited the objectives of this study. We applied no language restriction in electronic database search and limited to studies involving humans. We used the common keywords related to Staphylococcus aureus bacteremia and MRSA. The search terms were as follows: "Bacteremia" OR "sepsis" OR "Staphylococcus aureus infection" OR "endocarditis" AND "methicillin-resistant Staphylococcus aureus" OR "MRSA". We also reviewed the bibliographies of relevant articles to identify additional publications. The search terms "neonates" and "children" were not included in the search process. In the last step of the study selection, studies were identified and classified to estimate the number of studies with adult subjects and neonates or children relevant to the aim of this study.
In the first stage of the study selection, irrelevant studies were excluded by reviewing titles and abstracts. The full-text articles were reviewed in the second and third stages of the study selection process. Two authors (DA Park and SM Lee) independently reviewed the articles for eligibility with pre-determined selection criteria, and subsequently resolved any disagreements by discussion together with clinical expert consultation.
The study inclusion criteria were as follows: (1) studies comparing patients with S. aureus bacteremia and S. aureus endoConclusions carditis; (2) studies comparing patients with MRSA bacteremia and MSSA bacteremia; (3) studies comparing mortality rates (all-cause mortality; SAB-related mortality); and (4) studies investigating children (18 years or younger) and neonates. The study exclusion criteria were as follows: (1) not original research; (2) animal studies or pre-clinical studies; (3) not cohort studies; (4) studies published with only an abstract; (5) studies not published in Korean or English; and (6) duplicate reports.
Using a standardized data extraction form two independent reviewers authors (DA Park and SM Lee) extracted pre-specified data: first author, publication year, country, research design, study period, study setting, disease and number of study populations, age and sex of populations between MRSA/MSSA groups, results of outcomes(in-hospital mortality, infection-related mortality). Quality assessment of each included studies was performed independently by two authors using the Newcastle-Ottawa Scale (NOS) [17]. This NOS scale for cohort studies uses a star rating system (range: 0-9 stars) scoring three aspects of the study: selection (0-4), comparability (0-2) and outcomes (0-3). During the data extraction and quality assessment, any disagreements were resolved by discussion.
Meta-analyses were conducted using Review Manager, version 5.0 (RevMan, The Cochrane Collaboration, Oxford, UK. For the dichotomous outcomes such as all-cause mortality, in-hospital mortality, infection-related mortality, we calculated the odds ratio (OR) and 95% confidence interval (CI) using the fixed-effect model. To test for heterogeneity, the forest plot was checked visually, and then statistical heterogeneity was assessed using a Q test (a P < 0.10 was considered significant) and the I2 statistic as a quantitative measure. Statistical heterogeneity was defined as an I2 statistic equal to or greater than 50% [18].
Factors that may have had an effect on outcomes were pre-determined to investigate the cause of heterogeneity between studies, and sub-group analyses were conducted by type of study populations (neonates or children vs. neonates), study design (prospective cohort study vs. retrospective cohort study), the number of study subjects (60 people or fewer vs. above 60 people (as a rule of thumb)) [19], and the number of NOS stars (under 8 stars vs. more than 8 stars).
Publication bias was visually assessed using a funnel plot by plotting the inverse of the standard error against the log odds ratio. To examine for publication bias, the Egger regression asymmetry test [20] and the Begg and Mazumdar adjusted rank correlation test [21] were also conducted using software Stata 10.0 (Stata Corp., College Station, TX, USA).
A P value threshold for statistical significance was set at less than 0.05 for pooled effect estimates.
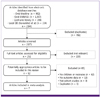
A total of 2,841 studies were identified through the search strategy (Fig. 1). Duplicate studies from each database were eliminated, and then 1,824 studies deemed irrelevant to this study through a review of titles and/or abstracts were excluded. A total of 159 studies were found not to include a comparison of clinical outcomes for MRSA and MSSA in SAB and, therefore, were excluded in the second stage of the study selection process. In the third stage, the authors reviewed the full-text of 92 studies with the inclusion and exclusion criteria. A total of 7 studies [12-15, 22-24] were finally selected after the exclusion of 85 studies for the following reasons: (1) not including children or neonates; (2) unable to extract mortality data; (3) not cohort studies; and (4) duplicate studies.
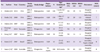
A total of seven cohort studies that enrolled 667 patients (191 for MRSA, 476 for MSSA) were selected and included for the meta-analysis. The population size in each study ranged from 18 to 288. Most of the studies were published since 2005 [12, 13, 15, 22-24]. In terms of study design, there were 5 retrospective cohort studies [12, 13, 15, 22, 24] and 2 prospective cohort studies [14, 23].
Of the 7 studies, 3 had been conducted in the United States [12, 13, 22], 1 in Korea [24], 1 in Tanzania [23], 1 in Israel [15], and 1 in Australia [14]. Except one Korean study [24], the remaining studies were published in English [12-15, 22, 23]. Most of the studies reported in-hospital mortality as the overall mortality rate [12, 14, 15, 22-24]. Kuint et al. [15] reported both all-cause mortality and sepsis-related mortality, and Burke et al. [13] reported only infection-related mortality. The main characteristics of the studies included in this review and meta-analysis are summarized in Table 1.
A total of seven studies were combined in the all-cause mortality analysis with six reporting in-hospital mortality outcomes [12, 14, 15, 22-24] and one reporting infection-related mortality outcome [13]. In the pooled analysis with the fixed-effect model for all-cause mortality, there was no evidence of heterogeneity between-studies (χ2 = 4.40, P = 0.62, I2 = 0%). The pooled OR for the effect of methicillin resistance on mortality was 2.33 (95% CI: 1.42 to 3.82, P = 0.0008), indicating a significant increase for mortality in patients with MRSA bacteremia (Fig. 2).
Among four studies which have reported infection-related mortality [12, 13, 15, 24], except two [12, 24] not reporting SAB-related mortality, remaining two studies [13, 15] were combined in the pooled analysis and showed no heterogeneity between the studies (χ2 = 0.33, P = 0.56, I2 = 0%). The pooled OR for infection-related mortality in patients with MRSA was 2.03 (95% CI: 0.55 to 7.53), indicating the increasing tendency of infection-related mortality for MRSA without a statistically significant difference (P = 0.29) (Fig. 3).
The results of methicillin resistance on mortality are sub-analyzed according to study population, study design, and sample size and the results of quality assessment and presented in Table 2. The pooled OR from the 3 studies [12, 13, 22] that involved both neonates and children was 1.73 (95% CI: 0.71 to 4.22, P = 0.23). From four neonates studies [14, 15, 23, 24], the pooled OR was 2.66 (95% CI: 1.46 to 4.851, P = 0.001) (Fig. 4). In terms of study design, the pooled OR from the 2 prospective cohort studies [14, 23] was 3.20 (95% CI: 1.66 to 6.15, P = 0.0005), whereas the pooled OR from the 5 retrospective ones [12, 13, 15, 22, 24] was 1.60 (95% CI: 0.75 to 3.40, P = 0.22). With regard to sample size, 3 studies [13, 14, 22] involved sample size > 60 people, and 4 studies [12, 15, 23, 24] involved ≤ 60 people; the OR from studies with more than 60 people was 2.89 (95% CI: 1.62 to 5.16, P = 0.0003), and the OR from studies 60 people or fewer was 1.46 (95% CI: 0.58 to 3.67, P = 0.42). There were three studies with NOS of more than 8 stars which showed OR 2.76 (95% CI: 1.50 to 5.06, P = 0.001), whereas four studies with NOS of under 8 stars showed OR 1.66 (95% CI: 0.70 to 3.96, P = 0.25).
No evidence of potential publication bias was noted in the funnel plot, the regression asymmetry test (P = 0.119), or the adjusted rank correlation test (P = 0.23).
This study conducted a systematic review and meta-analysis of cohort studies published since 2000 to quantify the effect of methicillin-resistance on mortality in neonates or children with SAB. The mortality rate was found to be significantly higher in patients with MRSA bacteremia, compared to rate in those with MSSA.
A total of 7 cohort studies were included in the final analysis. The results of the analysis showed a significantly higher mortality risk (OR = 2.33) in neonates or children with MRSA bacteremia than in those with MSSA bacteremia. We considered the possibility that estimating the mean mortality rate of 9.0% (43/476) in the control group with MSSA bacteremia based on the pooled OR could result in an overestimation of the effect size. This difference of the pooled estimate might have been influenced by the result from Isaacs et al.'s study [14], which had the largest sample size among combined studies and of which subjects been enrolled in the 1990's; in consideration of these factors, a sensitivity analysis, excluding the Isaacs et al.'s study, showed that methicillin resistance have not significantly increased the mortality rate (OR: 1.91, 95% CI: 0.97 to 3.77, P = 0.06). Although this sensitivity analysis did not obtain a statistical significance, the direction of effect was consistent with the pooled result of the overall mortality.
In comparison of mortality rate between MRSA bacteremia and MSSA bacteremia in neonates or children, methicillin-resistance is considered to be associated with an increase in mortality risk. This study is the first meta-analysis to investigate the effect of methicillin-resistance on mortality in neonates and children with SAB. The result was comparable to the OR, 1.93 (95% CI: 1.54 to 2.42) in a meta-analysis [7] which have been investigated among adult subjects. Although the pooled analysis for infection-related mortality in four combined studies did not provide a statistically significant result, the direction of effect was in accordance with the hypothesis that methicillin-resistance increases the overall mortality in study population.
The significant association between resistance and mortality risk was found in the subgroup analysis only for neonate subjects, not for mixed population of children and neonates. It might be because the number of studies in mixed population of children and neonate are too small to show the significant result, compared to that in neonate studies. More published studies targeting children are required to show the significant association between methicillin-resistance and increase of mortality in SAB. In subgroups stratified according to study design and sample size, a significant risk of methicillin-resistance for mortality was found in prospectively designed groups, large population groups above 60 and higher quality groups more than 8 stars of NOS.
The lack of a significant difference in some subgroups is due to the small number of included studies, which have resulted in insufficient power to identify the association between methicillin-resistance and risk for mortality in children and neonates with SAB. Out of seven primary studies, only Isaacs et al. [14] demonstrated a significant difference of mortality rates between patients with MRSA and MSSA bacteremia. Remaining six [12, 13, 15, 22-24] did not show any significant difference of those. In a meta-analysis by Cosgrove et al. [7], which investigated adult subjects, although 77.4% of the 31 cohort studies failed to identify the impact of methicillin-resistance on mortality, but the integrated results showed a evident association between MRSA bacteremia and mortality (OR: 1.93, 95% CI: 1.54 to 2.42). Similar to the result of Cosgrove's study, an increase in mortality rate of methicillin resistance was demonstrated in the integrated results of our meta-analysis, even though 85.7% of studies did not demonstrate an increase of mortality.
Although the studies included in this meta-analysis had different subject characteristics, such as neonates vs. children or neonates, no statistical heterogeneity was identified, and bebetween-study statistical heterogeneity was not found in any of the all pooled analyses. (I2 statistic: 0% to 29%). In the meta-analysis by Cosgrove et al. [7], heterogeneity among the studies was quite high (Q test : P = 0.03). In this study, however, the heterogeneity test results were considerably lower than those in the general meta-analysis by Cosgrove et al. This indicates that between-study heterogeneity did not have a major impact on the results. Therefore, a wide distribution of subject characteristics between studies in this meta-analysis is not considered to have had a huge impact on the study results.
Publication bias has been considered to be a particular threat to the validity of meta-analysis of observational studies [25]. However, there was no evidence of publication bias in the current study. According to the Cochrane handbook, tests for funnel plot asymmetry should be used only when there are at least 10 studies included in the meta-analysis, because when there are fewer studies the power of the tests such as the Egger test, and Begg and Mazumdar rank correlation test is too low to distinguish chance from real asymmetry [26]. Therefore, the results of publication bias in this study should be cautiously interpreted, further research is needed to assess evidence to investigate the publication bias clearly.
This study is clinically meaningful in that it was the first study to conduct integrated analysis regarding mortality outcomes of resistance in neonates and children with SAB. Based on studies published since 2000, our meta-analysis results indicated that mortality rate in MRSA group is still higher than that in MSSA group despite advances in medical technology and environmental system. Prior to the year 2000, glycopeptides were the primary treatment option for MRSA infection. Around 2000, however, the FDA approved quinupristin-dalfopristin, linezolid, daptomycin, and tigecycline, broadening treatment choices for MRSA. Hence, MRSA treatment outcomes were expected to improve. As existing studies on the impact of MRSA are based on data collected prior to 2000, this study focused on studies published since 2000 to reevaluate the impact of MRSA in light of the introduction of new antibiotics into clinical practice. However, one limitation of this analysis is that it does not fully reflect the current medical environment, given that some of the primary studies included in this analysis had study periods earlier than 2000.
The more severe condition of MRSA bacteremia patients compared with MSSA bacteremia patients may have accounted for the higher mortality rate, but none of the 7 studies in this analysis conducted multivariable analysis to identify methicillin-resistance as an independent predictive factor for mortality. Hultén et al. [22], however, reported that hospital-acquired S. aureucs infections accounted for mortality in 23 out of 242 patients (9.5%), and at the time of death, all of these subjects had either bacteremia or catheter-associated infection. Among them, 10 (43.5%) had SAB, 6 (26.1%) were premature infants, and 7 (30.4%) were male. Kayange et al. [23] reported that having a positive blood culture test and MRSA are significant related factors that increase mortality in neonates with sepsis. In the study published in Korea, Kang et al. [24] reported that the absence of SAB-related mortality in patients in the neonatal intensive care unit (NICU) was due to empirical antibiotic administration and vancomycin administration in the high-risk group (those with very low birth weight, ventilation therapy, retention of the central venous catheter, and high baseline levels of C-reactive protein).
In conclusion, a significant association was found between methicillin-resistance and higher mortality rate in neonates and children, compared to susceptible one. Based on the integrated results in comparison of mortality rate, MRSA bacteremia is associated with higher mortality risk compared with MSSA bacteremia, and this was consistent in results of subgroups with neonate subjects, prospective cohort studies, studies with large sample sizes and the higher quality studies. Due to limited number of studies for mortality in children and neonates with SAB, it is insufficient to draw the conclusion about mortality risk of methicillin-resistance on outcomes in study population. Hence, further studies are warranted in these areas.
Acknowledgement
This study was supported by a grant of the Korea Healthcare technology R&D Project, Ministry of Health & Welfare, Republic of Korea (A102065).
References
1. Laupland KB, Church DL, Mucenski M, Sutherland LR, Davies HD. Population-based study of the epidemiology of and the risk factors for invasive Staphylococcus aureus infections. J Infect Dis. 2003. 187:1452–1459.

2. Brumfitt W, Hamilton-Miller JM. The worldwide problem of methicillin-resistant Staphylococcus aureus. Drugs Exp Clin Res. 1990. 16:205–214.
3. Naimi TS, LeDell KH, Como-Sabetti K, Borchardt SM, Boxrud DJ, Etienne J, Johnson SK, Vandenesch F, Fridkin S, O'Boyle C, Danila RN, Lynfield R. Comparison of community-and health care-associated methicillin-resistant Staphylococcus aureus infection. JAMA. 2003. 290:2976–2984.

4. Kaech C, Elzi L, Sendi P, Frei R, Laifer G, Bassetti S, Fluckiger U. Course and outcome of Staphylococcus aureus bacteremia: a retrospective analysis of 308 episodes in a Swiss tertiary-care centre. Clin Microbiol Infect. 2006. 12:345–352.

5. Kern WV. Management of Staphylococcus aureus bacteremia and endocarditis: progress and challenges. Curr Opin Infect Dis. 2010. 23:346–358.

6. Whitby M, McLaws ML, Berry G. Risk of death from methicillin-resistant Staphylococcus aureus bacteraemia: a meta-analysis. Med J Aust. 2001. 175:264–267.

7. Cosgrove SE, Sakoulas G, Perencevich EN, Schwaber MJ, Karchmer AW, Carmeli Y. Comparison of mortality associated with methicillin-resistant and methicillin-susceptible Staphylococcus aureus bacteremia: a meta-analysis. Clin Infect Dis. 2003. 36:53–59.

8. Herold BC, Immergluck LC, Maranan MC, Lauderdale DS, Gaskin RE, Boyle-Vavra S, Leitch CD, Daum RS. Community-acquired methicillin-resistant Staphylococcus aureus in children with no identified predisposing risk. JAMA. 1998. 279:593–598.

9. Khairulddin N, Bishop L, Lamagni TL, Sharland M, Duckworth G. Emergence of methicillin resistant Staphylococcus aureus (MRSA) bacteraemia among children in England and Wales, 1990-2001. Arch Dis Child. 2004. 89:378–379.

10. Chuang YY, Huang YC, Lee CY, Lin TY, Lien R, Chou YH. Methicillin-resistant Staphylococcus aureus bacteraemia in neonatal intensive care units: an analysis of 90 episodes. Acta Paediatr. 2004. 93:786–790.

11. Purcell K, Fergie J. Epidemic of community-acquired methicillin-resistant Staphylococcus aureus infections: a 14-year study at Driscoll Children's Hospital. Arch Pediatr Adolesc Med. 2005. 159:980–985.

12. Hakim H, Mylotte JM, Faden H. Morbidity and mortality of Staphylococcal bacteremia in children. Am J Infect Control. 2007. 35:102–105.

13. Burke RE, Halpern MS, Baron EJ, Gutierrez K. Pediatric and neonatal Staphylococcus aureus bacteremia: epidemiology, risk factors, and outcome. Infect Control Hosp Epidemiol. 2009. 30:636–644.

14. Isaacs D, Fraser S, Hogg G, Li HY. Staphylococcus aureus infections in Australasian neonatal nurseries. Arch Dis Child Fetal Neonatal Ed. 2004. 89:F331–F335.
15. Kuint J, Barzilai A, Regev-Yochay G, Rubinstein E, Keller N, Maayan-Metzger A. Comparison of community-acquired methicillin-resistant Staphylococcus aureus bacteremia to other staphylococcal species in a neonatal intensive care unit. Eur J Pediatr. 2007. 166:319–325.

17. Wells GA, Shea B, O'Connell D, Peterson J, Welch V, Losos M, Tugwell P. The Newcastle-Ottawa Scale (NOS) for assessing the quality if nonrandomized studies in meta-analyses. Accessed 20 August 2012. Available at: http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp.
18. Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003. 327:557–560.

19. Hogg RV, Tanis EA. Probability and Statistical Inference. 1988. 3rd ed. New York: Macmillan.
20. Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997. 315:629–634.

21. Begg CB, Manzumdar M. Operating characteristics of a rank correlation test for publication bias. Biometrics. 1994. 50:1088–1101.

22. Hultén KG, Kaplan SL, Lamberth LB, Slimp K, Hammerman WA, Carrillo-Marquez M, Starke JR, Versalovic J, Mason EO Jr. Hospital-acquired Staphylococcus aureus infections at Texas Children's Hospital, 2001-2007. Infect Control Hosp Epidemiol. 2010. 31:183–190.

23. Kayange N, Kamugisha E, Mwizamholya DL, Jeremiah S, Mshana SE. Predictors of positive blood culture and deaths among neonates with suspected neonatal sepsis in a tertiary hospital, Mwanza-Tanzania. BMC Pediatr. 2010. 10:39.
24. Kang HC, Lee KC, Kim SS, Park JO, Kim CH. Staphylococcal infection in the neonatal intensive care unit. J Korean Soc Neonatol. 2007. 14:215–220.
25. Easterbrook PJ, Berlin JA, Gopalan R, Matthews DR. Publication bias in clinical research. Lancet. 1991. 337:867–872.

26. Higgins JPT, Green S. Cochrane handbook for systematic reviews of interventions Version 5.0.2. [Updated September 2009]. 2009. Accessed 20 August 2012. The Cochrane Collaboration;Available at: www.mrc-bsu.cam.ac.uk/cochrane/handbook502/.




 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download