Abstract
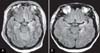
Clinical presentations associated with acute human immunodeficiency virus (HIV) infection are various and nonspecific. Neurologic manifestations may accompany acute HIV infection. Aseptic meningitis has been described in several reports; however, acute encephalitis during acute HIV infection is rare. Some studies have suggested that antiretroviral therapy for treatment of symptomatic acute HIV infection could be beneficial, especially in severe cases. Encephalitis is life-threatening; therefore, early diagnosis and antiretroviral therapy may be needed. We report on a case of encephalitis associated with acute HIV infection. The patient received early antiretroviral therapy and recovered from encephalitis without neurological sequelae.
Figures and Tables
References
2. Gaines H, von Sydow M, Pehrson PO, Lundbegh P. Clinical picture of primary HIV infection presenting as a glandular-fever-like illness. BMJ. 1988. 297:1363–1368.

3. Daar ES, Little S, Pitt J, Santangelo J, Ho P, Harawa N, Kerndt P, Glorgi JV, Bai J, Gaut P, Richman DD, Mandel S, Nichols S. Los Angeles County Primary HIV Infection Recruitment Network. Diagnosis of primary HIV-1 infection. Los Angeles County Primary HIV Infection Recruitment Network. Ann Intern Med. 2001. 134:25–29.
4. Cooper DA, Gold J, Maclean P, Donovan B, Finlayson R, Barnes TG, Michelmore HM, Brooke P, Penny R. Acute AIDS retrovirus infection. Definition of a clinical illness associated with seroconversion. Lancet. 1985. 1:537–540.
5. Carne CA, Tedder RS, Smith A, Sutherland S, Elkington SG, Daly HM, Preston FE, Craske J. Acute encephalopathy coincident with seroconversion for anti-HTLV-III. Lancet. 1985. 2:1206–1208.

6. Nzwalo H, Añón RP, Àguas MJ. Acute encephalitis as initial presentation of primary HIV infection. BMJ Case Rep. 2012. pii: bcr0320125970.

7. Brenner BG, Roger M, Routy JP, Moisi D, Ntemgwa M, Matte C, Baril JG, Thomas R, Rouleau D, Bruneau J, Leblanc R, Legault M, Tremblay C, Charest H, Wainberg MA. High rates of forward transmission events after acute/early HIV-1 infection. J Infect Dis. 2007. 195:951–959.

8. Wawer MJ, Gray RH, Sewankambo NK, Serwadda D, Li X, Laeyendecker O, Kiwanuka N, Kigozi G, Kiddugavu M, Lutalo T, Nalugoda F, Wabwire-Mangen F, Meehan MP, Quinn TC. Rates of HIV-1 transmission per coital act, by stage of HIV-1 infection, in Rakai, Uganda. J Infect Dis. 2005. 191:1403–1409.

9. Bell SK, Little SJ, Rosenberg ES. Clinical management of acute HIV infection: best practice remains unknown. J Infect Dis. 2010. 202:Suppl 2. S278–S288.

10. Boufassa F, Bachmeyer C, Carré N, Deveau C, Persoz A, Jadand C, Séréni D, Bucquet D. SEROCO Study Group. Influence of neurologic manifestations of primary human immunodeficiency virus infection on disease progression. J Infect Dis. 1995. 171:1190–1195.

11. Letendre S, Marquie-Beck J, Capparelli E, Best B, Clifford D, Collier AC, Gelman BB, McArthur JC, McCutchan JA, Morgello S, Simpson D, Grant I, Ellis RJ. CHARTER Group. Validation of the CNS Penetration-Effectiveness rank for quantifying antiretroviral penetration into the central nervous system. Arch Neurol. 2008. 65:65–70.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download