Discussion
In this study, the mortality of bacteremia patients in BICU was 36.0% overall, and it was similar to the mortality of 30.0% in another study conducted in 2011 [
6]. The mean number of day to the occurrence of bacteremia was 17.6 days after burn injury in this study, which was similar to the 16 days that was reported by Vostrugina et al. [
7].
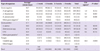
Among the patients admitted to the BICU with burn injuries, gram negative organisms accounted for 59.8% of the causative pathogens for blood stream infections, which was almost twice the proportion of gram positive organisms with 31.3%, and
P. aeruginosa was the most common causative pathogen from the date of admission to the occurrence of bacteremia, regardless of the period. However, existing study results reported that infections by gram positive organisms are predominant in the early period of burn injuries, and those are quickly replaced by gram negative organisms thereafter. Then, with delayed wound closure and an increase in the need for broad-spectrum antibiotics, further replacement of fungi and antibiotic-resistant bacteria takes place [
2]. Other studies showed the same concordant result of this study that
P. aeruginosa was the most common pathogen causing wound infection and bacteremia in the burn center [
1].
A. baumannii was the second most isolated organism, which accounted for 19.0% of all the microorganisms, and it was isolated more frequently in the early stage of the burn injury (mean 14.9 days) and the frequency gradually decreased over time.
Among the gram positive organism,
S. aureus accounted for 14.4% which was the third most common isolate; furthermore,
S. aureus is known to be the major causative pathogen for wound infection and septicemia in other burn center studies, and Gang et al. reported that 74% of septicemic patients were confirmed to have
Staphylococcus species in their blood [
8].
Enterococcus species accounted for 12.3% of all the causative pathogens as the fourth most common isolate. In another study,
Enterococcus species was the causative pathogen for 11% of the bacterial infections among 1,146 burn patients [
9].
Candida species was the fifth most common isolate (48 cases, 8.5%) in this study. The frequency of candida isolates increased with a longer period after the burn injury, and it was confirmed in other studies as well [
10-
11].
C. albicans was the most common isolate with 17 cases followed by
C. parapsilosis (12),
C. tropicalis (11), and
C. glabrata (6). Recent studies reported that
Candida species are the most common fungal isolates in burn patients [
12-
13]. In a study on candidemia in burn patients by Pedrosa et al.,
C. parapsilosis was the second most frequent isolate (25.6% of all fungi) subsequent to
C. albicans in Spanish & Canadian hospitals, and a study from Switzerland reported that
C. glabrata, which accounted for 14% of all cases of candidemia, was the second most frequent isolate [
12]. In the case of burn patients, generally, the rate of candida infections caused by species other than
C. albicans is increasing. Some centers administer fluconazole as a prophylaxis, and the possibility of fluconazole-resistant candida infection is increasing. In this study,
C. glabrata, which is highly resistant to fluconazole, comprised 12.5% of all candida infections, and
C. parapsilosis, which is highly associated with central line infection, was 25.0%. The aggressive nature of treating burn patients such as the use of a central venous line, urine catheter, endotracheal tube, total parenteral nutrition (TPN), prolonged mechanical ventilation, systemic steroid therapy, and broad-spectrum antibiotics increase the risk of fungal infections in burn patients [
12].
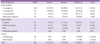
In cases where the presumed primary focus was secondary bacteremia, burn wound had the highest rate of concordant cultures at 37.7% followed by sputum 31.9%, catheter tip 26.0%, and urine 7.5% which was relatively low.
P. aeruginosa bacteremia had a high rate of concordant cultures for the burn wound (79.3%), sputum (58.0%) and catheter tip (37.3%), and candida had a high rate of concordant cultures for the urine (22.9%) and catheter tip (39.6%). Therefore, a primary focus of bacteremia would be easier to assume based on the types of the microorganisms identified from the blood cultures.
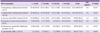
Most of
P. aeruginosa (95.9%) cultured in this study showed resistance to carbapenem. An increase in carbapenem-resistant bacteria has been continuously reported in other studies [
14]. In addition, most of
A. baumannii (95.3%) were carbapenem-resistant bacteria. Those bacteria exhibited high carbapenem resistance even in isolates from less than 1 week after burn injury. The above cases are believed to be due to not keeping the patients isolated from each other in the BICU. There is a high risk of cross contamination of causative pathogens through the skin barrier when 40% or greater of the body's surface area is open to infection in patients. Although completely preventing the occurrence of resistance from cross contamination would be difficult, changing the burn wound dressings in designated places such as a wound dressing room would help to minimize the risk.
Fortunately,
P. aeruginosa and
A. baumannii, which are resistant to colistin, were not found; this finding is identical to the results of another study [
15]. The effectiveness of colistin was shown for the treatment of nosocomial infections caused by multi-drug resistant (MDR)
P. aeruginosa and
A. baumannii [
16], and the use of colistin for severe gram negative infections in the BICU should be prioritized in real practice. The proportion of MRSA was very high accounting for 96.3% of all the
S. aureus, and 56.5% of all the enterococci exhibiting resistance to ampicillin/sulbactam, and 36.2% of
Enterococcus species were VRE. In another study, 28% of enterococcus bacteremia was confirmed to be VRE [
9].
There were limitations in this study. First, we excluded duplicate cases that were defined in other studies [
4,
5], and this exclusion may have caused a distortion in the bacteremia results. Second, it was a retrospective study which was conducted after the patients' data such as the isolated microorganisms from blood cultures were obtained. This may have caused difficulty in finding the rate of at least one or more blood cultures and the rate of regular weekly blood cultures without an exception, among all the admitted patients. Therefore, the representativeness of the study could be reduced. In addition, with this study being a retrospective study, the difficulty in determining the incidence of blood stream infections based on the duration of the ICU stay in the hospital made it difficult to more accurately calculate the statistical data which was another limitation of this study.
In conclusion, gram-negative bacteria such as multi-drug resistant P. aeruginosa and A. baumannii, MRSA, resistant enterococci were isolated at high rates from the early period of the burn injury in severe patients admitted to the BICU; hence, the selection of empirical antibiotics that target those highly antibiotic resistant bacteria should be considered in severe burn patients prior to receiving the results of the microbiological culture test. Specifically, in the early period of the burn injury, de-escalation therapy can be applied where broad-spectrum antibiotics are administered targeting multi-drug resistant gram-negative bacteria and gram-positive bacteria. Then, the antibiotics are changed to narrow spectrum antibiotics based on the test results of the blood cultures. In addition, the use of antifungal agents should be considered by 1 week after the burn injury when the relative frequency of candidemia is high, and the use of empirical antifungal agents should be considered more in patients without any clinical improvement despite the administration of broad-spectrum antibiotics and patients with risk factors of candidemia.






 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download